Abstract
Background
Inflammatory myofibroblastic tumor (IMT) is a rare condition. The aim of the present study was to evaluate the clinical characteristics and surgical outcomes for IMT of the liver in our large cohort of patients.
Methods
From January 2001 to December 2007, all patients with a pathological diagnosis of IMT of the liver who underwent partial hepatectomy were retrospectively analyzed.
Results
During the study period, 64 patients underwent partial hepatectomy for IMT of the liver in our tertiary referral center. The commonest clinical presentation was abdominal pain (53%), followed by fever (41%); 15.6% of patients were asymptomatic. Preoperative diagnosis of IMT was suspected in only five patients (8%). The indications for surgery included suspicion of malignancy (60.9%), uncertain diagnosis (40.6%), symptomatic disease (26.6%), and spontaneous rupture (3.1%). The postoperative complication rate was low (17.2%). There was no hospital mortality. After a median follow-up of 30 months, no patient developed recurrence.
Conclusions
Although there are various treatment options for IMT of the liver, surgical resection for good risk patients is preferred.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory myofibroblastic tumor (IMT) is a rare condition. There are a variety of synonyms for this tumor including plasma cell granuloma, postinflammatory tumor, xanthomatous pseudotumor, inflammatory pseudotumor, and inflammatory fibrosarcoma [1]. By definition, the tumor is composed of dominant spindle cell proliferation with a variable inflammatory component. These spindle cells are now known to be myofibroblasts, and this is the reason for the current designation for this disease. Inflammatory myofibroblastic tumor may affect individuals of any age, but it has a predilection for children and young adults. It is most commonly found in the lung, but is also reported in the central nervous system, salivary glands, larynx, breast, pancreas, spleen, lymph nodes, skin, and liver [2, 3]. As the synonyms suggest, there has been some confusion as to whether IMT is truly neoplastic or whether it represents a reactive proliferation of myofibroblastic cells. It is now generally accepted that IMT is a true neoplasm. These lesions have a benign behavior, but the possibility of malignant transformation exists [4, 5]. The present study was designed to evaluate the clinical characteristics and surgical outcome based on the largest series of IMT of the liver in the medical literature.
Materials and methods
From January 2001 to December 2007, all patients with a pathological diagnosis of IMT of the liver who underwent partial hepatectomy at the Eastern Hepatobiliary Surgery Hospital (Shanghai, China) were retrospectively analyzed. The prospectively maintained database and medical records were reviewed for demographics, characteristics of the tumor, indications for operation, operative variables, length of hospital stay, postoperative complications, and progress.
Preoperative evaluation
All patients had a chest X-ray, ultrasonography (USG) of the abdomen, and either contrast computed tomography (CT) of the abdomen or magnetic resonance imaging (MRI). Laboratory blood tests for hepatitis B surface antigen, antibodies to hepatitis C, serum alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA19-9), serum albumin, serum total bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and prothrombin time were obtained. All resected specimens were verified by histopathological examination after the operation.
Surgery
Surgery was performed through a bilateral subcostal incision. During the operation, we carefully searched the abdominal cavity for extent of local disease, extrahepatic metastases, and peritoneal seeding. After mobilization of the liver, intraoperative ultrasound was performed to assess the number and the size of the lesions as well as to assess the relation of the tumor to important vascular structures. The Pringle maneuver was selectively applied to occlude the blood inflow to the liver. Liver resection was carried out by a clamp-crushing method.
Postoperative management
During the early postoperative period all patients received the same postoperative care by the same team of surgeons in the intensive care unit. Need for extending the stay in the intensive care unit was determined by the patient’s condition. Liver function test and clotting profile were monitored.
Follow-up
All patients had postoperative follow-up by the same team of surgeons. The follow-up program was similar for all patients and included abdominal USG and a liver function test every year and then at gradually increasing intervals.
Results
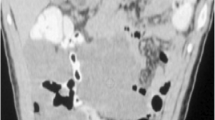
During the study period, 64 patients (42 men and 22 women) underwent partial hepatectomy for IMT of the liver in our center. The patient characteristics are shown in Table 1. The commonest clinical presentation was abdominal pain (53%), followed by fever (41%); 15.6% of patients were asymptomatic. Contrast computed tomography (CT) scan was carried out on 44 patients and magnetic resonance imaging (MRI) with gadolinium-enhanced images was carried out on 28 patients. The radiographic appearance varied, and in the majority of patients it was difficult to make a specific diagnosis based on the findings of the imaging studies. The radiological features are shown in Table 2. Before operation, only five patients (8%) were suspected of having IMT of the liver in the differential diagnoses, whereas 39 patients (60.9%) were diagnosed to have malignant liver tumors. The clinical features of those five patients are shown in Table 3.
The indications for surgery and the surgical details are shown in Table 4. Some patients had more than one indication for surgery. The postoperative complication rate was 17.2%. No patient developed liver failure or postoperative ascites/encephalopathy. There was no hospital mortality. Based on the pathological findings and clinical behavior, all tumors were benign. The tumor and pathological features are shown in Table 5. After a median follow-up of 30 months (range: 5–96 months), no patient was found to have recurrence.
Discussion
Inflammatory myofibroblastic tumor of the liver is rare. To the best of our knowledge, the present cohort study represents a major proportion of the cases reported in the medical literature. Therefore, our study is important for a better understanding of this unusual tumor.
The etiology and pathogenesis of IMT remain unknown, although the tumors were initially thought to represent a reactive inflammatory process. Factors that have been hypothesized in the pathogenesis include infection, vascular diseases, and autoimmune disorders [6–8]. Some authors have even hypothesized that micro-organisms from certain conditions such as appendicitis, could seed the hepatic parenchyma through the portal vein, thus creating an inflammatory reaction with obliterating phlebitis and granulomata formation [7]. In our series, two patients (3.1%) had a past history of gastrointestinal infective disease. Some patients in other series have been reported to have Epstein-Barr virus (EBV)–positive inflammatory follicular dendritic cell tumors [8]. However, any association between IMT and infectious organisms is doubtful because in most reported series, including ours, no acid-fast organisms, fungi, parasites, or bacteria could be identified, and EBV has not been detected with in situ hybridization in the tumors in most reported cases. Some authors believe that the etiology of the IMT lesions is vascular, a result of intraparenchymatous hemorrhage secondary to trauma or coagulopathy [8]. The high content of plasma cells in these lesions has led some authors to hypothesize an immunological origin of this disease [9]. In our series, one patient (1.6%) had a medical history of autoimmune disease. Based on the findings of our study, there was no single etiological factor that could be identified in all the patients.
The diagnosis of IMT without an operation is difficult, despite the use of modern imaging and laboratory techniques. The lesions are often confused with other tumors, such as primary or secondary neoplasms, because their clinical presentation and morphological appearance are nonspecific. There have been limited radiological descriptions of the appearances of hepatic IMT. In most cases, CT scans and MRI are usually performed to narrow the differential diagnosis and to rule out malignancy [10, 11]. Even fine needle aspiration cytology or core biopsy often just shows a large number of inflammatory cells [3, 12, 13], thus a definitive diagnosis cannot be reached. As a consequence, most IMT are diagnosed after surgical resection.
On gross examination, IMT tends to be circumscribed or multinodular, firm, white or tan, with a whorled fleshy, fibrotic or myxoid cut surface. The surface, in a minority of cases, has a variegated appearance with areas of necrosis and hemorrhage. Microscopically, three basic histological patterns are recognized: (1) myxoid, vascular, and inflammatory areas resembling nodular fasciitis; (2) compact spindle cells with intermingled inflammatory cells (lymphocytes, plasma cells, eosinophils) resembling fibrous histiocytoma; and (3) dense plate-like collagen resembling a desmoid or scar [2]. There is little pleomorphism or mitotic activity. Immunohistochemistry is a valuable adjunct to light microscopic diagnosis. Vimentin is almost invariably positive in the spindle cells. Smooth muscle actin and muscle-specific actin are present in the majority of cases. Desmin, CD68, pankeratin, and polyclonal carcinoembryonic antigen (pCEA) are positive in some cases, whereas S100, CD21, and myoglobin are uniformly negative.
There are various treatment options for IMT of the liver [3, 12–15]. Surgery, high-dose steroids, irradiation, and chemotherapy have all been suggested. Spontaneous regression has also been reported in IMT [14]. Although some authors suggest observation or conservative therapy with steroids or nonsteroidal anti-inflammatory drugs, if a definitive diagnosis of IMT of the liver can be made, surgical resection is the preferred treatment. The value of resection has been demonstrated in patients in whom a definitive histological diagnosis could not be made preoperatively or intraoperatively by frozen section. The natural course of IMT without resection is unclear. A small proportion of patients with local recurrence or metastases after partial hepatectomy have been recorded [4, 5]. In fact, most patients reported in the medical literature recovered uneventfully after partial hepatectomy. Because the morbidity and mortality of partial hepatectomy in noncirrhotic livers is low, surgical resection with clear margins should be considered as the treatment of choice for IMT in patients with good surgical risk. In our series, partial hepatectomy offered excellent results with low morbidity and zero mortality.
References
Pettinato G, Manivel JC, De Rosa N et al (1990) Inflammatory myofibroblastic tumor (plasma cell granuloma). Clinicopathologic study of 20 cases with immunohistochemical and ultrastructural observations. Am J Clin Pathol 94:538–546
Coffin CM, Watterson J, Priest JR et al (1995) Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 19:859–872
Chen HW, Lai EC, Huang XJ et al (2008) Inflammatory myofibroblastic tumours of the spleen and liver. Asian J Surg 31:25–28
Zavaglia C, Barberis M, Gelosa F et al (1996) Inflammatory pseudotumour of the liver with malignant transformation. Report of two cases. Ital J Gastroenterol 28:152–159
Pecorella I, Ciardi A, Memeo L et al (1999) Inflammatory pseudotumour of the liver—evidence for malignant transformation. Pathol Res Pract 195:115–120
Horiuchi R, Uchida T, Kojima T et al (1990) Inflammatory pseudotumor of the liver. Clinicopathologic study and review of the literature. Cancer 65:1583–1590
Cheuk W, Chan JK, Shek TW et al (2001) Inflammatory pseudotumor-like follicular dendritic cell tumor: a distinctive low-grade malignant intra-abdominal neoplasm with consistent Epstein-Barr virus association. Am J Surg Pathol 25:721–731
Cotelingam JD, Jaffe ES (1984) Inflammatory pseudotumor of the spleen. Am J Surg Pathol 8:375–380
Grouls V (1987) Pseudolymphoma (inflammatory pseudotumor) of the liver. Zentralbl Allg Pathol 133:565–568
Abehsera M, Vilgrain V, Belghiti J et al (1995) Inflammatory pseudotumor of the liver: radiologic-pathologic correlation. J Comput Assist Tomogr 19:80–83
See TC, Davies SE, Appleton DS et al (2005) CT and angiographic features of hepatic inflammatory myofibroblastic tumour. Clin Radiol 60:718–722
Locke JE, Choti MA, Torbenson MS et al (2005) Inflammatory pseudotumor of the liver. J Hepatobiliary Pancreat Surg 12:314–316
Koea JB, Broadhurst GW, Rodgers MS et al (2003) Inflammatory pseudotumor of the liver: demographics, diagnosis, and the case for nonoperative management. J Am Coll Surg 196:226–235
Yamaguchi J, Sakamoto Y, Sano T et al (2007) Spontaneous regression of inflammatory pseudotumor of the liver: report of three cases. Surg Today 37:525–529
Mangiante GL, Colombari R, Portuese A et al (1997) Inflammatory pseudotumor of the liver: case report and review of the literature. G Chir 18:417–420
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, L., Lai, E.C.H., Cong, Wm. et al. Inflammatory Myofibroblastic Tumor of the Liver: A Cohort Study. World J Surg 34, 309–313 (2010). https://doi.org/10.1007/s00268-009-0330-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0330-x