Abstract
Background
Although some lymph nodes (upper para-esophageal lymph nodes) that exist between the right recurrent laryngeal nerve and the esophagus should be involved in central-compartment lymph node dissection (CLND) in patients with papillary thyroid cancer, the procedure can cause some injury to the nerve. We set out to assess the incidence of right upper para-esophageal lymph node metastasis after routine CLND.
Methods
Records from 123 patients with PTC who underwent total thyroidectomy with CLND were reviewed.
Results
Fourteen of 123 patients exhibited nodal metastasis in right upper para-esophageal lymph nodes. Metastasis of right upper para-esophageal lymph nodes was usually associated with lesions of the right thyroid, comparatively large tumor size (more than 1 cm), and lateral cervical lymph node metastasis (p < 0.05).
Conclusions
Right upper para-esophageal lymph nodes should be removed during operation for PTC in patients with lesions of the right thyroid gland, large tumor size, and lateral cervical lymph node metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical lymphatic metastases are quite common in papillary thyroid cancer (PTC), found in 20%–50% of patients by standard pathology techniques [1]. Cervical lymph node metastases do not seem to adversely affect survival, but they are known to significantly correlate with the persistence of PTC, the need for reoperation, and recurrence of PTC [2, 3]. Although the role of elective neck dissection has not been clearly defined, the American Thyroid Association recommends that routine central lymph node (level VI) dissection (CLND) should be considered for patients with PTC [1].
Central-compartment lymph nodes (CLN) lie in the central portion of the neck. Its superior border is the hyoid bone, the inferior border is the suprasternal notch, and the lateral borders are the common carotid arteries. Central compartment lymph nodes include pretracheal and paratracheal nodes, the Delphian node, and the perithyroidal nodes, including those along the recurrent laryngeal nerve [4].
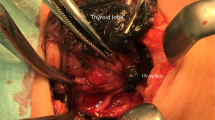
The right recurrent laryngeal nerve ascends through the fibrofatty tissue of the CLN, a different course from that followed by the left recurrent laryngeal nerve. Some lymph nodes exist between the right recurrent laryngeal nerve and the esophagus and/or prevertebral fascia (Fig. 1). Although Grodski et al. [5] recommend that some lymph nodes (right upper para-esophageal lymph nodes) posterior to right recurrent laryngeal nerve should be involved in routine CLND, this procedure can cause injury to the nerve, resulting from traction and elevation during the removal of the lymph nodes. It is therefore essential to investigate the incidence of lymph node metastases posterior to the right recurrent laryngeal nerve in patients with PTC. Although there are some studies on the incidence and pattern of CLN metastasis in PTC, there are few studies on the incidence of right upper para-esophageal lymph node metastasis of nodes posterior to the right recurrent laryngeal nerve [6, 7].
Schematic diagram indicating the location of the upper para-esophageal lymph nodes (area defined by bold line). The right recurrent laryngeal nerve ascends through the fibrofatty tissue of the central-compartment lymph nodes (indicating the difference in the course of the left and right recurrent laryngeal nerves). Some lymph nodes exist between the right recurrent laryngeal nerve and the esophagus and/or the prevertebral fascia
The purpose of this study was to assess the incidence and pattern of and prognostic factors related to right upper para-esophageal lymph node metastasis and to determine whether the resection of these lymph nodes should be part of routine CLND in patients with PTC.
Methods
Patients
We reviewed the medical records of 123 patients (102 women and 21 men; mean age, 44.3 years; age range: 23–78 years) who underwent a total thyroidectomy with routine CLND for PTC at the Department of Otorhinolaryngology-Head and Neck Surgery, Pusan National University Hospital, Pusan, Korea, from March 2007 to February 2008. This retrospective review was conducted under the approved guidelines of our institutional review board. Procedures for follicular, medullary, and anaplastic thyroid carcinoma were excluded from this analysis. Patients who underwent CLND for recurrent PTC after thyroidectomy were also excluded. Preoperative assessment for cervical lymph node metastasis included high-resolution ultrasound scan, fine-needle aspiration cytology, and computerized tomography (CT) scan. Nineteen patients required lateral or modified radical neck dissection.
Surgical technique
All patients underwent total thyroidectomy with routine CLND. This dissection was performed completely according to a techniques similar to that described by Grodski et al. [5]. Our surgical technique for CLND is as follows; the recurrent laryngeal nerve is usually identified distally near the lower border of the cricothyroid muscle. After the thyroid is removed, the nerve is dissected retrograde to the point where it courses under the clavicles, the innominate artery, or the right carotid artery. The fibrofatty tissues are dissected off the nerve and usually reflected medially, and then dissected off the trachea. If possible, the specimen is removed en bloc. However, additional nodal contents that are deep to the right recurrent laryngeal nerve may be removed separately. Attention is given in particular to identify the parathyroid glands, and auto-transplantation of the parathyroid glands was performed only when their vascularity was compromised.
Lymph node compartments
The CLN were divided into three nodal sites: left central compartment lymph nodes, right paratracheal lymph nodes, and right upper para-esophageal lymph nodes (posterior to the right recurrent laryngeal nerve). The nodes were classified by the operating surgeon. The pretracheal and Delphian nodes were included in the right paratracheal LN or left central compartment LN according to the location of the primary lesion. The patients were considered to have a positive site when one or more nodes in the particular site were reported to contain a tumor.
Statistical analysis
Student’s t-test and Pearson’s chi-square test were used to assess the relation between metastasis of upper para-esophageal lymph nodes and the following potential predictors: sex, age, primary site, T stage, size, pathologic extracapsular invasion, total dissected lymph nodes, total metastatic lymph nodes, lateral cervical lymph node mestastasis. Statistical significance was defined as p < 0.05.
Results
Assessment of the primary tumor stage revealed a T1 lesion in 37 cases (30.8%), a T2 lesion in 6 cases (4.8%), a T3 lesion in 75 cases (54.5%), and a T4 lesion in 5 cases (4.1%). The number of resected left central compartment lymph nodes, right paratracheal lymph nodes, and right upper para-esophageal lymph nodes per specimen ranged from 1 to 25 (5.93 ± 3.84), 1 to 13 (5.17 ± 4.00), and 1 to 6 (2.92 ± 2.13), respectively (Table 1). The number of resected right upper para-esophageal lymph nodes is less than left central compartment or right paratracheal lymph nodes. The sum of right paratracheal and upper para-esophageal lymph nodes is much than the number of left central compartment lymph nodes.
Sixty-seven (54.5%) of 123 patients exhibited nodal metastasis at CLN. The incidence of lymph node metastasis according to nodal site was 36.6% (45/123) in right paratracheal lymph nodes, 11.4% (14/123) in right upper para-esophageal lymph nodes, 32.5% (40/123) in left central compartment lymph nodes, and 14.6% (18/123) in both right paratracheal and left central compartment lymph nodes (Table 1). Of 14 patients with metastatic lesions in the right upper para-esophageal lymph nodes, all (100%) also had disease in the right paratracheal lymph nodes. Skip metastases (right upper para-esophageal lymph node metastasis without right paratracheal nodal disease) were not found. The rate of right upper para-esophageal lymph node involvement in patients with metastatic lesions in the right paratracheal lymph node was 31.1% (14/45).
We divided our 123 patients into two groups: group A (n = 14) with metastasis of right upper para-esophageal lymph node, and group B (n = 109) without metastasis of right upper para-esophageal lymph node. There were no significant differences in the gender and age of the patients, T stage and pathologic extracapsular invasion was similar between two groups (Table 2). Metastases in the right upper para-esophageal lymph nodes (85.8%, 12/14) usually occurred in association with lesions of the right thyroid. Twelve (17.1%) of the 70 patients with lesions of the right thyroid gland had metastatic lesions in right upper para-esophageal lymph nodes (p = 0.021). The rate of right upper para-esophageal lymph node metastasis in patients with lesions of the left thyroid was 4.6% (2/53).
The mean tumor size did not significantly predict the metastasis of right upper para-esophageal lymph nodes, but patients with large tumor size (>1 cm) were more likely to have a metastatic lesion of this area (p = 0.015). The prevalence of right upper para-esophageal lymph node metastasis in patients with large tumor size (>1 cm) was 18.6% (11/59). In patients with papillary thyroid microcarcinoma (PTMC), 4.6% (3/64) had a metastatic node in the right upper para-esophageal area. Although the number of removed CLN in both groups was not significantly different, the number of metastatic lesions in CLN in group A was significantly higher than that in group B (p < 0.001).
Seven (36.8%) of the 19 patients who underwent lateral or modified neck dissection had metastatic lesions in the right upper para-esophageal lymph nodes, whereas only 7 (6.7%) of the 104 patient who did not have lateral neck dissection were found to have metastatic lesions in this area (p < 0.001). The incidence of nodal metastasis to right upper para-esophageal lymph nodes in patients with right lateral cervical lymph node metastasis was 45.5% (5/11). In the patients with left lateral cervical lymph node metastasis, 25% (2/8) of cases had nodal metastasis in the right upper para-esophageal lymph node.
There were no cases of permanent or transient vocal cord paralysis in this series (Table 3). Transient hypoparathyroidism was a complication in 6 of 14 patients (42.8%) in group A and in 45 of 109 patients (41.3%) in group B. Of transient hypocalcemic patients, 3 (2.4%, 3/123) had permanent hypoparathyroidism requiring calcium supplementation.
Discussion
The benefit and extent of prophylactic CLND dissection in PTC patients is controversial. Some data suggest that prophylactic CLND may decrease recurrence of PTC and likely improves disease-specific survival [8]. However, there may be a higher rate of permanent hypoparathyroidism and unintentional permanent recurrent laryngeal nerve injury when CLND is performed with total thyroidectomy than for total thyroidectomy alone [9, 10]. The right recurrent laryngeal nerve ascends through the fibrofatty tissue of the CLN. Some lymph nodes (specifically, right upper para-esophageal lymph nodes) lie posterior to the right recurrent laryngeal nerve, and injury to the right recurrent laryngeal nerve can occur from traction and elevation during removal of these lymph nodes. However, there have been few studies on the incidence and predictive factors of right upper para-esophageal lymph node metastasis.
In the present study, 11.4% (14/123) of the specimens had metastatic involvement of a right upper para-esophageal lymph node. The rate of right upper para-esophageal lymph node involvement in patients with metastatic lymph nodes on the right side was 31.1% (14/45). Skip metastases (right upper para-esophageal lymph nodes metastasis without right paratracheal lymph nodes metastasis) were not found. The right upper para-esophageal lymph nodes should be removed during dissection in patients with right paratracheal lymph node metastasis. The rate of right upper para-esophageal lymph node metastasis in patients with lesions of the left thyroid gland was 4.6% (2/53). Therefore, right upper para-esophageal lymph nodes may be preserved in routine CLND for left thyroid cancer patients without metastatic lesions in the right paratracheal lymph nodes, according to the operative finding and results of the frozen section.
The incidence of right upper para-esophageal lymph node metastasis in patients with PTMC in our series was 4.6% (3/64). Of those with a large thyroid tumor (> 1 cm), 18.6% (11/59) had metastatic lesions in the right upper para-esophageal lymph nodes. This rate was significantly higher than that for patients with PTMC (p = 0.015). Therefore, the right upper para-esophageal lymph nodes may be preserved in prophylactic CLND for PTMC patients without metastatic lesions in the right paratracheal lymph nodes.
Seven (36.8%) of the 19 patients with lateral cervical lymph node metastasis had nodal metastasis in the right upper para-esophageal lymph nodes. Seven (6.7%) of the 104 patient who did not undergo lateral neck dissection had nodal metastasis in this area. This difference was significant (p < 0.001), and these results indicate that the right upper para-esophageal lymph nodes should be removed during dissection in patients with lateral cervical lymph node metastasis.
Grodski et al. [5] recommend that some lymph nodes (right upper para-esophageal lymph nodes) posterior to the right recurrent laryngeal nerve should be involved routine CLND. Although this procedure could cause some bleeding and injury to the nerve, resulting from traction and elevation during removal of those lymph nodes, in our series there were no cases of significant bleeding or transient or permanent vocal cord paralysis. Although there were 3 cases (2.4%) of permanent hypoparathyroidism in our series, dissection of right upper para-esophageal lymph nodes was not related to the parathyroid dysfunction.
There may be a higher rate of morbidity when CLND is performed with total thyroidectomy than for total thyroidectomy alone [10, 11]. If a metastatic lesion occurs in the right upper para-esophageal lymph nodes, the risk of morbidity associated with reoperation is higher than that associated with primary dissection in this area. In fact, it is very difficult to reoperate on a patient with right upper para-esophageal lymph nodes metastasis after CLND.
Although this study included a limited number of patients, to our knowledge it was the first study on the prevalence of right upper para-esophageal lymph node metastasis in patients with papillary thyroid carcinoma. A large group of patients is required to assess the benefit of prophylactic CLND that includes lymph nodes in the right upper para-esophageal area when treating PTC.
In conclusion, this study demonstrates that right upper para-esophageal lymph node metastasis rarely occurs in patients with lesions of the left thyroid gland or PTMC. These findings provide support for idea that right upper para-esophageal lymph nodes may be preserved in these patients. Metastasis in the right upper para-esophageal lymph nodes was associated with initial lesion of right thyroid gland, comparatively large tumor size (>1 cm), and the presence of lateral cervical lymph node metastasis. These results indicate that right upper para-esophageal lymph node should be removed during dissection for patients with these findings.
References
Cooper DS, Doherty GM, Haugen BR, For The American Thyroid Association Guidelines Taskforce et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic consideration. Surg Oncol Clin North Am 5:43–63
Machens A, Hinze R, Thomusch O et al (2002) Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 26:22–28
Robbins KT, Clayman G, Levine PA et al (2002) Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 128:751–758
Grodski S, Cornford L, Sywak M et al (2007) Routine level VI lymph node dissection for papillary thyroid cancer: surgical technique. Aust N Z J Surg 77:203–208
Lee BJ, Wang SG, Lee JC et al (2007) Pattern of and factors related with central compartment lymph node metastasis in papillary thyroid carcinoma. Korean J Otolaryngol 50:346–350
Lee SH, Lee SS, Jin SM et al (2008) Predictive factors for central compartment lymph node metastasis in thyroid papillary microcarcinoma. Laryngoscope 118:659–662
White ML, Gauger PG, Doherty GM (2007) Central lymph node dissection in differentiated thyroid cancer. World J Surg 31:895–904
Gemsenjäger E, Perren A, Seifert B et al (2003) Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg 197:182–190
Henry JF, Gramatica L, Denizot A et al (1998) Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg 383:167–169
Rosato L, Avenia N, Bernante P et al (2004) Complications of thyroid surgery: analysis of a multicentric study on 14, 934 patients operated on in Italy over 5 years. World J Surg 28:271–276
Acknowledgments
This work was done at Medical Research Institute (2007-18), Pusan National University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, BJ., Lee, JC., Wang, SG. et al. Metastasis of Right Upper Para-Esophageal Lymph Nodes in Central Compartment Lymph Node Dissection of Papillary Thyroid Cancer. World J Surg 33, 2094–2098 (2009). https://doi.org/10.1007/s00268-009-0149-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0149-5