Abstract
Background
Mutations in the BRCA genes confer greater risk of developing breast, ovarian, and prostate cancer. Families carrying the mutation can have intensive surveillance and take preventative measures. This is the first report on the uptake of such interventions in Chinese mutation carriers residing in Asia.
Methods
Breast and ovarian cancer index patients and family members referred for genetic counselling and testing who are found to carry the BRCA mutations were included in this multicenter study.
Results
A total of 31 patients with breast and/or ovarian cancer were found to carry BRCA1 or BRCA2 mutations. Forty-one tested family members also carried the mutations. Of the females, 85.7% of the index patients opted for breast surveillance and 23.8% for prophylactic mastectomy. Of the family members, 82.4% chose breast surveillance and 17.7% had prophylactic mastectomy. The majority of index patients and family members preferred ovarian surveillance (84 and 82.4%). Amongst the index patients, 32% decided for prophylactic salpingo-oophorectomy; 17.6% of the family members who did not have history of ovarian cancer decided to have prophylactic salpingo-oophorectomy. All male index patients agreed to breast and prostate surveillance, including breast clinical examination and PSA monitoring. For those male family members found to be BRCA mutation carriers, 56.3% agreed to have breast surveillance and 66.7% agreed to have prostate surveillance. No index patient or family member agreed to any form of chemoprevention.
Conclusions
Chinese BRCA mutation carriers have a higher uptake of cancer surveillance than prophylactic surgery and have a lack of interest in the use of chemoprevention drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Women who carry a mutation of BRCA1 or BRCA2 gene have an increased lifetime risk of breast cancer as high as 60–80%. Furthermore, the lifetime risk of ovarian cancer has increased to 40% for BRCA1 mutation carriers and 20% for BRCA2 mutation carriers [1–4]. For those who had unilateral breast cancer, risk of contralateral breast cancer also is high compared with women who are not mutation carriers [5]. Men also have an increased risk of breast cancer and more recently are confirmed to have a high risk of prostate cancer: 3.4 to 4.7 times higher than males who are not mutation carriers [6, 7]. With such increased risks, individuals who carry the BRCA mutation can elect for preventative measures, including prophylactic mastectomy [8, 9], salpingo-oopherectomy [10–13], or chemoprevention, such as tamoxifen or raloxifene for breast cancer and oral contraceptive pills for ovarian cancer [14–22]. Alternatively, one can decide for screening that is more intensive and commences earlier than standard screening. For breast cancer, this includes clinical examination, mammographic/ultrasonographic [23], and MRI screening [24–27], and for ovarian cancer, pelvic examination, transvaginal ultrasound, and serial monitoring of tumor marker CA125 [28, 29]. Male individuals also can be screened for prostate cancer, including serial monitoring of PSA [30], and breast screening by clinical examination with or without mammography (NCCN Practice Guidelines in Oncology, v. 1.2009). Although intensive screening cannot prevent cancer, there is an increased likelihood that early detection can result in effective treatment, although its effect on survival has not been established [23, 27]. Similarly there are limited data on the impact of survival using prophylactic surgery, although some studies have suggested its benefits [31].
Genetic testing that results in the option of screening and use of prophylactic measures has been well established and reported in western literatures. There also have been reports on the variation of choice of management for women who are found to carry the BRCA1 or BRCA2 mutation between European countries and the United States [32] due to the different perception of risk, availability of such measures, and cost [32]. Although there have been research-based studies on the prevalence of BRCA mutation in various Asian countries published during the past decade, the availability of clinical testing for BRCA mutation, genetic counseling, and management of these high-risk individuals have not been widely available. There also has been no report of the choice of risk management and uptake of such prophylactic measures for individuals at risk who reside in Asia. This study was designed to be the first to report the uptake of preventative and surveillance measures of Chinese women and men who were found to be carriers of the BRCA1 and BRCA2 mutations.
Materials and methods
Index patients, both male and female, with breast and/or ovarian cancer and their family members, who were referred from 12 government and private-based hospitals and private practitioners, to the Hong Kong Hereditary and High Risk Breast Cancer Programme (www.HRBCP.org) between April 2007 and April 2009 for genetic counseling and tested positive for BRCA1 or BRCA2 mutation were included. All study participants provided written, informed consent for genetic testing and participation of the study. The study has been approved by the ethics committees of all participating centers. All participants underwent standard genetic counseling by a genetic counselor and a breast surgeon with training in cancer genetics. The genetic counseling session included risk assessment of the eligibility of genetic testing based on age of onset of cancer, types of cancer, and family history. The counseling session also included education regarding the genetics of cancer and the likelihood of development of cancer based on western data if the individual is found to be a mutation carrier; advantages and disadvantages of genetic testing, appropriate choice of cancer screening, and prevention strategies and also the implications to the index patient and family members. At the result disclosure session, options of prevention, including screening, prophylactic surgery (mastectomy and salpingo-oophorectomy), and the use of chemopreventative drugs (tamoxifen, raloxifene, oral contraceptive pills) are discussed. When a mutation in the BRCA1 or BRCA2 gene was found in the index patient, testing was offered to their first- and second-degree relatives. Mutation detection was performed using full gene sequencing and multiplex ligation-dependent probe amplification (MLPA). A standard epidemiological questionnaire, including family history was administered. Clinical and medical information of all individuals, including choice of management, were prospectively collected and recorded in the database collection under The Hong Kong Hereditary Breast Cancer Family Registry (www.asiabreastregistry.com). Information about the choice of management was extracted from this prospective database for analysis by genetic counselors and research staff of the registry.
Statistical analyses
Patients’ characteristics and choice of screening and preventive measures were tabulated. The chi-square test was used to compare frequencies of categorical variables. Analyzes of the difference in choice of risk management for breast and/or ovarian or prostate cancer between probands and their family members or patients with and without cancer was performed. Descriptive statistics of choice of screening and prophylactic surgery—prophylactic mastectomy and/or prophylactic salpingo-oophorectomy with stratification by gender and age—was performed. Odd ratios (OR) and 95% confidence intervals (CI) were presented and p values from chi-square statistics (χ2) were estimated from univariate logistic regression using SPSS for Windows Release 16.0 (SPSS Inc., Chicago, IL). Fisher’s exact test was used in the analysis of categorical data where expected counts were <5. Multivariant logistic regression modeling was used to analyze associations between clinical characteristics and risk-reduction strategies undertaken. Statistical significance was set at p < 0.05. Those that are near statistically significant, where p value was set at <0.10, also were included because this may be of interest in our future studies with a larger sample size.
Results
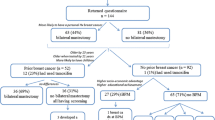
Between April 2007 and April 2009, among all female and male index patients referred for genetic testing, a total of 31 patients with clinically high-risk breast and/or ovarian cancer were found to carry BRCA1 or BRCA2 mutations. Eighty-three family members of these index patients also had genetic testing; 41 were found to carry BRCA1 or BRCA2 mutation. Therefore, there were a total of 72 (31 + 41) participants who were available for analysis in this study. One proband and her family members were lost to follow-up and no details of their management can be obtained. Two family members were still waiting for an appointment to be informed of the genetic result and genetic counseling at the time of analysis. Two family members passed away and therefore risk reduction management was not applicable. The final analysis was performed on 66 (30 + 36) mutation carriers. All individuals were of Chinese origin.
The majority (90.3%) of the index patients were females. All had breast cancer except for one who had ovarian cancer with a family history of breast cancer. The cohort also included three men with breast cancer. A higher percentage of BRCA2 mutation was found (64.5%). 22.6% also had a history of a second cancer, including ovarian, colorectal, prostate, and stomach cancers. Among family members who tested positive, 39% were male, although none of them had a history of cancer. All male index patients with mutations were BRCA2 mutation carriers whereas for family members, 87.5% of them carried BRCA2 mutation and 12.5% carried the BRCA1 mutation. Overall the mean and median age of diagnosis of breast cancer in female index patients were 43 and 39 (range 24–68) and for male index patients was 66 and 60 (range 59–78; Tables 1 and 2).
Table 3 shows the choice of management of the index patients and family members who were found to carry the BRCA mutation. Of the females, excluding those who already had bilateral mastectomy before genetic testing, 85.7% of the index patients opted for breast surveillance, and of these, 94.4% were willing to include MRI breast as part of the screening. For the 23.8% of women who had prophylactic contralateral mastectomy, 14.3% had it performed at the time of diagnosis of the breast cancer, whereas 9.5% had prophylactic contralateral mastectomy performed after a period of surveillance. One was found to have an ipsilateral breast cancer recurrence after breast conservation surgery and decided for ipsilateral completion mastectomy and prophylactic mastectomy; and the other was found to have a suspicious lesion during surveillance and decided for prophylactic contralateral mastectomy without prior biopsy diagnosis. This was confirmed to be atypical ductal hyperplasia. Both of these lesions were only found on MRI breast but not by mammography or ultrasound during screening, although the ipsilateral breast cancer recurrence lesion was seen on a second-look ultrasonography examination. Of the family members, the majority (82.4%) chose breast surveillance as an option; 11.8% who had unilateral breast cancer decided for prophylactic contralateral mastectomy and completion mastectomy if breast conservation was previously performed. One (5.9%) family member who had no history of cancer decided for bilateral prophylactic mastectomy and salpingo-oophorectomy when found to be a BRCA mutation carrier. The mean and median time for prophylactic mastectomy from diagnosis of breast cancer was 58 and 30 months, respectively.
The majority of index patients and family members preferred ovarian surveillance (84 and 82.4 % respectively); 84% of the index patients also agreed to have serial CA125 performed in addition to pelvic examination and transvaginal ultrasound as opposed to female family members who carry the mutation who all agreed to have CA125 monitored. Amongst the index patients who already had breast cancer, 16% decided for prophylactic salpingo-oophorectomy when found to be a mutation carrier. Another 16% of mutation carriers opted for prophylactic salpingo-oophorectomy after a period of surveillance because they were found to have ovarian cysts or presence of uterine fibroid during surveillance. One individual (4%) was diagnosed with ovarian cancer during surveillance. The mean and median time for prophylactic salpingo-oophorectomy from diagnosis of breast cancer was 78 and 84 months respectively.
For the male index patients (three in total), all agreed to breast and prostate surveillance, including breast clinical examination and PSA monitoring. For those male family members who carry the BRCA mutation, 56.3% agreed to have breast surveillance and 66.7% agreed to have prostate surveillance. Apart from index patients who were already or have been on tamoxifen for adjuvant treatment of their breast cancer, no index patient or family members agreed for any form of chemoprevention.
The presence of personal history of cancer significantly affect the choice whether MRI breast is included as part of the surveillance (88.5 vs. 33.3%; p = 0.012). Although not statistically significant (p = 0.109), it is much more likely that a woman would decide for prophylactic contralateral mastectomy and completion mastectomy if she already had history of breast cancer (all eight women who had prophylactic mastectomy except for one had breast cancer, and similarly, all 12 women who had prophylactic salpingo-oophorectomy had history of breast cancer except for one).
There is no significant difference between the age of diagnosis of breast cancer for women who had prophylactic mastectomy compared with those who did not choose to have the surgery (mean age, 37 vs. 42 years; p = 0.349), although those who chose to have prophylactic mastectomy tend to be younger at the age of diagnosis of breast cancer; 85.7% were younger than aged 40 years. Similarly there is no significant difference between age of diagnosis of breast cancer among those who chose to have prophylactic salpingo-oophorectomy compared with those who did not (mean age, 43 vs. 37 years; p = 0.088), although age of diagnosis of breast cancer of those who opted for prophylactic salpingo-oophorectomy tends to be older than 40 years. The mean age for those who had prophylactic mastectomy was slightly younger than those who had salpingo-oophorectomy (43 vs. 48 years). Presence of family history of ovarian cancer increases the rate of uptake of prophylactic salpingo-oophorectomy, but presence of family history of breast cancer did not have the same effect on choice of prophylactic mastectomy (Tables 4 and 5). The cancer pathology, BRCA1 or BRCA2 status, use of oral contraceptive pills and hormone replacement therapy, history of breast feeding, menopausal status, and parity of the women had no impact on the choice of prophylactic surgery or not (data not shown).
Male mutation carriers were more likely to choose to have breast examination (100 vs. 56.3%) and prostate screening (100 vs. 66.7%) in the presence of history of cancer.
Discussion
This study is the first to report the use of intensive surveillance and preventative measures in BRCA1 and BRCA2 mutation carriers in an Asian (Chinese) cohort residing in Asia. From the western literature, women with BRCA mutation confer a high risk of developing breast cancer (BRCA1, 55–95%; BRCA2 33–95%), ovarian cancer (BRCA1 22–66%; BRCA2 4–47%), and prostate cancer (threefold to fivefold increased risk) [6, 16, 33–36]. Compared with sporadic cancers, these related cancers can occur at a younger age and, therefore, affected individuals can be offered the opportunity to have more intensive surveillance or risk-reduction strategies. For breast cancer, the standard recommendation includes annual or biannual clinical breast examination, annual mammography, and MRI of breasts beginning at age 25–35 years [17, 23, 37] and the option of having prophylactic mastectomy [38, 39]. The use of tamoxifen and raloxifene to reduce breast cancer risk also has been promising [15, 18]. For ovarian cancer, annual screening, including pelvic examination, transvaginal ultrasound, and serial CA125 monitoring is recommended, or one has the choice of prophylactic salpingo-oophorectomy [38, 40]. Oral contraceptive pills have been found to have long-lasting protective effect against ovarian cancer [41]. Studies have reported that there is a reduction of breast and ovarian cancer with prophylactic mastectomy and oophorectomy [10, 11]. However, there is still minimal evidence showing that there is survival benefit [16], except for a few studies that showed a reduction in overall mortality and breast and ovarian-specific mortality for women who had prophylactic surgery compared with those who did not [31, 40]. For men the increased risk of prostate cancer in BRCA mutation carriers has warranted screening for prostate cancer in this group of individuals, and in particular BRCA1 mutation carriers. However, most studies have been performed in men of Ashkenazi Jewish origin; further studies need to be performed on other ethnicities [7, 42, 43]. With the reported benefits, genetic testing and risk management have been widely practice in the west. Genetic counseling is important to help decision in the choice of risk management because there are variations in cancer risks between BRCA1 and BRCA2 mutation carriers and also different sensitivities and amount of risk reductions that can be achieved. This includes difference in the sensitivity of screening, such as MRI breast surveillance, where increase in sensitivity is more significant in BRCA1 than BRCA2 mutation carriers and the likelihood of prophylactic salpingo-oophorectomy and tamoxifen being more significant in risk reduction of breast cancer in BRCA2 mutation carriers. In our cohort, however, the choice of prophylactic surgery was not different between BRCA1 and BRCA2 mutation carriers despite having been informed of the different risks between the two types of mutations [26]. Studies have found that the uptake rates of preventative options in BRCA mutation carriers can vary in different countries. One study, which included a number of countries, such as the United States, Canada, and various European countries, found that the uptake rate of prophylactic mastectomy ranges from 4.2–4.5% in Israel and Norway to 36.3% in the United States; uptake rates of prophylactic oophorectomy is usually higher, ranging from 34.9% in Poland to 71% in France and the United States [32, 44]. There also was a variation in the uptake of type of breast screening between countries where mammography is generally an accepted form of screening (65.5 to 100%) but uptake of MRI breast screening ranged from 2.2% in Israel to 94.6% in Holland [32].
Genetic counseling and testing is still a new discipline in Asia. There are a limited number of studies published based on research on prevalence of BRCA mutation and reports of novel mutations in Asian countries [45–50]. However, there have not been any reports of the formal establishment of genetic and high-risk clinics where patients can receive genetic counseling and genetic testing followed by risk management. There is no publication on the uptake rates of risk management of cohorts who carry the BRCA mutation from Asia to date.
The Hong Kong Hereditary and High Risk Programme was established in March 2007 to provide such services to that of international standards by trained specialists in genetics and genetic counselors and to establish a research database on Asian cohorts.
In our study, BRCA mutation carriers are more likely to choose intensive surveillance as an option for risk management. Prophylactic mastectomy rate (including completion mastectomy and contralateral prophylactic mastectomy) was 21.1% overall in all mutation carriers, which is in the mid range compared with that of international studies [32]. Interestingly two of the index patients decided to have contralateral prophylactic mastectomy and ipsilateral completion mastectomy for the individual who had previous breast conservation surgery performed, after a MRI screen detected lesion. One individual was a premenopausal woman diagnosed with ipsilateral breast cancer recurrence after breast conservation surgery who decided for bilateral mastectomy without reconstruction. The other was a postmenopausal woman with right-sided breast cancer with modified radical mastectomy performed who was found to have a MRI-detected breast lesion and decided for mastectomy of the contralateral breast before pathology confirmation preoperatively. The lesion was found to be atypical ductal hyperplasia. The additional information of risk of breast cancer is likely to have altered the choice of management in these high-risk patients. There have been studies in the past on Chinese cohorts suggesting that mastectomy is a preferred option to breast conservation when a woman is diagnosed with breast cancer [51]. There is likely to be cultural [52] differences and risk perception that may have an influence on choice of surgery of Chinese mutation carriers. Educational level also was a factor that influences choice of surgery and reinforces the importance of genetic counseling in the decision-making process [53, 54]. It has been shown that women who choose prophylactic mastectomy tend to be younger [55, 56] and have children [30, 57]. In our cohort, although not statistically significant, the majority of women who agreed to prophylactic mastectomy were younger than age 40 years at diagnosis of breast cancer. Western data have suggested that women with newly diagnosed breast cancer are more likely to choose prophylactic mastectomy if genetic information is known [44]. However, as the majority of patients only received genetic testing after they had cancer surgery, because testing was only offered retrospectively at the start of the program in 2007, most patients were unlikely to agree to prophylactic mastectomy years after their surgery unless this was offered at the time of diagnosis of breast cancer, which is now an option for patients who were counseled through the program. In our study, neither the number of children or parity nor the family history of cancer influenced choice of prophylactic mastectomy, which is different from some reports in the western literature but similar to others [54, 58, 59].
The uptake rate of prophylactic salpingo-oophorectomy was 32%, which is slightly higher than that of prophylactic mastectomy but relatively low compared with most western countries, especially the United States [32]. Similar to published data, however, it is of higher acceptance compared with prophylactic mastectomy [52]. Women who decide for prophylactic salpingo-oophorectomy were comparatively older than those who decided for prophylactic mastectomy. This is similar to western studies where prophylactic salpingo-oophorectomy was more common in carriers older than age 40 years compared with those between 25 and 39 years [60]. This is likely due to the influence of recommendation during genetic counseling where the procedure is generally recommended to be performed after the patient has completed a family and preferably in their 40s. Family history of ovarian cancer has much influence on the decision of prophylactic salpingo-oophorectomy in our cohort. This higher uptake rate of prophylactic salpingo-oophorectomy also is likely to be due to the knowledge of the limitation of sensitivity and specificity of ovarian screening and hence a more aggressive approach of prevention is acceptable [61].
The majority of mutation carriers preferred breast and ovarian surveillance. Although screening has been shown to improve survival in women, and retrospective studies have shown that mammography is able to detect some early-stage cancers in BRCA mutation carriers [16, 62], the improvement of survival from screening in high-risk women has still not been proven [63–66]. More importantly, mammograms are known to be less sensitive for detection of cancer in younger women who have denser breast tissue [67]. Asian women have been reported to have denser breast tissue, and in a previous study we found that >80% of women have heterogeneously dense breasts and are younger when diagnosed with breast cancer in our locality [68, 69]. These findings are similar to other Asian studies [70, 71] and therefore ultrasonography is commonly incorporated as part of breast screening due to the decreased sensitivity of mammography in Asian countries but not replacing mammography [27, 72–74]. MRI breast screening has been shown to be more sensitive than mammography for detecting breast cancer but has lower specificity [75]. Although more studies will be necessary to confirm its use in Asian cohorts who are likely to carry more BRCA2 mutations [76], it has been suggested that the increased sensitivity of MRI is only significant in BRCA1 mutation carriers and not BRCA2 [26]. Most index patients who have been offered MRI breast screening agreed to this type of screening in our cohort, but the acceptance was less in family members who were found to be a mutation carrier. This may be due to the different risk perception in those who have already had cancer. It also may be due to cost of MRI breast screening [77] compared with mammography; further studies are necessary to understand the reason for not choosing MRI breast screening as part of the surveillance screening.
Interestingly no female mutation carriers, excluding those who were already taking tamoxifen, agreed to have any chemoprevention. Although the risk of breast and ovarian cancer may be reduced by chemopreventative drugs, they are not without side effects. Studies have shown that some patients may be more reluctant to take chemopreventative drugs despite the proven effectiveness of the drug, because they are more worried about the side effects and hence are more willing to undergo preventative surgery [78].
In our cohort, uptake of breast and prostate screening is more acceptable in male patients who already had breast cancer. In a previous study in western cohort, although male mutation carriers believe in the risk of breast and prostate cancer, fewer than half of those who have no history of cancer will agree to cancer surveillance. Our cohort uptake of breast screening was 56.3% and prostate cancer screening was 66.7% in male mutation carriers who have no history of cancer, which is higher than published experience [79].
In our study as part of the risk assessment, we did not employ the use of standard risk assessment models developed in the west mainly based on Caucasian and Jewish cohorts [80]. This is because recent studies have found that common risk models used for prediction of BRCA mutation may not be accurate when applied to Asian population [81–83] and hence risk assessment for genetic testing is still based on clinical and family history in our cohort. Without an accurate assessment and estimation of risk of Asian population, it would be hard to evaluate the benefit from these preventative measures and to give accurate genetic counseling for Asian population. Prospective studies on BRCA mutation prevalence and risk in different ethnicities would be essential so that these families are managed appropriately.
The strength of this study is the multi-institutional sources of referral and the systematic prospective collection of data. Additionally, mutation carriers are generally compliant in returning to the high-risk clinic for further management. However, despite The Hong Kong Hereditary Breast Cancer Programme being an organized program, referral is still physician-referral and patient self-referral dependent. There may still be some patients who would receive genetic testing through laboratories in the community and not been given formal genetic counseling and hence the choice of management of those individuals may be different and not reflected in this study. Nevertheless, it is most likely that the majority of individuals tested were through this program, and the results from the study should give a good representation of the choices of management of mutation carriers in Hong Kong.
Weakness of this study includes a rather small cohort of patients because it is only 2 years into the establishment of the program. In addition this study is mainly based in Hong Kong, which is the southern part of China. Although this study is only based in a specific area in Asia, it is likely that the results from this study may reflect the practice in larger cohorts in Asia due to similar cultural background. It will be of interest to compare findings from other Asian countries when available. In addition, the reason and psychological impact of choice of management was not performed in this study. Prophylactic mastectomy can be mutilating and is irreversible, which can affect body image and sexual relationships. Choice of prophylactic surgery can have both negative and positive impact on the life of an individual [79, 84]. Due to the likely variability in different populations in culture, attitudes toward body image, femininity, preventative surgery, and chemopreventative treatment, future research in this area will improve our understanding of factors that influence mutation carriers’ choice to adopt particular risk surveillance and risk-reduction strategies. The costs related to preventative and screening measures may play a role in affecting these choices [56], hence future cost analysis study is important. These and the additional information of risk assessment in Asian population would improve clinician’s risk assessment and counseling and aid individuals on their choice of management so that those who will most likely benefit from these interventions may be appropriately selected.
References
Antoniou A et al (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72(5):1117–1130
King MC, Marks JH, Mandell JB (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645):643–646
Claus EB et al (1996) The genetic attributable risk of breast and ovarian cancer. Cancer 77(11):2318–2324
Ford D et al (1998) Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The breast cancer linkage consortium. Am J Hum Genet 62(3):676–689
Bollet MA et al (2007) Age remains the first prognostic factor for loco-regional breast cancer recurrence in young (<40 years) women treated with breast conserving surgery first. Radiother Oncol 82(3):272–280
Mohamad HB, Apffelstaedt JP (2008) Counseling for male BRCA mutation carriers: a review. Breast 17(5):441–450
Kirchhoff T et al (2004) BRCA mutations and risk of prostate cancer in Ashkenazi Jews. Clin Cancer Res 10(9):2918–2921
Rebbeck TR et al (2004) Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE Study Group. J Clin Oncol 22(6):1055–1062
Meijers-Heijboer H et al (2001) Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 345(3):159–164
Rebbeck TR et al (2002) Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 346(21):1616–1622
Kauff ND et al (2002) Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 346(21):1609–1615
Society of Gynecologic Oncologists Committee (2005) Society of gynecologic oncologists clinical practice committee statement on prophylactic salpingo-oophorectomy. Gynecol Oncol 98(2):179–181
Daly MB (2006) Tamoxifen in ductal carcinoma in situ. Semin Oncol 33(6):647–649
Narod SA et al (2002) Oral contraceptives and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 94(23):1773–1779
Vogel VG (2009) The NSABP study of tamoxifen and raloxifene (STAR) trial. Expert Rev Anticancer Ther 9(1):51–60
Bermejo-Perez MJ, Marquez-Calderon S, Llanos-Mendez A (2007) Effectiveness of preventive interventions in BRCA1/2 gene mutation carriers: a systematic review. Int J Cancer 121(2):225–231
Sakorafas GH (2003) The management of women at high risk for the development of breast cancer: risk estimation and preventative strategies. Cancer Treat Rev 29(2):79–89
Fisher B et al (2005) Tamoxifen for the prevention of breast cancer: current status of the national surgical adjuvant breast and bowel project P-1 study. J Natl Cancer Inst 97(22):1652–1662
Houssami N, Cuzick J, Dixon JM (2006) The prevention, detection, and management of breast cancer. Med J Aust 184(5):230–234
Cummings SR et al (1999) The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple outcomes of raloxifene evaluation. JAMA 281(23):2189–2197
The reduction in risk of ovarian cancer associated with oral-contraceptive use. The cancer and steroid hormone study of the centers for disease control and the national institute of child health and human development. N Engl J Med 316(11):650–655 (1987)
Brown S et al (2009) Initial radiation experience evaluating early tolerance and toxicities in patients undergoing accelerated partial breast irradiation using the contura multi-lumen balloon breast brachytherapy catheter. Brachytherapy 8(2):227–233
Burke W et al (1997) Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer genetics studies consortium. JAMA 277(12):997–1003
Kriege M et al (2004) Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 351(5):427–437
Stoutjesdijk MJ et al (2001) Magnetic resonance imaging and mammography in women with a hereditary risk of breast cancer. J Natl Cancer Inst 93(14):1095–1102
Leach MO et al (2005) Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 365(9473):1769–1778
Warner E et al (2004) Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA 292(11):1317–1325
National Institutes of Health Consensus Development Conference Statement. Ovarian cancer: screening, treatment, and follow-up. Gynecol Oncol 55(3 Pt 2):S4–S14 (1994)
Dorum A et al (1999) Prospectively detected cancer in familial breast/ovarian cancer screening. Acta Obstet Gynecol Scand 78(10):906–911
Wainberg S, Husted J (2004) Utilization of screening and preventive surgery among unaffected carriers of a BRCA1 or BRCA2 gene mutation. Cancer Epidemiol Biomarkers Prev 13(12):1989–1995
Domchek SM et al (2006) Mortality after bilateral salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Lancet Oncol 7(3):223–229
Metcalfe KA et al (2008) International variation in rates of uptake of preventive options in BRCA1 and BRCA2 mutation carriers. Int J Cancer 122(9):2017–2022
Ford D et al (1994) Risks of cancer in BRCA1-mutation carriers. Breast cancer linkage consortium. Lancet 343(8899):692–695
Easton DF et al (1997) Cancer risks in two large breast cancer families linked to BRCA2 on chromosome 13q12-13. Am J Hum Genet 61:120–128
Struewing JP et al (1997) The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 336(20):1401–1408
Hopper JL et al (1999) Population-based estimate of the average age-specific cumulative risk of breast cancer for a defined set of protein-truncating mutations in BRCA1 and BRCA2. Australian breast cancer family study. Cancer Epidemiol Biomarkers Prev 8(9):741–747
Podo F et al (2002) The Italian multi-centre project on evaluation of MRI and other imaging modalities in early detection of breast cancer in subjects at high genetic risk. J Exp Clin Cancer Res 21(3 Suppl):115–124
Kauff ND et al (2008) Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol 26(8):1331–1337
Fatouros M, Baltoyiannis G, Roukos DH (2008) The predominant role of surgery in the prevention and new trends in the surgical treatment of women with BRCA1/2 mutations. Ann Surg Oncol 15(1):21–33
Domchek SM, Stopfer JE, Rebbeck TR (2006) Bilateral risk-reducing oophorectomy in BRCA1 and BRCA2 mutation carriers. J Natl Compr Canc Netw 4(2):177–182
Milsom I, Odlind V (2008) Oral contraceptives give long-lasting protection against ovarian cancer. Use of oral contraceptives can explain reduced incidence of ovarian cancer in Sweden. Lakartidningen 105(10):715–716
Bonn D (2002) Prostate-cancer screening targets men with BRCA mutations. Lancet Oncol 3(12):714
Giri VN et al (2007) Prostate cancer risk assessment program: a 10-year update of cancer detection. J Urol 178(5):1920–1924
Basu SK et al (2008) Unilateral and bilateral breast cancer in women surviving pediatric Hodgkin’s disease. Int J Radiat Oncol Biol Phys 72(1):34–40
Kwong A et al (2008) Characterization of the pathogenic mechanism of a novel BRCA2 variant in a Chinese family. Fam Cancer 7(2):125–133
Lim YK et al (2007) Identification of novel BRCA large genomic rearrangements in Singapore Asian breast and ovarian patients with cancer. Clin Genet 71(4):331–342
Song CG et al (2006) BRCA1 and BRCA2 gene mutations of familial breast cancer from Shanghai in China. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 23(1):27–31
Law TT et al (2009) Telephone pre-anaesthesia assessment for ambulatory breast surgery. Hong Kong Med J 15(3):179–182
Kriege M et al (2006) Differences between first and subsequent rounds of the MRISC breast cancer screening program for women with a familial or genetic predisposition. Cancer 106(11):2318–2326
Choi DH et al (2004) Incidence of BRCA1 and BRCA2 mutations in young Korean breast cancer patients. J Clin Oncol 22(9):1638–1645
Gomez SL, France AM, Lee MM (2004) Socioeconomic status, immigration/acculturation, and ethnic variations in breast conserving surgery, San Francisco Bay area. Ethn Dis 14(1):134–140
Julian-Reynier CM et al (2001) Women’s attitudes toward preventive strategies for hereditary breast or ovarian carcinoma differ from one country to another: differences among English, French, and Canadian women. Cancer 92(4):959–968
Suen D, Chow L, Kwong A (2008) Breast-conserving surgery in Hong Kong Chinese women. World J Surg 32(12):2549–2553
Litton JK et al (2009) Perception of screening and risk reduction surgeries in patients tested for a BRCA deleterious mutation. Cancer 115(8):1598–1604
Scheuer L et al (2002) Outcome of preventive surgery and screening for breast and ovarian cancer in BRCA mutation carriers. J Clin Oncol 20(5):1260–1268
Meijers-Heijboer EJ et al (2000) Presymptomatic DNA testing and prophylactic surgery in families with a BRCA1 or BRCA2 mutation. Lancet 355(9220):2015–2020
Lodder LN et al (2002) One year follow-up of women opting for presymptomatic testing for BRCA1 and BRCA2: emotional impact of the test outcome and decisions on risk management (surveillance or prophylactic surgery). Breast Cancer Res Treat 73(2):97–112
Uyei A et al (2006) Association between clinical characteristics and risk-reduction interventions in women who underwent BRCA1 and BRCA2 testing: a single-institution study. Cancer 107(12):2745–2751
Ray JA, Loescher LJ, Brewer M (2005) Risk-reduction surgery decisions in high-risk women seen for genetic counseling. J Genet Couns 14(6):473–484
Botkin JR et al (2003) Genetic testing for a BRCA1 mutation: prophylactic surgery and screening behavior in women 2 years post testing. Am J Med Genet A 118A(3):201–209
Stirling D et al (2005) Screening for familial ovarian cancer: failure of current protocols to detect ovarian cancer at an early stage according to the international Federation of gynecology and obstetrics system. J Clin Oncol 23(24):5588–5596
Brekelmans CT et al (2001) Effectiveness of breast cancer surveillance in BRCA1/2 gene mutation carriers and women with high familial risk. J Clin Oncol 19(4):924–930
Liberman L (2004) Breast cancer screening with MRI–what are the data for patients at high risk? N Engl J Med 351(5):497–500
Tabar L et al (2004) Number needed to screen: lives saved over 20 years of follow-up in mammographic screening. J Med Screen 11(3):126–129
Warner E, Causer PA (2005) MRI surveillance for hereditary breast-cancer risk. Lancet 365(9473):1747–1749
Robson ME, Offit K (2004) Breast MRI for women with hereditary cancer risk. JAMA 292(11):1368–1370
Kerlikowske K, Brown JS, Grady DG (1992) Should women with familial ovarian cancer undergo prophylactic oophorectomy? Obstet Gynecol 80(4):700–707
Kwong A et al (2008) Breast cancer in Chinese women younger than age 40: are they different from their older counterparts? World J Surg 32:2554–2561
Kwong A et al (2008) The acceptance and feasibility of breast cancer screening in the East. Breast 17(1):42–50
Nagata C et al (2005) Mammographic density and the risk of breast cancer in Japanese women. Br J Cancer 92(12):2102–2106
Ursin G et al (1999) Breast cancer and oral contraceptive use in Asian-American women. Am J Epidemiol 150(6):561–567
Haars G et al (2005) Measurements of breast density: no ratio for a ratio. Cancer Epidemiol Biomarkers Prev 14(11 Pt 1):2634–2640
Buist DS et al (2004) Factors contributing to mammography failure in women aged 40–49 years. J Natl Cancer Inst 96(19):1432–1440
Kuhl CK et al (2005) Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol 23(33):8469–8476
Shah SK, Shah SK, Greatrex KV (2005) Current role of magnetic resonance imaging in breast imaging: a primer for the primary care physician. J Am Board Fam Pract 18(6):478–490
Kwong A et al (2009) A BRCA2 founder mutation and seven novel deleterious BRCA mutations in southern Chinese women with breast and ovarian cancer. Breast Cancer Res Treat 117:683–686
Plevritis SK et al (2006) Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA 295(20):2374–2384
Metcalfe KA et al (2005) The use of preventive measures among healthy women who carry a BRCA1 or BRCA2 mutation. Fam Cancer 4(2):97–103
Foster C et al (2007) Predictive genetic testing for BRCA1/2 in a UK clinical cohort: three-year follow-up. Br J Cancer 96(5):718–724
Parmigiani G, Berry D, Aguilar O (1998) Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet 62(1):145–158
Kurian AW, Gong GD, Chun NM et al (2008) Performance of BRCA1/2 mutation prediction models in Asian Americans. J Clin Oncol 26(29):4752–4758
Thirthagiri E et al (2008) Evaluation of BRCA1 and BRCA2 mutations and risk-prediction models in a typical Asian country (Malaysia) with a relatively low incidence of breast cancer. Breast Cancer Res 10(4):R59
Rao NY, Hu Z, Yu YM et al (2008) Evaluating the performance of models for predicting the BRCA germline mutations in Han Chinese familial breast cancer patients. Breast Cancer Res Treat 116(3):563–570
Brandberg Y et al (2008) Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol 26(24):3943–3949
Acknowledgments
The authors thank Dr. Ellen Li Charitable Foundation, Kerry Group Kuok Foundation Limited, and The Hong Kong Cancer Fund for their continual support of the work of the Hong Kong Hereditary and High Risk Breast Cancer Programme and Hong Kong Hereditary Breast Cancer Family Registry; Professor Jim M. Ford and Professor Dee West, Stanford University for their continual guidance; Dr. Annie Chu and Miss Elaine Tsui for assisting with the update of the registry database; and Dr. Edmond S.K. Ma, Dr. Chris L.P. Wong, Dr. W.K. Chan, and Dr. Fian Law and the team at the Department of Molecular Pathology, Hong Kong Sanatorium and Hospital for contributing to the laboratory work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kwong, A., Wong, C.H.N., Shea, C. et al. Choice of Management of Southern Chinese BRCA Mutation Carriers. World J Surg 34, 1416–1426 (2010). https://doi.org/10.1007/s00268-010-0477-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0477-5