Abstract
Background
The objective of the cross-sectional study reported here was to compare the quality of life of patients with an appropriate stoma site and with that of patients with an inappropriate stoma site.
Materials and methods
Two groups of patients with permanent intestinal stomas were assessed, 174 patients with appropriate stoma sites and 174 patients with inappropriate stoma sites. We used the EORTC QLQ-C30 and the EORTC QLQ-CR38, which evaluate 26 quality of life (QoL) scales. Data analysis was performed with SPSS software.
Results
From a total of 9 functional scales, 3 scales in patients with an appropriate stoma site were significantly higher than in patients with an inappropriate stoma site: sexual enjoyment (71.2% vs. 63.2%; p = 0.02), physical functioning (74.3% vs. 68.2%; p = 0.005), and role functioning (74.3% vs. 64.4%; p < 0.0001). From the total of 16 symptom scales, patients with an inappropriate stoma site had significantly more problems than patients with an appropriate stoma site in 8 scales: micturation (27% vs. 22.5%; p = 0.04), gastrointestinal problems (32.6% vs. 27%; p = 0.01), weight loss (36.5% vs. 29.2%; p = 0.03), dyspnea (25.95% vs. 12.5%; p = 0.0001), pain (39.3% vs. 29.6%; p = 0.001), fatigue (43.5% vs. 34.5%; p < 0.0001), nausea and vomiting (18.15% vs. 12.8%; p = 0.03), and insomnia (39.8% vs. 31.1%; p = 0.01). Patients with an appropriate stoma site scored global QoL significantly higher than those with an inappropriate stoma site (56.2% vs. 49.7%; p = 0.007)
Conclusions
A perfectly placed intestinal stoma is strongly related to good QoL for affected patients. From the total of 26 QoL scales assessed in the study, patients with appropriate stoma sites achieved better results in at least 50% of the scales.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stoma surgery profoundly affects a person’s life. The medical literature abounds with articles proclaiming the presumed negative impact that ostomies have on quality of life (QoL) [1–15]. They all show that stoma surgery has a great influence on a patient’s daily life.
Patients with stomas face many problems, both physical and psychological. Leakage caused by failure of adhesive or bag welds, ballooning of bags, difficulty in keeping bags in place, and poor siting are some of the problems that affect daily life. Anxiety and embarrassment over a stoma may lead to alterations in lifestyle, including the ability to find work, desire to travel, and overall self image. The way patients feel about the changes in their bodies can affect their behavior toward family and friends; problems with sex life also occur. Some patients have initial problems with diet and clothing, but most patients are thought to adapt with time [1].
Another possible problem for several days or weeks after formation of a stoma is “phantom rectum,” or the urge to defecate (empty the bowel). The inconvenience and distress caused by the need to adapt and by other changes in lifestyle and body image related to stomas are poorly documented.
In the modern health management guidelines, patient satisfaction is of paramount importance when planning future care and treatment, but information on how to achieve this for stoma patients is lacking. It seems that there are some factors that can change the intensity of these complications and promote good quality of life. One of these factors may be stoma siting. Inappropriate stoma sites are places that decrease the patient’s functioning, like body prominences—the iliac crest, costal margin, or umbilicus—or abdominal scars, the waistline or belt line; near a pendulous breast or an abdominal fat roll, on a radiation-affected abdominal wall, in the area of an abdominal herniation, or on a mobile abdominal wall. Cotton and Richard state that surgical technique is the most important factor in the creation of an appropriate or inappropriate stoma and the resulting effects on the patient’s quality of life [2].
The aim of the present study was to document the problems faced by patients with permanent intestinal stomas, and to compare the quality of life in patients with appropriate and inappropriate stoma sites.
Materials and methods
Between March 2006 and March 2008, records of 348 patients with permanent intestinal stomas were collected from Iranian Stoma Association, the only center of stoma patient care in Iran. The group included 174 patients with an appropriate stoma site and 174 patients with an inappropriate stoma site were selected by the nonprobability convenience sampling method.
The patients voluntarily completed the questionnaires after they received some information about the study and understood the goals of the research. No one refused to participate in the study. The reason for stoma creation was intestinal cancer curative surgery, and the patients with other causes for stoma creation were not included. Patients who had been affected by either local or distant recurrences or new cancers were excluded.
Although the healthcare professionals in the Iranian Stoma Association are aware of the appropriate and inappropriate stoma sites and specialize in stoma care, we shared our definitions (mentioned in background) with them at the beginning of the study and asked them to mention the appropriateness of the stoma site for each individual after the questionnaires were completed by the patients.
We used a cancer-specific self-administered questionnaire, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire EORTC QLQ-C30. This questionnaire has been used in more than 2,200 studies [16], and we used the latest (third) version in this study. We also used another self-administered questionnaire, which is a colorectal-specific QoL questionnaire—the EORTC colorectal quality of life questionnaire QLQ-CR38.
The EORTC QLQ-30 contains 30 questions and it is subdivided into five functional levels (physical, role, emotional, cognitive, and social), nine symptom scales (fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties), and one global quality of life scale. Scores are summed and transformed to a score range from 0 to 100. A high score for a functional scale represents a high level of functioning, and a high score for the global health status and quality of life represent a high quality of life. In contrast, a high score for a symptom scale or item represents a high level of symptomatology and problems [17].
The EORTC QLQ-CR38 consists of 38 questions: 19 questions are completed by all patients, whereas the remaining 19 questions are divided into groups of questions relevant for subsamples of patients only (i.e., male or female, patient with or without a stoma). The EORTC QLQ-C38 is subdivided into four functional scales (i.e., body image, sexual functioning, sexual enjoyment, and future perspective), eight symptom scales (micturition problems, gastrointestinal tract symptoms, chemotherapy side effects, defecation problems, stoma-related problems, male and female sexual problems, and weight loss) [17]. Previous studies showed that the EORTC Quality of life Questionnaire C30 (QLQ-C30 had high internal consistency, interscale correlation, and discriminant validity [18, 19]. The EORTC QLQ-CR38 was designed as a supplement to the EORTC QLQ-C30 for use in colorectal cancer clinical trials. The original validation study showed high internal consistency of most scales, good known-good discriminant ability and good change-over-time discriminant ability [20]. Both questionnaires contain questions relating to the previous week.
Five questions regarding age, gender, marital status, educational status, and family history for cancer were added.
Statistical analyses
All data were entered in a computer database and analyzed with SPSS version 14.5. To test for differences between the two groups, the chi-squared test was applied for binary and qualitative variables. For quantitative variables, the t-test and Mann–Whitney U-test were used as appropriate. Differences were considered significant at p < 0.05.
Results
The two groups were comparable with respect to gender, marital status, and educational level, but they were not comparable regarding the mean age. The age of patients with an appropriate stoma site was significantly higher than those with an inappropriate stoma site. The patients’ characteristics are displayed in Table 1. Patients were preliminarily operated for malignancy of the small or large intestine.
Table 2 reports the mean scores and statistical analysis of the functional and symptom scales of the QLQ-C38 in patients with appropriate and inappropriate stoma sites.
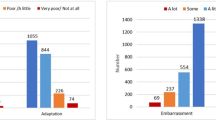
The data from the CR38 questionnaire showed that the patients with an appropriate stoma site had a significantly better sexual functioning score (71.2 vs. 63.2; p = 0.02). No other difference was observed on the other functional scales. Patients with an appropriate site had a significantly better score in the following symptom scale categories: micturation problems (27 vs. 22.5; p = 0.04), gastrointestinal tract symptoms (32.6 vs. 27; p = 0.01), and weight loss (36.5 vs. 29.2; p = 0.03).
According to the results of the QLQ-C30 questionnaire (Table 3), patients with an appropriate stoma site had significantly better functional level scores in several categories—physical functioning (74.28 vs. 68.23; p = 0.005), role functioning (74.3 vs. 64.39; p < 0.0001), and emotional functioning (38.5 vs. 44.8; p = 0.02)—as well as in global health status (G-QOL) (56.2 vs. 49.7; p = 0.07). For patients with an appropriate site, better results were also registered on the symptoms scale for dyspnea (p < 0.0001), pain (p = 0.001), fatigue (p < 0.0001), nausea and vomiting (p = 0.03), and insomnia (p = 0.01). However, it may be of some interest to note that emotional level in patients with an inappropriate stoma site was better (p = 0.02).
Discussion
It is mandatory to form the stoma according to established surgical principles performed with meticulously sound surgical technique. A perfectly placed stoma in an appropriate site, allowing easy care and management in the long term, is essential for the patient’s quality of life. This study confirms the finding that the patient with an inappropriate stoma site has a lower QoL in comparison with patients whose stoma is placed appropriately. The latter group had a significantly better score in sexual functioning and role functioning; they had fewer micturation and gastrointestinal problems, less pain and fatigue, and less nausea and insomnia.
We could not match the age between the two groups in our study, but our review of the literature revealed an article describing the impact of age on quality of life in patients with rectal cancer [4]. The authors showed that QoL is dynamic over time, and that age has an impact on QoL and sexuality. Patients aged >70 years were affected by impaired physical functioning and global health, as well as fatigue, whereas patients <70 years experienced increased strain because of impaired sexual function.
The finding that emotional functioning was better in patients with an inappropriate stoma site may be explained by the confounding effect of age. Although the mean age of patients with an inappropriate stoma site was lower than in the other group, they had a worse QoL score; this can show a stronger negative effect of an inappropriate stoma site on QoL.
We did not use randomization for selecting the subjects of our study. Stoma patients treated between March 2006 and March 2008 were asked to complete the Iranian Stoma Association questionnaires, and they voluntarily agreed to do so. There is always a potential and unavoidable possibility for selection bias in this kind of data collection, which is based on the volunteers’ motivation to participate the study. We tried to reduce this probability by increasing the sample size to include a representative group of stoma patients. Moreover, the patients were well informed about the goals of the project, and nobody refused to participate.
We found very few reports on QoL with respect to stoma site. Arumugam et al., in a prospective study on 97 stoma patients, showed that preoperative siting by stoma nurses and the grade of the operating surgeon did not affect outcome [5]. In another study in patients with a temporary stoma, the impact of having the stoma on patients’ daily life was assessed [3]. The researchers hypothesized that an ileostomy would be superior because there would be fewer complications and the procedure would have a more favorable site with respect to clothing and stoma appliance management. They also indicated that careful surgical technique in stoma construction will minimize technique-related complications and that a period of follow-up care under the direction of a stoma care nurse will minimize problems associated with stoma management.
Buchman and Huber, in a review of the literature, determined that stoma creation is related to up to 50% of the difficulties affecting QoL. Two main causes reported in the literature are stoma care and positioning of the stoma. During the first few postoperative weeks the diameter of the stoma may shrink by as much as one-third. During this phase, without professional assistance by a stoma therapist the risk of skin problems is high. Late complications, such as prolapse, parastomal hernia, and stenosis, are generally the result of a too lateral positioning of the stoma or of early complications as necrosis, dehiscence, retraction, and parastomal abscess [6].
Our study highlights the effect of stoma positioning and its effect on the patient’s quality of life.
Conclusions
We can conclude from this study and other reports that an adequate and perfectly placed intestinal stoma is strongly correlated with good quality of life for stoma patients. In contrast, an inappropriate stoma site will negatively affect the patient’s quality of life.
References
Nugent KP, Daniels P, Stewart B et al (1999) Quality of life in stoma patients. Dis Colon Rectum 42:1569–1574
Cottam J, Richards K, Hasted A et al (2007) Results of a nationwide prospective audit of stoma complications within 3 weeks of surgery. Colorectal Dis 9:834–838
Gooszen AW, Geelkerken RH, Hermans J et al (2000) Quality of life with a temporary stoma: ileostomy vs. colostomy. Dis Colon Rectum 43:650–655
Schmidt CE, Bestmann B, Kuchler T et al (2005) Impact of age on quality of life in patients with rectal cancer. World J Surg 29:190–197
Arumugam PJ, Bevan L, Macdonald L et al (2002) A prospective audit of stomas-analysis of risk factors and complications and their management. Colorectal Dis 5:49–52
Buchmann P, Huber M (2007) [The complicated stoma—late complications, conservative and surgical management.] Ther Umsch 64:537–544 [German]
Nilsson LO, Kock NG, Kylberg F et al (1981) Sexual adjustment in ileostomy patients before and after conversion to continent ileostomy. Dis Colon Rectum 24:287–290
Follick MJ, Smith TW, Turk DC (1984) Psychosocial adjustment following ostomy. Health Psychol 3:505–517
Foulis W, Mayberry JF (1990) Elderly ileostomists and their social problems. J Clin Gastroenterol 12:276–278
Walsh BA, Grunert BK, Telford GL et al (1995) Multidisciplinary management of altered body image in the patient with an ostomy. J Wound Ostomy Continence Nurs 22:227–236
Bekkers MJ, van Knippenberg FC, van den Bome HW et al (1995) Psychosocial adaptation to stoma surgery: a review. J Behav Med 18:1–31
Karadağ A, Menteş BB, Uner A et al (2003) Impact of stoma therapy on quality of life in patients with permanent colostomies or ileostomies. Int J Colorectal Dis 18:234–238
Silva MA, Ratanayake G, Deen KI (2003) Quality of life of stoma patients: temporary ileostomy versus colostomy. World J Surg 27:421–424
Scarpa M, Barollo M, Polese L et al (2004) Quality of life in patients with an ileostomy. Minerva Chir 59:23–29
Marquis P, Marrael A, Jambon B (2003) Quality of life in patients with stomas: the Montreux study. Ostomy Wound Manag 49:48–55
EORTC QLQ-C30 scoring manual, 3rd edn (2001) EORTC Data Center Quality of Life, Unit, Brussels, p. 1–78
Breukink SO, Van der Zaag-Loonen HJ, Bouma EMC et al (2007) Prospective evaluation of quality of life and sexual functioning following laparoscopic total mesorectal excision. Dis Colon Rectum 50:147–155
Aaronson NK, Ahmedzai A, Berman BA et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality of life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Apoplone G, Filiberti A, Cifan S et al (1998) Evaluation of the EORTC QLQ-C30 questionnaire: a comparison with the SF-36 health survey in a cohort of Italian long-survival patients. Ann Oncol 9:549–557
Sprangers MAG, Velde A, Aaronson NK (1999) The construction and testing of the EORTC colorectal cancer-specific quality of life questionnaire module (QLQ-CR38). Eur J Cancer 35:238–247
Acknowledgments
The authors thank the staff of the Iranian Stoma Association for kind and helpful support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mahjoubi, B., Kiani Goodarzi, K. & Mohammad-Sadeghi, H. Quality of Life in Stoma Patients: Appropriate and Inappropriate Stoma Sites. World J Surg 34, 147–152 (2010). https://doi.org/10.1007/s00268-009-0275-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0275-0