Abstract
Background
Most cases of sporadic primary hyperparathyroidism (PHP) are due to a single parathyroid adenoma and can be treated with minimally invasive parathyroid exploration guided by sestamibi SPECT imaging and intraoperative parathyroid hormone monitoring. Successful surgery depends on identification of the 10–15% of patients with multiglandular disease. Failed initial parathyroid exploration is both costly and morbid. We examined whether a sestamibi SPECT scoring system could predict anatomic findings in patients with PHP.
Methods
Prospective data from 1,061 consecutive patients undergoing initial parathyroid exploration for PHP from March 6, 2000 to September 28, 2007 were reviewed. One nuclear medicine physician performed independent blinded review of 577 available dual time-point sestamibi SPECT scans, and scored the results into 1 of 5 categories: 0—negative, 1—possible, 2—probable, 3—definite adenoma, or 4—multiglandular disease. Intraoperative findings and outcomes at >5 months follow-up were examined. Chi-square and nonparametric analyses were used to evaluate variables for correlation.
Results
Among patients with sestamibi SPECT scan results classified as either 0—negative or 1—possible adenoma, only 211/262 (81%) had a single adenoma, compared to 263/288 (91%) patients with scan results classified as 2—probable or 3—definite adenoma (p < 0.001). Positive predictive values increased in stepwise correlation with sestamibi SPECT image intensity: 1—possible 78.5%, 2—probable 94.3%, and 3—definite adenoma 98.8%. Multiglandular disease was present in 31/144 (22%) patients with a 0—negative scan versus 13/166 (8%) patients with a 3—definite adenoma scan (p = 0.0005). Only 7/27 (26%) patients with scans classified as 4—multiglandular had actual multiglandular disease. Negative scan results were associated with a greater risk of operative failure (p < 0.001).
Conclusions
A simple scoring system based on sestamibi SPECT intensity can predict the likelihood of single adenoma in PHP. Even the best localizing study cannot exclude multiglandular disease preoperatively. Negative sestamibi SPECT scans are associated with a higher rate of operative failure. Because sestamibi SPECT scans of any category do not reliably identify multiglandular disease, expert surgeons must use validated adjuncts to avoid operative failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is well established that sporadic primary hyperparathyroidism (PHP) is most commonly (>85%) due to a single parathyroid adenoma. Durable biochemical cure of PHP can be achieved with focused parathyroid exploration, but limited exploration requires the exclusion of multiglandular disease by techniques such as bilateral four-gland exploration or intraoperative parathyroid hormone (PTH) monitoring [1–4].
Successful parathyroid exploration also depends on accurate preoperative localization. Although ultrasonography and 4-dimensional computed tomography (CT) can localize and/or lateralize enlarged parathyroid glands prior to neck exploration [5, 6], the most studied and accepted technique is technetium-99 m sestamibi scintigraphy. Even better anatomic resolution is achieved when sestamibi is combined with single photon emission computed tomography (SPECT) [7]. Sestamibi SPECT can also facilitate the identification of ectopic parathyroid glands and can often differentiate between superior and inferior glands [8, 9].
However, even with SPECT, preoperative sestamibi imaging can be negative. In two recent studies, approximately 12–18% of PHP patients had negative preoperative sestamibi imaging, and up to 30% of scan-negative patients were found to have multiglandular disease [10, 11]. By contrast, we recently described a large cohort of PHP patients with “lightbulb” sestamibi SPECT results, i.e., scans that showed a single bright focus of tracer uptake, and found that multiglandular disease was anatomically present in 8.4% of such patients [12]. These findings thus suggested that the rate of multiglandular disease may vary with the intensity of sestamibi tracer uptake. To examine this idea, we devised a simple sestamibi scoring system based on the intensity and pattern of sestamibi tracer uptake. We evaluate here its accuracy in relation to the observed anatomic findings at parathyroid exploration for PHP.
Materials and methods
Patients
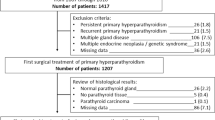
Under an institutional review board-exempted protocol, we retrieved from a prospective clinical database the records of 1,061 patients who underwent surgery for PHP from March 6, 2000 to September 28, 2007, with >5 months follow-up. No patient had prior parathyroid exploration. We found that preoperative sestamibi SPECT scans had been performed at our institution in 577 patients. All 577 of these sestamibi scans were reviewed by one nuclear medicine physician (D.A.P.), who was unaware of the anatomic findings at exploration and who placed each scan into one of five categories according to the intensity and pattern of retained tracer activity on delayed images, as shown in Fig. 1: 0—negative, 1—possible, 2—probable, 3—definite adenoma, and 4—multiglandular disease.
Classification of sestamibi SPECT scans. Early and late maximum intensity projection sestamibi SPECT images. Parathyroid adenoma indicated by the arrows. a Anterior projection of a patient with a 0-negative scan. b Anterior projection in a patient with a 1-possible adenoma manifested by the more caudal extent of the right thyroid lobe compared to the left without clear delayed washout. c Right anterior oblique projection of a patient with 2-probable right superior parathyroid adenoma. d Left anterior oblique projection of a patient with a right inferior definite parathyroid adenoma. e Left anterior oblique projection of a patient with multifocal delayed washout outside the normal borders of the thyroid, consistent with multiglandular disease [12]
The clinical data were reviewed for demographics, presenting symptoms, biochemical profile, history of radiation exposure, prior nonparathyroid neck operation, preoperative ultrasound results, operative findings, and surgical outcomes.
Sestamibi SPECT scanning
Imaging was performed as described elsewhere [12]. Briefly, a peripheral intravenous catheter was placed and patients were positioned with the neck extended. A median dose of 25.2 (range: 6.3–28) MBq Tc-99 m sestamibi was injected, and after a 10-min delay, SPECT imaging was performed using an SMV DST dual head gamma camera (GEMS, Milwaukee, WI) from the skull base through the mid-chest at 30 s/frame, 128 frames. After a delay of approximately 180 min (range: 64–265 min), the imaging was repeated. Image reconstruction using filtered back projection was performed and reviewed on a GE Vision workstation (GEMS, Milwaukee, WI).
Clinical management
Parathyroid exploration was performed as previously described [12] using intraoperative PTH monitoring with results interpreted by our validated and strict criteria [3]. Unilateral exploration was performed whenever possible as allowed by the results of preoperative imaging, identified anatomy, and intraoperative PTH monitoring [12, 13]. Three dedicated endocrine surgeons conducted the explorations. All patients had hypercalcemic hyperparathyroidism at presentation, except one patient who had normocalcemic hyperparathyroidism (described below). Postoperative follow-up occurred at 7–14 days and >5 months. Operative cure was defined as normocalcemia persisting >5 months after surgery. Patients with postoperative normocalcemic hyperparathormonemia at >5 months were treated with calcium and ergocalciferol supplementation until PTH normalized or until recurrent hypercalcemic hyperparathyroidism was diagnosed [12]. Surgical failure was defined as postoperative hypercalcemia, and was categorized as either <5 months from surgery (persistent hyperparathyroidism) or as >5 months from surgery (recurrent hyperparathyroidism).
Statistics
Sestamibi SPECT results were considered true positive if the scan accurately identified the laterality of a single parathyroid adenoma, accurately identified double adenomata, or correctly predicted parathyroid hyperplasia. Sestamibi SPECT results were considered false negative if a single focus of sestamibi tracer uptake was observed preoperatively but multiglandular disease was present at exploration or at follow-up. A false positive scan incorrectly identified an anatomically normal parathyroid gland contralateral to an adenoma or suggested multiglandular disease when only a single adenoma was present. A true negative scan correctly demonstrated no foci of increased sestamibi tracer uptake, with anatomically normal parathyroid glands and was seen in one patient found to have been operated on because of an error in PHP diagnosis.
Statistical analyses were performed with SPSS software (SPSS Inc., Chicago, IL) using chi-square and nonparametric analysis to evaluate for correlation; p values ≤ 0.05 were considered significant.
Results
Distribution versus patient characteristics
Table 1 shows the distribution of the 577 PHP patients whose sestamibi SPECT scan results were assigned by blinded review to one of five intensity scoring categories. Negative sestamibi SPECT results occurred in 144/577 (25%) patients, vague single-site uptake (possible adenoma) was present in 117 (20%), probable or definite single-site uptake was seen in 289 (50%), and a multiglandular imaging pattern was seen in 27 (5%) patients. As the data in Table 1 show, by scoring category there were no differences in demographics, predominant presenting manifestations, biochemical profile, neck irradiation history, or concomitant thyroid pathology. Preoperative neck ultrasound was performed in 71 patients, and the rate of accurate ultrasound localization (67–90%) did not differ by scoring category.
Operative outcomes
Unilateral exploration for adenoma (Table 2) was possible with a frequency that increased as the sestamibi image intensified. By score category, the rate of unilateral exploration was 43% for 0—negative, 59% for 1—possible, 78% for 2—probable, and 83% for 3—definite adenoma. The complications of exploration included hematoma (2 patients, 0.3%) and vocal cord paralysis (1 patient, 0.2%). There were no deaths. Operative failure occurred in 16/577 (2.8%) patients and in every case was due to missed multiglandular disease. To date, 11/16 patients have been able to undergo re-exploration and are biochemically cured at >5 months. One patient with apparent normocalcemic hyperparathyroidism preoperatively had four normal parathyroid glands identified intraoperatively with a decrease in the intraoperative PTH from 113 pg/ml to 71 pg/ml. He remains normocalcemic at 59 months follow-up.
As shown in Table 2, by sestamibi SPECT score category, operative failure was significantly more frequent with a sestamibi SPECT score of 0—negative than for other categories (p < 0.005). Of the 10 patients with 0—negative sestamibi SPECT scans and operative failure, 5 had persistent disease and 5 had recurrent disease diagnosed at a mean of 30 ± 14 months postoperatively.
Sestamibi SPECT score and PHP patients with a single adenoma
As the sestamibi SPECT score increased from 0—negative to 3—definite adenoma, the percentage of PHP patients with single adenoma increased in a stepwise manner from 77% to 92% (Table 3; Fig. 2). The maximum observed rate of single adenoma was only 92%. For patients with single adenoma, as the score increased from 1—possible to 3—definite adenoma, the positive predictive value (79%, 95%, 99%), sensitivity (80%, 88%, 92%), and accuracy (66%, 82%, 90%) of sestamibi SPECT scan results also increased. As shown in Table 3, mean single adenoma weight was examined, and patients whose scans were scored as 0—negative were observed to have lower mean adenoma weights than those with scans scored as 3—definite adenoma (p < 0.005).
Association between sestamibi SPECT score and multiglandular disease
Multiglandular disease, defined as either double adenomata or four-gland hyperplasia, was present anatomically in a total of 74 study patients (12.8%). As the sestamibi SPECT score increased, the percentage of patients with multiglandular disease decreased from 20% to 8% (Fig. 2). Among patients with a sestamibi SPECT score of 4—multiglandular, only 25.9% had actual multiglandular disease. The anatomic findings in PHP patients with scans scored as 4—multiglandular were statistically similar to the findings in PHP patients with scans scored as 0—negative scan.
A total of 43 (7.5%) PHP patients had parathyroid hyperplasia. The majority had either a 0—negative (17/43; 40%) or 1—probable adenoma (12/43; 28%) sestamibi SPECT score. Only 4 (9%) had preoperative sestamibi SPECT that suggested hyperplasia. Hyperplasia was more frequent in patients with a scan scored as 0—negative or 1—possible adenoma (29/266; 11%) than in patients with a scan scored as 2—probable or 3—definite adenoma (9/289; 3%); p < 0.005. Double adenomas, on the other hand, were equally frequent among the five scan categories, ranging from 5% to 8% (p = 0.51).
Discussion
Localization of parathyroid adenomas using sestamibi SPECT imaging has been demonstrated to be accurate and sensitive [9, 14, 15]. To our knowledge, no previous study has attempted to correlate the degree of sestamibi intensity to anatomic findings in PHP patients. Other studies have shown correlation of parathyroid gland size with sestamibi SPECT sensitivity [16–18]. Our own observation that PHP patients with a “lightbulb” scan intensity had a high rate of single-gland disease (92%) led to the development of a novel scoring system based on sestamibi SPECT intensity. Here we demonstrate that the likelihood of single parathyroid adenoma correlates with sestamibi SPECT intensity score in patients with PHP.
A number of studies have evaluated whether parathyroid histopathologic features such as higher weight or greater oxyphil content correlate with sestamibi scan localization accuracy [16–18]. We found that adenoma weight was an important factor in the degree of sestamibi SPECT intensity; higher-weight adenomas were more likely to have a sestamibi SPECT scan scored as a 3—definite adenoma. We did not evaluate whether other histologic characteristics correlated with the accuracy or intensity of sestamibi SPECT scans.
Other studies have evaluated how best to optimize preoperative testing to predict the presence of either single gland or multiglandular disease in patients with PHP. For example, Mózes et al. reported that preoperative PTH and calcium levels alone did not predict the presence of single-gland or multiglandular disease [19]. Kebebew et al. devised a preoperative scoring system which incorporates preoperative calcium and intact PTH levels as well as ultrasound and sestamibi results and found that with the presence of at least three of the five predictive variables, single-gland versus multiglandular disease could be predicted with a positive predictive value of 100% and a sensitivity of 44% [20]. We here demonstrate that sestamibi SPECT intensity alone can be used to predict the likelihood of PHP a single adenoma; PHP patients with sestamibi SPECT scans scored as 3—definite adenoma were most likely to have a single parathyroid adenoma (positive predictive value of 99%, sensitivity of 92%). We did not observe statistically significant differences in calcium or intact PTH levels among the sestamibi SPECT scan scoring categories, suggesting that the preoperative biochemical profile does not correlate with sestamibi SPECT intensity.
We found that as the sestamibi SPECT intensity score decreased, the likelihood of having parathyroid hyperplasia increased (3% for patients with sestamibi SPECT scored as 2—probable or 3—definite adenoma compared to 11% for patients with a scan scored as 0—negative or 1—possible adenoma). The likelihood of double adenomata was the same regardless of sestamibi SPECT results. The poor sensitivity of sestamibi SPECT scans in predicting multiglandular disease has been well documented in other studies [21, 22]. In fact, in our subgroup of patients with sestamibi SPECT scans suspicious for multiglandular disease, only 26% actually had multiglandular disease.
Although our results demonstrate that sestamibi SPECT intensity can predict the likelihood of a single adenoma, our data also show that sole reliance on the imaging findings to exclude multiglandular disease will result in unacceptably high rates of surgical failure. Most endocrine surgeons know this from clinical experience. Operative failure rates among endocrine surgeons range from 0% to 5% [2, 23]. Our study, encompassing as it did the practices of three endocrine surgeons who were at varying stages in their career development, demonstrated a low failure rate of 2.8%, and with no cases of failure due to missed adenoma. While a sestamibi SPECT scan that is 0—negative or 4—multiglandular should increase the suspicion of multiglandular disease, our study data demonstrate clearly that a 3—definite adenoma score does not eliminate the possibility of multiglandular disease, which as we previously reported, is present in 8.4% of patients with these scan results. A validated adjunct such as intraoperative PTH monitoring or four-gland exploration therefore must be routinely used to prevent surgical failure, even in patients with seemingly unequivocal sestamibi SPECT scan results.
Ultrasound can also be an important preoperative imaging modality for parathyroid localization, but at present it is only associated with up to 77% sensitivity [5, 24, 25]. As other investigators have reported, concordant ultrasound and sestamibi scan results demonstrating a single parathyroid adenoma can increase the sensitivity to 96% [25]. In our series, ultrasound correctly localized the abnormal parathyroid gland(s) in 58/66 (88%) patients. As our ultrasound studies are done by a dedicated endocrine radiologist, we attribute the observed high sensitivity rate to operator skill. Among patients with false negative sestamibi SPECT scans, only five had preoperative ultrasound performed. Of these, two (40%) patients had multiglandular disease identified by ultrasound that was missed on sestamibi: in one case the sestamibi SPECT score was 2—probable adenoma and in the other case, the sestamibi SPECT score was 3—definite adenoma.
Overall, ultrasound was most useful in the patients with a sestamibi SPECT scan scored as either 0—negative or 4—multiglandular. It is interesting that in this subgroup, 8/10 (80%) had accurate preoperative identification by ultrasound despite equivocal sestamibi findings. Among these eight patients, confounding factors for accurate sestamibi localization include concomitant thyroid nodules (five patients) or parathyroid adenomas that were in close association with the thyroid (two patients). We now routinely combine preoperative neck ultrasound and sestamibi SPECT scanning for PHP patients preoperatively; additional studies to determine if both modalities are needed for accurate localization in all types of PHP are ongoing.
A number of studies have addressed the accuracy and sensitivity of sestamibi scans in parathyroid localization [4, 7–9, 26]. These studies are difficult to compare because not all use the same definition of true negative, false negative, false positive, and/or true positive. Because laterality is by far the most useful criterion, we selected commonly described definitions that appeared to be the most clinically applicable. The development of standardized definitions in the field would allow for a more accurate comparison and interpretation of studies.
Although we scored sestamibi SPECT scans into five categories, our results stratified easily into three groups. The first group, with equivocal scans, or scans scored as 0—negative and 4—multiglandular, were more likely to have a bilateral neck exploration (97/171, 57%; p < 0.005), parathyroid hyperplasia (19/171, 11%; p = 0.0005), and a failed initial neck exploration (10/171, 6%; p = 0.02). In contrast, the second group with scans scored as 2—probable and 3—definite adenoma were more likely to have a single adenoma (263/289, 91%) and successful unilateral neck exploration. Scans scored as 1—possible adenoma share characteristics of both groups; a unilateral neck exploration is more common (69/117, 59%) with a low operative failure rate (1/117, 0.9%), but the rate of parathyroid hyperplasia (12/117, 10%) is similar to that of scans scored as 0—negative or 4—multiglandular. As our experience with sestamibi SPECT scoring continues to increase, it is possible that additional discriminatory characteristics will be apparent.
In our series of PHP patients, the rate of equivocal preoperative imaging (sestamibi SPECT scans scored as either 0—negative or 4—multiglandular) was 30%. This rate is higher than other published reports, and it most likely reflects a referral bias to a tertiary center, as a common perception has heretofore been (incorrectly) that a lightbulb scan excludes multiglandular disease. The rate of multiglandular disease in the equivocal group (36/171, 21%) was similar to other series [10, 11, 16, 27]. Even among PHP patients with equivocal imaging and single gland disease, parathyroid exploration can be more challenging because of smaller mean gland weights. Chan et al. recently reported that patients with negative preoperative imaging often require more extensive neck exploration to achieve surgical cure [27]. As expected, the majority of patients in our series with equivocal sestamibi SPECT scan findings underwent bilateral neck exploration. Whether the higher rate of surgical failure can be decreased by other modalities, such as neck ultrasound, is currently under study.
Although our scoring system is based on the interpretation of a single radiologist, sestamibi SPECT scans that demonstrate a single bright focus, or 3—definite adenoma, clearly have a higher likelihood of a single adenoma (92%) compared to a 0—negative scan (77%; p = 0.002. Even if differences in sestamibi uptake intensity are subtle except to experienced nuclear medicine physicians, this comparison is obvious and significant. Scans with more than one bright focus are not always (26%) associated with actual multiglandular disease.
Conclusions
A scoring system based on intensity of retained radiotracer activity seen on preoperative sestamibi SPECT scan can help to predict the likelihood of single adenoma in PHP patients, but it cannot exclude multiglandular disease. Sporadic primary hyperparathyroidism patients with equivocal sestamibi SPECT scans have a higher rate of multiglandular disease and a higher rate of operative failure. Routine use of other preoperative parathyroid imaging modalities, such as neck ultrasound, and validated adjuncts, including intraoperative PTH monitoring and/or four-gland exploration, may help avoid surgical failure.
References
Irvin GL III, Solorzano CC, Carneiro DM (2004) Quick intraoperative parathyroid hormone assay: surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg 28:1287–1292
Udelsman R (2002) Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 235:665–670
Carty SE, Worsey J, Virji MA et al (1997) Concise parathyroidectomy: the impact of preoperative SPECT 99 m-Tc sestamibi scanning and intraoperative quick parathormone assay. Surgery 122:1107–1116
Siperstein A, Berber E, Mackey R et al (2004) Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery 136:872–880
Solarzano CC, Carneiro-Pla DM, Irvin GL (2006) Surgeon-performed ultrasonography as the initial and only localizing study in sporadic primary hyperparathyroidism. J Am Coll Surg 202:18–24
Rodgers SE, Hunter GJ, Hamberg LM et al (2006) Improved preoperative planning for directed parathyroidectomy with 4-dimensional comoputed tomography. Surgery 140:932–940
Billotey C, Sarfati E, Aurengo A et al (1996) Advantages of SPECT in technetium–99 m-sestamibi parathyroid scintigraphy. J Nucl Med 37:1773–1778
Lavely WC, Goetze S, Friedman KP et al (2007) Comparison of sestamibi SPECT/CT, sestamibi SPECT, and planar imaging with single- and dual-phase 99 mTc-sestamibi parathyroid scintigraphy. J Nucl Med 48:1084–1089
Sharma J, Mazzaglia P, Milas M et al (2006) Radionuclide imaging for hyperparathyroidism (HPT): which is the best technetium-99 m sestamibi modality? Surgery 140:856–865
Lal A, Chen H (2007) The negative sestamibi scan: Is a minimally invasive parathyroidectomy still possible? Ann Surg 14:2362–2366
Sebag F, Hubbarg JGH, Maweja S et al (2004) Negative preoperative localization studies are highly predictive of multiglandular disease in sporadic primary hyperparathyroidism. Surgery 134:1038–1042
Yip L, Pryma DA, Yim JH et al (2008) Can a lightbulb sestamibi SPECT accurately predict single-gland disease in sporadic primary hyperparathyroidism. World J Surg 32:784–792
Carty SE, Roberts MM, Virji MA et al (2002) Elevated serum parathormone level after “concise parathyroidectomy” for primary sporadic hyperparathyroidism. Surgery 132:1086–1093
Johnson NA, Tublin ME, Ogilvie JB (2007) Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol 188:1706–1715
Civelek AC, Ozalp E, Donovan P et al (2002) Prospective evaluation of delayed technetium–99 m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism. Surgery 131:149–157
Chiu B, Sturgeon C, Angelos P (2006) What is the link between nonlocalizing sestamibi scans, multigland disease, and persistent hypercalcemia? A study of 401 consecutive patients undergoing parathyroidectomy. Surgery 140:418–422
Stephen AE, Roth SI, Fardo DW et al (2007) Predictors of an accurate preoperative sestamibi scan for single-gland parathyroid adenomas. Arch Surg 142:381–386
Mehta NY, Ruda JM, Kapadia S et al (2005) Relationship of technetium Tc 99 m-sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue. Arch Otolaryngol Head Neck Surg 131:493–498
Mózes G, Curlee KJ, Rowland CM et al (2002) The predictive value of laboratory findings in patients with primary hyperparathyroidism. J Am Coll Surg 194:126–130
Kebebew E, Hwang J, Reiff E et al (2006) Predictors of single-gland vs multigland parathyroid disease in primary hyperparathyroidism. Arch Surg 141:777–782
Sugg SL, Krzywda EA, Demeure MJ et al (2004) Detection of multiple gland primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Surgery 136:1303–1309
Haciyanli M, Lal G, Morita E et al (2003) Accuracy of preoperative localization studies and intraoperative parathyroid hormone assay in patients with primary hyperparathyroidism and double adenoma. J Am Coll Surg 197:739–746
Carneiro-Pla DM, Irvin GL III, Chen H (2007) Consequences of parathyroidectomy in patients with “mild” sporadic primary hyperparathyroidism. Surgery 143:795–799
Haber RS, Kim CK, Inabnet WB (2002) Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m) technetium sestamibi scintigraphy. Clin Endocrinol 57:241–249
Arici C, Cheah WK, Ituarte PHG et al (2001) Can localization studies be used to direct focused parathyroid operations? Surgery 129:720–729
Kim CK, Kim S, Krynyckyi BR et al (2002) The efficacy of sestamibi parathyroid scintigraphy for directing surgical approaches based on modified interpretation criteria. Clin Nucl Med 27:246–248
Chan RK, Ruan DT, Gawande AA et al (2008) Surgery for hyperparathyroidism in image-negative patients. Arch Surg 143:335–337
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yip, L., Pryma, D.A., Yim, J.H. et al. Sestamibi SPECT Intensity Scoring System in Sporadic Primary Hyperparathyroidism. World J Surg 33, 426–433 (2009). https://doi.org/10.1007/s00268-008-9841-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9841-0