Abstract
Background
Simulators are being used to teach laparoscopic skills before residents get to the operating room. It is unknown whether the use of three-dimensional (3D) vision will facilitate laparoscopic training. Therefore, our objective was to compare the effectiveness of using 3D imaging over the traditional two-dimensional (2D) imaging to teach laparoscopic simulator skills to novice individuals and assess whether 3D imaging ameliorates laparoscopic performance for surgeons who have already adapted to working within a 2D surgical environment.
Methods
This prospective study involved 36 surgical residents and students. Inexperienced participants included medical students and first- and second-year surgical residents (n = 25). Experienced participants included third- and fifth-year surgical residents (n = 11). Participants were tested on six laparoscopic skills using 2D or 3D imaging systems and then retested about 3 months later using the opposing imaging system. Evaluation of performance was based on the time elapsed to task completion and the errors committed during that time.
Results
The experienced participants performed better than the inexperienced participants regardless of the imaging system. Inexperienced participants initially tested using 2D imaging required significantly more time and/or made more errors to complete five of the six laparoscopic tasks compared to those initially tested using 3D imaging (p < 0.05). After initial testing on 3D imaging, inexperienced participants retested using 2D imaging performed significantly better on five of six tasks compared to the scores of inexperienced participants initially tested on 2D imaging (p < 0.05). In contrast, the inexperienced participants’ retested on 3D after initial 2D imaging did not improve on any laparoscopic task compared to the scores of inexperienced participants initially tested on 3D imaging. Among the experienced participants, no significant difference in time or errors to task completion was observed under 2D imaging compared to 3D imaging during the first or second testing session.
Conclusions
Our study indicates that 3D imaging offers significant advantages in the teaching of laparoscopic skills to inexperienced individuals.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic skills are initially best taught and practiced in an inanimate setting. Various devices are used to aid in this education of laparoscopic skills. These devices range from simple box trainers to sophisticated computer-based virtual reality trainers. Currently, most training devices allow the surgical field to be viewed on a two-dimensional (2D) flat video display panel. Information about the depth of the field and the relative position of the anatomic structures is obtained in an indirect way, mainly by tactile stimulation and previously acquired experience. This 2D imaging has been shown to impair performance compared to natural vision [1, 2]. Although the shortcoming of working under 2D visual conditions can be overcome with intense practice, such an investment in time on the laparoscopic trainers may be difficult to achieve for both educators and residents in light of reduced resident work hours and substantial clinical workloads. Using the operating room for fundamental laparoscopic skill acquisition is uneconomical and unethical. Thus a faster, more efficient way of learning laparoscopic skills using simulation techniques is needed. Three-dimensional (3D) laparoscopic simulators have been developed in an attempt to overcome the problems associated with 2D imaging by restoring the perception of depth in the operating field. Teaching laparoscopic skills using 3D imaging systems might be one way to facilitate learning, especially for novice individuals. Therefore, we evaluated whether there was any advantage of 3D imaging systems with regard to learning laparoscopic simulator surgical skills over conventional 2D imaging systems for novice laparoscopic surgeons and whether 3D imaging systems independently improve performance in laparoscopic simulator skills for experienced surgeons who have already adapted to working in a 2D surgical environment.
Materials and methods
Study population
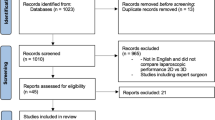
A total of 36 residents and medical students from the General Surgery Residency Program, Baylor College of Medicine and Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX were recruited under an Institutional Review Board-approved protocol. Because previous operative experience has been shown to affect performance on simulators to test laparoscopic surgical skills, participants recruited into the study were first stratified by their laparoscopic experience into inexperienced or experienced groups [3]. This was determined by their postgraduate training year (PGY) and number of recorded Accreditation Council on Graduate Medical Education (ACGME) basic and complex laparoscopic index cases. The inexperienced participants were defined as having ≤2 years of postgraduate training and having performed fewer than two basic laparoscopic procedures, whereas the experienced participants were defined as having >2 years of postgraduate training and having performed 15 to 120 laparoscopic procedures. The inexperienced participants included medical students, physician assistant students, and PGY 1 and 2 surgery residents (n = 25). The experienced participants included PGY 3 and 5 general surgery residents (n = 11). Demographic data, handedness, and whether the participant wears eyeglasses were collected (Tables 1a, 1b).
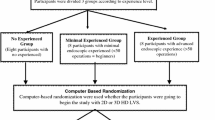
Experimental design
Inexperienced participants were randomly assigned into a two by two crossover trial using a computer–generated randomization schedule to each of two sequences of imaging testing. Group A was assigned to an initial testing session using 2D imaging followed by 3D imaging in a second testing session. Group B was assigned to an initial testing session using 3D imaging followed by 2D imaging in a second testing session (Fig. 1). Experienced participants were also randomized to an initial testing session using 2D imaging followed by 3D imaging in a second testing session (group C) or 3D imaging followed by 2D imaging in a second testing session (group D) (Fig. 1). In terms of effectiveness of randomization, the groups (A vs. B; C vs. D) were statistically similar in all parameters including age, sex, handedness, and laparoscopic experience (Tables 1a, 1b). At the first testing session all participants were asked to perform the same six laparoscopic skills of varying degrees of complexity and requiring different levels of concentration and coordination under their assigned imaging condition (2D or 3D). The 3D imaging was intended to immerse the subject in the natural visual state and eliminate the subjects’ need to adapt to an artificial 2D environment. Subjects were given verbal instructions and a demonstration of how to perform each task prior to starting. No practice was allowed before evaluation of performance. Participants performed each of the laparoscopic tasks two times before moving on to the next one. Performance was supervised and recorded. Next, a given period of time was allowed to elapse (i.e., the washout period), and each participant was then retested (testing session 2) on the same six laparoscopic tasks in the same order but using the opposing imaging system (Fig. 1). The washout period was defined as a nearly 3 months period of time during which no practice was allowed on the 2D or 3D laparoscopic simulators. This time period was chosen to minimize the persistence of any skills acquired from the initial testing session into the subsequent testing session and was based on previous work that showed up to an 80% loss of laparoscopic simulator skill performance after 1 month [4].
Experimental design. A cross-over study involving 25 inexperienced subjects (groups A and B) and 11 experienced subjects (groups C and D). After a given period of time (i.e., washout period) participants were retested on the same six laparoscopic tasks but using a different visual imaging system. The testing sequences were as follows: 2-D then 3-D, group A; 3-D then 2-D, group B; 2-D then 3-D, group C; 3-D then 2-D, group D
Laparoscopic tasks
The six laparoscopic tasks are shown in Table 2. In all tasks, the lighting conditions, laparoscopic instruments, trocar insertion sites, and distance of the scope from the working fields was kept constant for both imaging systems. The only variable that was changed between testing sessions was the imaging condition (i.e., 3D or 2D).
Outcome measures
The mean values for time to complete each task and number of errors made during completion of each task were calculated for the imaging systems. Objective measurements of surgical skills were based on two parameters: time (measured in seconds) and errors (counted in numbers) to complete each task. A statistically better performance on each task was defined as either completion of the task (1) in a significantly shorter amount of time; (2) with significantly fewer errors; or (3) in a significantly shorter amount of time with significantly fewer errors. Acquisition of laparoscopic skills on a task was defined as the difference between the first and last score during the first training session for time and errors.
Imaging systems
The 2D system (Karl Storz, Culver City, CA, USA) was a standard laparoscopic tower with a 10 mm, 0° scope and a three-chip charge coupled device digital system attached to a regular flat video monitor. The 3D system was an Endosite 3Di Digital Vision System (Viking Systems, La Jolla, CA, USA). It included a stereo digital scope (dual 3CCD optical channel) attached to a 3D image-processing unit that transfers information to dual miniature LCD screens attached to a helmet-type headset.
Statistical analyses
Values are given as mean ± standard deviation (SD) if not stated otherwise. Statistical analyses were preformed using a two-sample paired and unpaired t-test as well as Fisher’s exact test as indicated in the text. Differences in performance between the levels of laparoscopic experience were analyzed by a repeated measures analysis of variance (ANOVA). Data were analyzed using the SAS 9.1 (SAS, Cary, NC, USA) software package. A value of p < 0.05 was considered statistically significant.
Results
All participants recruited into this study successfully completed both testing sessions and all six laparoscopic tasks. The average performance time for inexperienced participants to complete a laparoscopic task was 70.7 ± 3.6 seconds compared to 48.2 ± 2.7 seconds for experienced participants (p < 0.01, ANOVA). However, the average number of errors to task completion was not statistically different across experience levels (0.5 ± 0.1 inexperienced vs. 0.44 ± 0.1 experienced participants). Subjective assessment of the 3D imaging system by all participants revealed no complaints of nausea or dizziness. However, 20% of the inexperienced and 9% of the experienced participants complained of discomfort while wearing the head gear.
Testing session one
The inexperienced subjects (group A) who were initially assigned and tested under the 2D imaging condition required a significantly longer time to complete three of the six laparoscopic tasks, on average, compared to the inexperienced subjects initially assigned and tested under 3D imaging (group B) (Fig. 2A). These tasks included ring board exchange (121.2 ± 60.3 vs. 65.4 ± 12.8 seconds, p < 0.01); duct cannulation (113 ± 39.4 vs. 68.2 ± 26 seconds, p < 0.01), and instrument spatial navigation (22.1 ± 10.1 vs. 16.1 ± 2.4 seconds, p < 0.05). The number of errors to task completion was also higher, on average, for group A than for group B and reached statistical significance on three of the six laparoscopic tasks: rope passing (2 ±1.9 vs. 0.3 ± 0.4, p < 0.01), instrument spatial navigation (0.3 ± 0.5 vs. 0, p < 0.05), and suturing (1.71 ± 1.4 vs. 0.3 ± 0.5, p < 0.001). In fact, for both the rope passing and suturing tasks performed under 2D imaging, errors averaging more than three times the same tasks in 3D were observed (Fig. 2B). For the experienced participants, the time and errors to task completion were not statistically different at the first testing session between 2D and 3D imaging for all laparoscopic tasks (Table 3). However, with respect to all six tasks, the time to task completion was shorter for 3D compared to 2D, especially regarding the suturing time.
Effects of 3D (hatched bars) and 2D (open bars) imaging on the performance of inexperienced participants during the first training session. Values are expressed as the mean ± SEM in the time-to-task completion (A) and number of errors to task completion (B). Compared to 2D, participants performed better using 3D imaging with regard to speed and accuracy of task completion. *p < 0.05; **p< 0.01; ***p< 0.001
The learning curve patterns for inexperienced participants initially tested using 2D imaging were different compared to those tested using 3D imaging. For example, under 2D imaging statistically significant differences between the first and last scores for time and/or errors to task completion were noted for the following laparoscopic tasks: peg drop (first to last score, 18 seconds, 0.5 errors, p < 0.05); ring board exchange (first to last score, 0.8 errors, p < 0.05); rope passing (first to last score, 23 seconds), and duct cannulation (first to last score, 57 seconds, p < 0.05). By comparison, inexperienced participants initially tested using 3D imaging quickly reach a statistically stable performance level (i.e., no significant difference between the first and last scores, p > 0.05) on all tasks except one: peg drop (first to last score, 22 seconds, p < 0.05). Experienced participants showed no significant difference between the first and last scores for all six tasks using either 2D or 3D imaging for either times or errors to task completion (p > 0.05), indicating the absence of a learning curve for these tasks (data not shown).
Time interval between testing sessions
A given period of time was allowed to elapse before each participant was retested on the same six laparoscopic skills in an attempt to eliminate the persistence of any laparoscopic skills acquired from the initial testing session into the subsequent testing session. This period of time was defined as the washout period. For the inexperienced participants, the washout period was 80.1 ± 13.3 days. There was no significant difference in the washout periods between the inexperienced groups (A vs. B) (Table 1a). For the experienced participants, the washout period was 131.1 ± 19.8 days. Again, no statistically significant difference was noted between the washout periods for the experienced groups (C vs. D) (Table 1b).
Testing session two
Evaluation of the second testing scores revealed no statistically significant difference in the average times or errors to task completion on all six laparoscopic tasks between the inexperienced participants reassigned to 3D imaging (group A) during the second testing session compared to those reassigned to 2D imaging (group B) (Fig. 3). Statistical evaluation of the second testing session for the experienced participants showed a significant difference in the mean performance time to task completion under 3D imaging compared to 2D imaging for only one task: duct cannulation (38 ± 6.5 vs. 62.8 ± 22.8 seconds, p < 0.05).
Effects of 3D (hatched bars) and 2D (open bars) imaging on the performance of inexperienced participants during the second training session. Values are expressed as the mean ± SEM in the time-to-task completion (A) and number of errors to task completion (B). Any significant comparison showed that subjects performed equally well in the second set regardless of the imaging system tested
Importantly, the sequence of imaging testing appeared to influence the performance time and errors to task completion for the inexperienced participants. For example, the 2D testing scores for the group of inexperienced participants during the second testing session after receiving 3D imaging in the first testing session (group B) were significantly better than the 2D imaging scores of their inexperienced counterparts during the first testing session (group A) on five of the six laparoscopic tasks: peg drop (54.4 ± 15.8 vs. 81.4 ± 29.6 seconds, p = 0.019), ring board exchange (77.0 ± 21.2 vs. 121.2 ± 60.6 seconds, p = 0.016), rope passing (69.3 ± 19.3 vs. 95.9 ± 35.4 seconds, p = 0.050), duct cannulation (81.1 ± 27.6 vs. 113.0 ± 39.4 seconds, p = 0.042), and suturing (0.6 ± 0.4 vs. 1.8 ± 0.4 errors, p = 0.004). In contrast, the 3D scores for the subgroup of inexperienced participants during the second testing session after 2D imaging in the first testing session (group A) did not differ from the 3D scores during the first testing session of their inexperienced counterparts (group B) on any of the tasks. The value of initially training inexperienced participants on 3D imaging tasks was even more dramatically evident when we compared the total time effects of the crossover from 3D to 2D imaging and from 2D to 3D imaging. Combing all six tasks, the total 2D imaging times to task completion of those inexperienced participants who crossed from 3D to 2D were 181.2 seconds lower than those who began with 2D tasks (p = 0.002). In contrast, the total 3D imaging times to task completion of those inexperienced participants who crossed from 2D to 3D were only 9.6 seconds lower than those who began with 3D imaging tasks (p = 0.84).
Discussion
Surgical training programs utilize various two-dimensional (2D) laparoscopic imaging systems for the acquisition and refinement of surgical skills in the preclinical setting. Potential educational and outcome benefits have brought increasing attention to this area given the fact that one of the principal problems in laparoscopic training is the significant time, commitment, and practice needed to adapt to a 2D surgical field. Compared with direct normal vision, surgical task performance using current 2D imaging systems has been shown to be impaired 35% to 100% [1, 2]. 3D laparoscopic simulators have been developed in an attempt to overcome the problem with 2D imaging by restoring the perception of depth, thereby enabling subjects to gauge the relative position of objects and instruments in space more accurately. As a result, teaching laparoscopic skills using 3D visual conditions might be one way to facilitate learning, especially for inexperienced or untrained surgeons. However, over the years conflicting data have been generated with respect to whether 3D imaging improves laparoscopic skill performance [5–13]. These disagreements in the observations and findings seem to be dependent not only on the laparoscopic experience of the study participants but also on the 3D imaging system used for testing, methodologies, study group sample size, and the number and type of laparoscopic tasks tested. For example, Jones and colleagues found no significant difference in laparoscopic skills performance among novice and experienced individuals asked to complete five laparoscopic tasks, in random order, using both 2D and 3D imaging systems [8]. On the other hand, Pietgen and colleagues found that 3D imaging significantly improved performance compared to 2D among a group of 60 individuals with varying laparoscopic experience tested on only two laparoscopic tasks [9].
Several factors have also been shown to influence laparoscopic performance significantly: age, sex, hand dominance, and prior laparoscopic experience [3, 14, 15]. In the present study, these potential confounders were equal for the compared groups. Because the tasks performed and the instruments used were also identical for the two groups, we were able to assess independently the impact of the imaging system alone on laparoscopic skill performance. Moreover, our crossover study design was chosen because it can provide unbiased estimates for the difference between the imaging systems [16].
Performance of laparoscopic simulator skills requires a wide variety of physical aptitudes. Thus, diverse simulator tests are needed to assess accurately one’s laparoscopic abilities. However, most previous study designs comparing laparoscopic skill performance on 2D and 3D imaging systems have not utilized more than two laparoscopic skill tests [5, 6, 9–12]. In our study we were able to test the performance characteristics of six laparoscopic tasks, each of which required a different set of coordination skills. One of our first observations was that the time and error patterns to task completion for inexperienced subjects were nearly identical to those of experienced subjects. For example, the instrument spatial navigation task was apparently the easiest task in terms of time and errors to task completion for all participants regardless of the imaging system used. In contrast, the suturing task took the longest time overall and had the most errors. This, in our opinion, was the most challenging and complicated task requiring superior technical skill abilities. The rope-passing task was similar to other tasks, such as the peg drop, with respect to time but had a large number of errors, similar to the suturing task.
From the first testing session, our results demonstrated that 3D imaging greatly facilitated the initial performance of laparoscopic tasks with regard to speed and/or accuracy of completion for individuals with little or no laparoscopic experience, especially on tasks that demanded dexterity in both hands for successful completion of the task. For example, the ring board exchange task was completed 45% faster using 3D imaging with two times fewer errors compared to 2D imaging. In contrast, although faster times to task completion were noted using 3D compared to 2D imaging in the first testing session for those individuals with laparoscopic experience, none of these differences were statistically significant. This nonsignificant difference may be partially due to the smaller sample size compared to the inexperienced participants or the fact that most of the experienced participants not only have learned the form and function of the laparoscopic instruments but also are able to reconstruct 3D images from the 2D images and their fundamental monocular depth clues.
Different learning curves have been shown for the acquisition of laparoscopic simulator skills [17–19]. Although more repetitions of each task could have been provided to each participant, we found that inexperienced participants initially assigned to 3D imaging during the first testing session not only performed each task faster but also had a more rapid rate of learning compared to those initially tested on the 2D imaging. This points to the potential usefulness of the 3D imaging simulators ultimately to shorten the training time needed for laparoscopic skill acquisition for inexperienced individuals, but this warrants further investigation.
Without practice, studies have shown that individuals lose acquired laparoscopic skills over time. Torkington and colleagues showed a 25% decrease in skill over 3 months [20], whereas Windsor and Zoha showed an 81% loss of acquired skills after only 1 month [4]. In our study, approximately 3 months was allowed to elapse before retesting the subjects on the laparoscopic tasks using the opposing imaging system in an attempt to minimize the likelihood of any acquired laparoscopic skills from the first testing sessions being carried over into the second testing session. However, it was not possible to suspend the participants operating commitments for months between testing sessions. This meant that the participants of our study, especially the experienced participants, had ongoing opportunities to maintain their laparoscopic skills.
The results from the second testing session demonstrated no significant difference in performance time or error rates using 3D imaging compared to 2D imaging for those individuals with little or no laparoscopic experience. This observation was due to the improved performance on the 2D imaging tasks during the second testing session for individuals who had 3D imaging testing during the first testing session. In other words, there appeared to be a sequence effect. A sequence effect refers to a change in the measured outcome as a result of the order in which the testing on the imaging systems was administered [16]. For example, we found that when inexperienced participants were assigned to 3D imaging during the first testing session and then 2D imaging during the second testing session (group B) the performance scores using 2D imaging improved by nearly 30% compared to the 2D imaging scores of the participants originally assigned to 2D imaging in the first testing session (group A). In contrast, when the testing order was from 2D imaging during the first testing session to 3D imaging during the second testing session (group A), the scores for the inexperienced participants on the 3D imaging system were essentially the same as the 3D imaging scores for group B. Thus, our study suggests that for inexperienced individuals initial practice using 3D imaging to perform laparoscopic simulator skills results in a positive transfer of motor skills when switching to 2D imaging so that one’s laparoscopic performance is ultimately improved. If this improvement was due to greater familiarity with the testing procedure, we should have seen an improvement in the 3D tasks during the second testing session for those having initial 2D practice during the first testing session. However, initial 2D practice did not improve 3D imaging laparoscopic skill performance. Therefore, in light of this potential impact on laparoscopic education, we believe that the integration of 3D imaging systems into educational programs may lead to more efficient teaching of laparoscopic skills to those surgical trainees who appear to have difficulty acquiring a performance criteria level using the distorted visual information obtained from 2D views. Further experiments are needed to explore acquisition and learning enhancements due to 3D imaging.
The use of 3D imaging technology in laparoscopic surgery remains a fascinating but expensive technology. Although it is common sense that an improved visual system is likely to make any laparoscopic task easier, the benefits of 3D imaging remain unsettled. We believe that this two-treatment, two-period study design demonstrated that 3D imaging makes the initial performance and learning of laparoscopic tasks easier, quicker, and less prone to errors over traditional 2D imaging for inexperienced or untrained individuals. Moreover, for inexperienced individuals, the use of 3D imaging facilitated the education of laparoscopic skills by improving their performance using 2D imaging. However, not all participants in our study benefited equally from practice using 3D imaging. The experienced group, whose subjects already possessed laparoscopic familiarity, showed little difference in the performance of all tasks irrelevant of optical conditions, testing sequence or testing session. The fact that the experienced groups showed only minor improvement with changing optical conditions essentially points to the expected: that experienced laparoscopic surgeons have already adapted to the lack of depth perception inherit in the 2D imaging systems. Despite these important findings, we cannot state at this point what effect 3D imaging has on operative performance. Hanna and colleagues showed that 3D imaging systems show no advantage over 2D imaging in the conduct of laparoscopic cholecystectomy [21]. However, more clinical studies are needed to assess whether newer 3D visual enhancements can decrease laparoscopic operating times and costs and minimize morbidity for all laparoscopic procedures.
References
Taffinder N, Smith SG, Huber J, et al. (1999) The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13:1087–1092
Perkins N, Starkes JL, Lee TD, et al. (2002) Learning to use minimal access surgical instruments and 2-dimensional remote visual feedback: how difficult is the task for novices? Adv Health Sci Educ 7:117–131
Risucci D, Geiss A, Gellman L, et al. (2001) Surgeon-specific factors in the acquisition of laparoscopic surgical skills. Am J Surg 181:289–293
Windsor JA, Zoha F (2005) The laparoscopic performance of novice surgical trainees: testing for acquisition, loss, and reacquisition of psychomotor skills. Surg Endosc 19:1058–1063
Chan AC, Chung SC, Yim AP, et al. (1997) Comparison of two dimensional vs. three dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Thomsen MN, Lang RD (2004) An experimental comparison of 3-dimensional and 2-dimensional endoscopic systems in a model. Arthroscopy 20:419–423
McDougall EM, Soble JJ, Wolf JS Jr, et al. (1996) Comparison of three-dimensional and two-dimensional laparoscopic video systems. J Endourol 10:371–374
Jones DB, Brewer JD, Soper NJ (1996) The influence of three-dimensional video systems on laparoscopic task performance. Surg Laparosc Endosc 6:191–197
Peitgen K, Walz MV, Walz MV, et al. (1996) A prospective randomized experimental evaluation of three dimensional imaging in laparoscopy. Gastrointest Endosc 44:262–267
Hanna GB, Cuschieri A (2000) Influence of two-dimensional and three-dimensional imaging on endoscopic bowel suturing. World J Surg 24:444–449
Bhayani SB, Andriole GL (2005) Three-dimensional (3D) vision: does it improve laparoscopic skills? An assessment of 3D head-mounted visualization system. Rev Urol 7:211–214
Sun CC, Chiu AW, Chen KK, et al. (2000) Assessment of a three dimensional operating system with skill tests in a pelvic trainer. Urol Int 64:154–158
Byrn JC, Schluender S, Divino CM, et al. (2007) Three dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System. Am J Surg 193:519–522
Powers TW, Bentrem DJ, Nagle AP, et al. (2005) Hand dominance and performance in a laparoscopic skills curriculum. Surg Endosc 19:673–677
Grantcharov TP, Bardram L, Funch-Jensen P, et al. (2003) Impact of hand dominance, gender and experience with computer games on performance in virtual reality laparoscopy. Surg Endosc 17:1082–1085
Reed JF (2004) Analysis of two treatment, two period cross trials in emergency medicine. Ann Emerg Med 43:54–58
Grantcharov TP, Bardram L, Funch-Jensen P, et al. (2003) Learning curves and impact of previous operative experience on performance on virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185:146–149
Everbusch A, Grantcharov TP (2004) Learning curves and impact of psychomotor training on performance in simulated colonoscopy: a randomized trial using a virtual reality endoscopy trainer. Surg Endosc 18:1514–1518
Fraser SA, Freldman LS, Stanbridge D, et al. (2005) Characterizing the learning curve for a basic laparoscopic drill. Surg Endosc 19:1572–1578
Torkington J, Smith SG, Rees B, et al. (1001) The role of the basic surgical skills course in the acquisition and retention of laparoscopic skills. Surg Endosc 15:1071–1075
Hanna GB, Shimi SM, Cuschieri A (1998) Randomized study of the influence of two dimensional versus three dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251
Acknowledgment
We thank Viking Systems (La Jolla, CA, USA) for allowing us to use their 3Di Digital Visual System for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Votanopoulos, K., Brunicardi, F.C., Thornby, J. et al. Impact of Three-Dimensional Vision in Laparoscopic Training. World J Surg 32, 110–118 (2008). https://doi.org/10.1007/s00268-007-9253-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9253-6