Abstract
Background
Various factors regarding the biological state of tumors or the nutritional status of patients have been reported individually to correlate with prognosis. Identification of defined patient groups based on a prognostic score may improve the prediction of survival and individualization of therapy. The aim of the present study was to identify clinically useful parameters obtainable before treatment that could be used for predicting clinical outcomes in patients with gastric cancer.
Methods
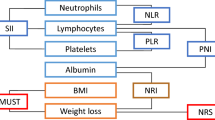
In 357 consecutive patients who had been treated for potentially curable gastric cancer, we retrospectively analyzed the following clinicopathological factors: sex, age, body mass index, body weight changes, hemoglobin, white blood cell count, neutrophil to lymphocyte (N/L) ratio, serum C-reactive protein (CRP), serum albumin, serum cholinesterase, tumor location, tumor size, histology, and clinical tumor node metastasis (TNM) stage. Factors related to prognosis were evaluated by univariate and multivariate analysis.
Results
From univariate analysis, significant differences in survival were found for age, hemoglobin, N/L ratio, serum CRP, serum albumin, serum cholinesterase, tumor size, and clinical T and N grouping. N/L ratio, tumor size, and clinical T grouping were identified as independent prognostic indicators in multivariate analysis. A prognostic score was constructed using these variables to estimate the probability of death. The model gave an area under the receiver operating characteristic curve of 0.85 for prediction of death at 5 years.
Conclusions
This model based on N/L ratio, tumor size, and clinical T grouping before treatment offers a very informative scoring system for predicting prognosis of gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a result of advances in diagnostic methods and surgical treatment, the 5-year survival rate of patients with gastric cancer has steadily increased, reaching >60% in Japan [1, 2]. However, approximately a quarter of patients who undergo curative resection of gastric cancer suffer recurrence [2].
Prognosis depends on cancer stage. Patients with stage I disease have a good prognosis, and those with stage IV disease show a very poor prognosis [3]. However, we have occasionally encountered patients with unexpected advanced stage disease at operation, even when the diagnosis at clinical staging was early gastric cancer. We have also found patients with early recurrence after curative surgery. Additional factors that can be used to predict prognosis are required. The idea of combining multiple, clinically available host- and tumor-related factors is of great interest and might serve as an excellent basis for clinical decision making, treatment planning, and establishing follow-up schedules.
Various factors regarding the biological state of tumors and the nutritional status of patients have been reported to correlate with prognosis. It is recognized increasingly that it is not only the intrinsic properties of tumor cells that determine tumor spread but also the host inflammatory response [4, 5].
The aim of the present retrospective study was to verify the value of well-known prognostic factors and to identify a clinically useful prognostic score of host- and tumor-related factors, including tumor node metastasis (TNM) stage [6], for individualized therapy in gastric cancer patients with potentially curable gastric cancer.
Methods
Patients
We retrospectively reviewed a database of 357 patients who had been diagnosed with potentially curable gastric cancer at the Department of Gastrointestinal Surgery, Mie University Hospital, Japan between January 1992 and December 2004. Patients who had no laboratory data on the day of admission or no preoperative staging data, or who died from a non-cancer-related cause were excluded from the study. In this study, TNM stage I–III was considered to be amenable to curative surgical resection.
Routine laboratory measurements including hemoglobin, white blood cell, neutrophil, lymphocyte, and platelet counts, C-reactive protein (CRP), albumin, and cholinesterase were carried out on the day of the operation to exclude any inflammatory effects of preoperative sequential examinations, such as endoscopy or esophagogastrography. These laboratory results showed no clinical evidence of infection or any other inflammatory conditions, such as pneumonia. Moreover, no patient had received preoperative chemotherapy or irradiation. Pretreatment body weight was compared with past body weight under healthy conditions.
Preoperative disease staging
Depth of tumor invasion, lymph node metastases, and distant metastasis were estimated from computerized tomography (CT), endoscopy, barium examination, ultrasonography, and endoscopic ultrasound (EUS). When comparing between clinical and pathologic stage according to the TNM classification of the International Union Against Cancer [6], the accuracy rate of preoperative diagnosis was 71.9%. Tumor size was measured under the endoscopic examination before surgery.
Statistical analysis
Data are presented as mean and range (95% confidence interval [CI]). The Cox proportional hazards model was used to determine the effects of host- and tumor-related factors on survival time in univariate and multivariate analysis. A Kaplan–Meier analysis and log-rank test were used to compare mortality. Models were developed from host- and tumor-related factors. Receiver operating characteristic (ROC) curves were used to select cut-off values for continuous variables. Values with the best combination of sensitivity and specificity were chosen. The performance of the prognostic model was assessed by determining the area under the ROC curve. Estimates of probability of death within 2 and 5 years were calculated from survival.
Results
Demographic characteristics
Patient characteristics are shown in Table 1. The subject group was composed of 245 men and 112 women, with a mean age of 63.4 years (range: 32–87 years). According to clinical TNM classification, the number of patients with stage I, II, and III cancer was 232, 57, and 68, respectively. Lesions were located in the upper third of the stomach in 69 patients, in the middle third in 125, and in the lower third in 163. Histologically, 99 tumors were classified as well-differentiated adenocarcinoma, 99 were moderately differentiated adenocarcinoma, 100 were poorly differentiated adenocarcinoma, and 59 were miscellaneous types, such as signet ring cell carcinoma and mucinous adenocarcinoma.
All patients underwent laparotomy. In 339 patients, the resection was curative (R0 resection). Eighteen patients had unexpected metastatic disease at laparotomy. Among them, 14 patients proceeded to palliative resection and four did not proceed to resection. Total gastrectomy was performed in 133 patients, distal gastrectomy in 211, and proximal gastrectomy in 9.
Median follow-up was 68 months (range: 1–70 months). Ninety-eight patients (27.5%) died within 5 years after operation. Fifty-six patients (16.0%) died within 2 years. The overall 5-year survival rate was 72.5%. According to the clinical TNM staging, the 5-year survival rate of patients with stage I, II, and III cancer was 89.1, 47.4, and 36.7%, respectively (Fig. 1).
Prognostic significance of various parameters
According to univariate analysis, significant differences in the Cox hazard model were observed for age, neutrophil to lymphocyte (N/L) ratio, hemoglobin level, serum albumin level, serum CRP level, serum cholinesterase level, tumor size, and clinical T and N grouping (Table 2). Gender, body mass index, body weight loss, white blood cell count, platelet count, histological type, and tumor location change did not display significant differences.
On the basis of ROC curves, cut-off values with the best discriminatory power for each continuous variable were age ≥70 years, tumor size >3 cm, serum CRP concentration >0.3 mg/dl, hemoglobin level <12 g/dl, serum albumin level <3.5 g/dl, cholinesterase level <0.65 ΔpH, and N/L ratio >2.2 (Table 3). Multivariate analysis demonstrated that high N/L ratio, large tumor size, and advanced clinical T grouping were all independently correlated with prognosis in patients with gastric cancer (Table 4; Fig. 1).
Clinical outcome based on new scoring
Based on these results, we established a new prognostic score for gastric cancer (PSGC) to reliably estimate survival of patients with gastric cancer. The prognostic scoring system was devised by logarithmically transforming the hazard ratio for each of these variables and multiplying by 100. For each patient, a cumulative risk score could be calculated (maximum score 143; Table 5). The prognostic risk score could then be used to estimate the probability of death within 2 years and 5 years after curative surgery. The model gave an area under the ROC curve of 0.86 and 0.85 for prediction of death at 2 and 5 years, respectively (Fig. 2). When predictions from PSGC were compared with those obtained by clinical TNM staging, PSGC discrimination was superior to clinical TNM staging (ROC AUC 0.85 versus 0.78). The advantage of the combined host- and tumor-related factors expressed through the PSGC over the clinical TNM staging is shown in Fig. 3. The heterogeneity, particularly in stages II and III of the clinical TNM staging, was found in our study subjects.
Plot used to assign estimated probability of death with 2 or 5 years after surgery, according to prognostic score. Values along the horizontal axis represented the total risk score attainable through application of the individual risk scores outlined in Table 5. Total scores were not linear, as patients’ scores may not have fallen between these values
Discussion
In the present study, univariate analysis revealed that six host-related factors (age, hemoglobin level, N/L ratio, serum albumin level, serum CRP level, and serum cholinesterase level), and three tumor-related factors (clinical T, clinical N, and tumor size) correlated well with patient survival. Moreover, multivariate analysis identified three independent prognostic indicators: N/L ratio, tumor size, and clinical T grouping. Pretreatment evaluation of the N/L ratio affected the prognosis of gastric cancer patients more strongly than other host-related factors.
Of all pretreatment factors studied, clinical TNM staging is considered to predict the prognosis of gastric cancer most strongly. Determination of clinical TNM staging as accurately as possible before treatment is important. Despite advances in clinical staging accuracy, patients with gastric cancer are still not stratified adequately [7, 8].
Identification of a simple and useful indicator for predicting the prognosis of patients with gastric cancer before treatment is an important goal. Of course, pathological tumor classification is valuable for predicting prognosis of gastric cancer patients. Many studies have detected a number of independent prognostic factors among tumor-related factors for gastric cancer, such as lymph node status, depth of tumor invasion, and some molecular markers [9–11]. However, these prognostic factors are not available to a surgeon at the time of gastric resection because they depend in large part on postoperative histological examination of the resected specimen. When predicting patient prognosis, tumor-related factors, as well as host-related factors need to be considered.
In recent years there has been increasing evidence that there is a positive correlation between inflammatory response before surgery and poor outcome in patients who have undergone potentially curative primary tumor resection [4, 5]. Indeed, the systemic response, as demonstrated by expression of CRP [12–16] and increased N/L ratio [17–21], has been shown to be a disease-independent prognostic factor in a variety of tumors including gastric cancer, when resection is carried out with curative intent. Increased N/L ratio is thought to reflect the host reaction to the biological behavior of the tumor [22]. The systematic inflammatory response features changes in relative levels of circulating leukocytes, and the well-recognized neutrophilia is accompanied by relative lymphocytopenia [23]. Recently, an inverse relationship has been shown to exist between the level of CRP and lymphocyte count in patients with gatroesophageal cancer [14]. Elevated CRP concentration was associated with a greater proportion of patients having lymphocytopenia.
Tumor size is one of the valuable tumor-related factors because it can be measured easily before operation. However, the prognostic value of tumor size in patients with gastric cancer remains controversial. Some studies have shown that tumor size serves as a simple predictor of long-term survival after resection of gastric cancer [24, 25]. Controversially, other studies have reported that tumor size is not an independent prognostic factor in patients with gastric cancer [26–28]. There is a tendency for tumor size to increase with depth of invasion and extent of lymph node metastasis. Recently, a significant independent correlation has been shown to exist between tumor size and cancer-related survival [29]. A larger tumor size than that determined by ROC curve for cancer-related death was associated with poorer cancer-related survival in that study. Interestingly, the cut-off value was 3.5 cm, which was similar to the cut-off value we had established in this study.
In the present study, we devised a new prognostic score using pre-interventional N/L ratio, tumor size, and clinical T grouping. In predicting the probability of death within 2 and 5 years for individual patients, our PSGC score allows good discrimination. Moreover, the score developed in this study allows accurate estimation of the probability of death within 2 years for individual patients. Although the TNM staging system is an important classification tool, at present clinical TNM staging before treatment is not in complete accord with pathological TNM staging. The PSGC staging system therefore seems particularly effective for providing pretreatment information regarding short- and long-term prognosis of patients with gastric cancer. Furthermore, it may be that survival, especially for patients with clinical TNM stage II and III tumors, is influenced by the host- and tumor-related factors, which are not included in TNM staging, an issue that should be kept in mind in the design of future prospective multimodal treatment trials.
In conclusion, we found the following factors to be associated with prognosis in patients with gastric cancer: N/L ratio, tumor size, and clinical TNM staging. From the results of the present retrospective analysis, our prognostic score using these three parameters offers a method of reliably predicting patient survival before operative treatment. This score still requires prospective validation before its introduction into clinical practice.
References
Noguchi Y, Imada T, Matsumoto A et al (1989) Radical surgery for gastric cancer—a review of the Japanese experience. Cancer 64:2053–2062
Maruyama K, Okabayashi K, Kinoshita T (1987) Progress in gastric cancer surgery in Japan and its limits of radicality. World J Surg 11:418–425
Akoh JA, Macintyre IM (1992) Improving survival in gastric cancer: review of 5-year survival rates in English language publications from 1970. Br J Surg 79:293–299
Balkwill F, Mantovani A (2000) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
International Union Against Cancer (1997) TNM Classification of Malignant Tumors, 5th edn. Wiley-Liss, New York
Habermann CR, Weiss F, Riecken R et al (2004) Preoperative staging of gastric adenocarcinoma: comparison of helical CT and endoscopic US. Radiology 230:465–471
Bentrem D, Gerdes H, Tang L et al (2007) Clinical correlation of endoscopic ultrasonography with pathologic stage and outcome in patients undergoing curative resection for gastric cancer. Ann Surg Oncol 14:1853–1859
Kim JP, Lee JH, Kim SJ et al (1998) Clinicopathological characteristics and prognostic factors in 10783 patients with gastric cancer. Gastric Cancer 1:125–133
Siewert JR, Böttcher K, Stein HJ et al (1998) Relevant prognostic factors in gastric cancer. Ten-year results of the German Gastric Cancer Study. Ann Surg 228:449–461
Yasui W, Oue N, Aung PP et al (2005) Molecular-pathological prognostic factors of gastric cancer: a review. Gastric Cancer 8:86–94
Ishizuka M, Nagata H, Takagi K et al (2007) Inflammation-based prognostic score is a novel predictor of postoperative outcome in patients with colorectal cancer. Ann Surg 246:1047–1051
Sharma R, Hook J, Kumar M et al (2008) Evaluation of an inflammation-based prognostic score in patients with advanced ovarian cancer. Eur J Cancer 44:251–256
Crumley AB, McMillan DC, McKerman M et al (2006) An elevated C-reactive protein concentration prior to surgery predicts poor cancer-specific survival in patients undergoing resection for gastro-oesophageal cancer. Br J Cancer 94:1568–1571
Canna K, McMillan DC, McKee RF et al (2006) Evaluation of a cumulative prognostic score based on systemic inflammatory response in patients undergoing potentially curative surgery for colorectal cancer. Br J Cancer 30:1707–1709
Lamb GW, McMillan DC, Ramsey S et al (2006) The relationship between the preoperative systemic inflammatory response and cancer-specific survival in patients undergoing potentially curative resection for renal cell cancer. Br J Cancer 94:781–784
Sarraf KM, Belcher E, Raevsky E et al (2009) Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 137:425–428
Cho H, Hur HW, Kim SW et al (2009) Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother 58:15–23
Yamanaka T, Matsumoto S, Teramukai S et al (2007) The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 73:215–220
Hirashima M, Higuchi S, Sakamoto K et al (1998) The ratio of neutrophils to lymphocytes and the phenotypes of neutrophils in patients with early gastric cancer. J Cancer Res Clin Oncol 124:329–334
Walsh SR, Cook J, Goulder F et al (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts—rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14
Jilma B, Blann A, Pernerstorfer T et al (1999) Regulation of adhesion molecules during human endotoxemia. No acute effects of aspirin. Am J Respir Crit Care Med 159:857–863
Adachi Y, Oshiro T, Mori M et al (1997) Tumor size as a simple prognostic indicator for gastric carcinoma. Ann Surg Oncol 4:137–140
Giuliani A, Caporale A, Di Bari M et al (2003) Maximum gastric cancer diameter as a prognostic indicator: univariate and multivariate analysis. J Exp Clin Cancer Res 22:531–538
Michelassi F, Takahashi DM Jr, Pantalone D et al (1994) Analysis of clinicopathologic prognostic features in patients with gastric adenocarcinoma. Surgery 116:804–809
Yokota T, Ishiyama S, Saito T et al (2002) Is tumor size a prognostic indicator for gastric carcinoma? Anticancer Res 22:3673–3677
Yu CC, Levision DA, Dunn JA et al (1995) Pathological prognostic factors in the second British Stomach Cancer Group trial of adjuvant therapy in resectable gastric cancer. Br J Cancer 71:1106–1110
Jun KH, Junq H, Baek JM et al (2009) Does tumor size have an impact on gastric cancer? A single institute experience. Langenbecks Arch Surg 394:631–635
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mohri, Y., Tanaka, K., Ohi, M. et al. Prognostic Significance of Host- and Tumor-Related Factors in Patients with Gastric Cancer. World J Surg 34, 285–290 (2010). https://doi.org/10.1007/s00268-009-0302-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0302-1