Abstract
Background
Day-surgery laparoscopic cholecystectomy (LC) should be the procedure of choice in patients with symptomatic gallstone disease. This article assesses feasibility, patient outcome and predictive factors for successful day-case laparoscopic cholecystectomy.
Method
A retrospective analysis of our prospective database of 176 patients following laparoscopic cholecystectomy in a day-surgery unit was performed. A telephone interview was conducted within 24 h after discharge and again after 3 weeks.
Results
Of the 176 cases included in this study, 74% had biliary colic, cholecystitis (16%), pancreatitis (8%), and jaundice (2%). In addition to LC, nine patients (5.1%) underwent laparoscopic bile duct exploration and ten (5.7%) had an additional procedure performed. Eighty-six percent of the patients were discharged the same day. Multivariate analysis identified risk factors affecting same-day discharge, including age greater than 50 years and intraoperative complications. Bile duct exploration reduced the odds of discharge but did not reach significance. Postoperative telephone interviews identified high patient satisfaction with 86% of respondents recommending LC as a day-surgery procedure.
Conclusion
Day-surgery LC is a safe procedure with an acceptable rate of patient discharge. However, intraoperative complications or age over 50 years adversely affected the same-day discharge rate and as such should be taken into consideration when planning day-case laparoscopic cholecystectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As part of the National Health Service (NHS) Plan in the UK, 75% of all elective surgery is expected to be performed as day surgery [1]. Laparoscopic cholecystectomy (LC) is considered the gold standard treatment of symptomatic cholelithiasis. However, there have been concerns regarding day-case LC due to potentially life-threatening complications that do not become apparent within 8 h, or even 24 h [2]. Patients who underwent day-surgery LC were studied to establish predictive factors for success and to analyze the safety of LC as a day-case procedure.
Patients and methods
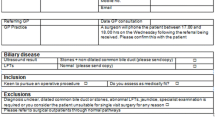
From July 2000 to January 2005 consecutive patients with both chronic and acute symptomatic gallstone disease who were eligible for day surgery underwent LC with an intraoperative cholangiogram (IOC). Median time from onset of symptoms to surgery was 6 weeks. All patients were under the care of one consultant surgeon (AGP).
Preoperatively all patients underwent blood tests (full blood count, urea and electrolytes, and liver function tests) along with an ultrasound of the gall bladder. No other preoperative testing was routinely performed.
The first 34 cases were selected in accordance with strict criteria. Patients with biliary colic only, normal liver function tests, American Society of Anaesthesiology (ASA) grade I or II, and a body mass index (BMI) of less than 35 were selected. In addition, 48-h social support was required. Patients who were asthmatic and/or unable to tolerate nonsteroidal anti-inflammatory drugs (NSAIDs) were excluded. After the first 34 cases inclusion criteria were relaxed to include all patients with symptomatic gallstone disease except those who were medically unfit, had insufficient social support, or a weight greater than 120 kg (the maximum weight for the operating table). It is important to note that abnormal preoperative biochemical and radiologic findings were not used as exclusion criteria for day surgery.
All patients were admitted on the day of surgery having been nil-by-mouth from midnight. All operations occurred before 13:00 h, with day-case surgery being defined as discharge by 20:00 h the same day.
Operative technique
Deep vein thrombosis prophylaxis using low-molecular-weight heparin (enoxaparin 40 mg) and compression stockings with additional intermittent pneumatic compression was used. Total intravenous (IV) anesthesia using propofol (125 μg/kg/min) with remifentinal (0.5 μg/kg/min) was administered for induction and maintenance. IV hydration was maintained with 2–3 L of Hartmann’s solution. Intraoperative analgesia comprised a combination of IV NSAIDs (diclofenac 75 mg) and opioids (morphine or diamorphine 10 mg). Bupivacaine (0.25%) was infiltrated locally into the wound sites (20 ml) and intraperitoneally (20 ml).
LC was performed using four ports: an open Hasson port with a subumbilical incision, and three 5-mm ports at the xiphisternum, below right costal margin in the anterior axillary line, and right of the umbilicus in the midclavicular line. An intra-abdominal pressure of 10 mmHg was maintained. An intraoperative cholangiogram (IOC) was attempted in all but the first 13 cases. Any removal of common bile duct stones was undertaken in accordance with IOC findings. In the event of bile spillage, a prophylactic dose of cefuroxime (750 mg) was given. Intra-abdominal irrigation and suction with normal saline occurred and the abdomen deflated prior to the removal of the ports.
Combination therapy was used to prevent postoperative nausea and vomiting (PONV). Typically, metaclopramide and steroids (dexamethasone 8 mg) were administered at the beginning of the procedure and a specific (5HT3) serotonin antagonist (ondansetron 4 mg) given at the end of the operation.
Patients were discharged with an analgesic package of paracetamol and codeine, and diclofenac if not contraindicated, with tramadol as an alternative. Patients were also advised to wear compression stockings for an additional four weeks postoperatively. Wound care advice and postoperative literature were provided along with out-of-hours contact telephone numbers.
Telephone interviews
Prospective telephone interviews were conducted by the nursing staff to assess patient satisfaction; an interim analysis was conducted after the first 100 patients. Contact with the patient was made within 24 h of discharge and again after 3 weeks. The interview focused on postoperative pain, return to daily activities, wound healing, and patient satisfaction.
Statistical analysis
The probability of discharge was modeled using logistic regression. Multiple logistic regression of all explanatory variables recorded and surgical complications was used to model the probability of discharge. Analyses were performed using the statistical software package Intercooled Stata Version 8 (StataCorp LP, College Station, TX).
Results
The total number of cholecystectomies performed over the study period (4.5 years) was 439. Of these, nine were performed as open cholecystectomies (for suspected malignancies), and a total of 430 were undertaken laparoscopically. Of the 254 inpatients, the median age was 52 years (range = 18–91 years) and 74% were female. Day-case LC was performed on 176 patients, the majority of which were female (90.3%). Median age for day-surgery cases was 43 years (range = 21–78 years) with 49 (28%) above the age of 50. One hundred seventy-four patients were ASA I and II while two were ASA III.
One hundred thirty patients (74%) were treated for biliary colic, 29 (16%) for cholecystitis, 14 (8%) for gallstone pancreatitis, and 3 (2%) for obstructive jaundice. Surgical procedures performed are shown in Table 1. Despite the strict inclusion criteria for the first 34 patients, with the exception of increased incidence of biliary colic within this group (p < 0.01), there was no observed difference in outcome between the two groups of patients (p = 0.09).
Bile duct exploration (BDE)
Of the nine patients who underwent BDE, there were eight transcystic explorations and one choledochotomy. Six of the transcyctic explorations were successful, with one requiring the insertion of a double J stent. Follow-up magnetic resonance cholangiopancreatography (MRCP) of these six patients showed no evidence of residual stones. In the remaining two patients transcystic exploration was unsuccessful due to difficulty in cannulating the bile duct. Subsequent tests [MRCP and endoscopic ultrasound (EUS)] revealed no residual stones.
Compared with LC only, the addition of IOC did not affect the discharge rate. On univariate and multiple logistic analyses, the odds of discharge for patients who underwent BDE were 21.4% of the odds of discharge for LC patients, i.e., the odds decreased by 78.6% if the patient underwent laparoscopic bile duct exploration; however, this did not reach statistical significance (p = 0.098).
Additional procedures (LCadd)
Ten additional procedures were performed (LCadd) during LC, as shown in Table 1. In addition to two patients requiring adhesiolysis, one underwent on-table frozen section of the gallbladder to exclude carcinoma and one patient required a liver biopsy because of visible white plaques on the liver (despite normal preoperative ultrasound). Finally, one patient was found to have an eroding giant duodenal ulcer with a large inflammatory mass with acute or chronic cholecystitis. This case was converted to a partial open cholecystectomy and partial gastrectomy with Roux-en-Y gastrojejunostomy. On analysis, an additional procedure to LC reduced the rate of same-day discharge by 75%; however, this did not reach statistical significance (p > 0.1).
Conversions to open
There were three conversions to an open procedure. In the IOC group one patient had a severely inflamed gallbladder which impaired visualization and dissection. In the BDE group a choledochotomy occurred which resulted in conversion to open because of an impacted cystic duct stone that could not be removed laparoscopically. A T tube was inserted and the patient was discharged after 8 days with no further complications. The final conversion occurred in the LCadd group because of an eroding giant duodenal ulcer as discussed above. All three conversions to open were subsequently admitted.
Operating time
Within this series the median operating time was 64 min (range = 23–389 min). However, this was not found to be a predictor of same-day discharge (p = 0.11).
Complications and admissions
In total ten complications occurred during surgery. Only one major complication occurred (bleeding following liver biopsy) which required a blood transfusion (Table 2). One patient presented one day postoperatively with abdominal pain and had developed signs of peritonitis. Despite a further laparoscopy with IOC, which revealed bile-stained fluid in the abdomen, the source of the bile leak could not be identified. In view of this, a mini-laparotomy was performed which, despite injecting methylene blue through the cystic duct, still did not reveal the source of the leak. The assumption was, therefore, that the small bile leak was from the cystic duct as no other cause for the leak could be identified. The patient made an uneventful recovery.
A total of 25 (14%) patients were admitted and seven patients were readmitted at a later date (Table 3). However, it is noted that the majority (60%, n = 15) of admissions were due to nausea, vomiting, and pain.
Univariate logistic regression found that surgical complications had a significantly adverse effect on discharge (p < 0.001), with only 10% odds of same-day discharge (Table 4). Seven of the ten complications occurred intraoperatively of which six (86%) patients were admitted. However, this did not reach significance when compared with nonintraoperative complications (Fisher’s exact test, p = 0.088).
Age
An additional factor that significantly affected rates of same-day discharge was age [p < 0.046 (multiple logistic regression adjusted for all prognostic factors)]. The odds of discharge decreased by 67% for patients over 50 years of age. Further analysis of surgical complications [OR = 0.07 (95%CI 0.02, 0.28), p < 0.001] and age [OR = 0.33 (95%CI 0.12, 0.88), p < 0.03] showed a significant effect on the outcome. While the odds of discharge decreased by 67% for patients over 50 years, this then decreased further to 92% for patients over 50 years who had surgical complications. The Hosmer and Lemeshow test confirmed that the model had a good fit [χ 2 (df,2) = 0.44, r = 0.8].
Telephone interviews
Of 100 patients, 83 were contactable in the first postoperative day and 79 during the third postoperative week. Approximately 80% of respondents reported mild to moderate pain during the first postoperative day. After three weeks 96% reported slight to no pain. During the first postoperative day 88% reported no nausea while only 2% experienced vomiting. This was reflected in their daily activity as 95% were eating during their first postoperative day and 81% had resumed normal daily activity by week 3. The majority of patients (94%) felt at ease at home. There were no major problems with wound management. Eighty-six percent of respondents would recommend the procedure as a day case. The main reasons for not recommending LC as a day-case procedure were concerns over complications, having small children at home, and not feeling ready to go home.
Discussion
Prior to the establishment of day-surgery laparoscopic cholecystectomy, 100% of cases were performed on an inpatient basis, which over the 4.5-year study period was reduced to only 45%. This study has shown that laparoscopic cholecystectomy can be successfully performed on a day-surgery basis. The discharge rate of 86% is similar to other studies [3–5]. Because this is still a relatively new procedure in day surgery within the UK, it is important to have a dedicated staff who are trained in the preparation and handling of appropriate equipment. Patient education is also vital with respect to the surgery and what to expect postoperatively.
It is important that the procedure occur in the morning to ensure sufficient postoperative recovery prior to discharge the same evening. It has been shown that LC surgery occurring after 13:00 h increases the risk of admission [6]. Key to same-day discharge is the successful control of pain, nausea, and vomiting. Intraoperatively patients received prophylactic analgesia using morphine/diamorphine and NSAIDs (diclofenac) if not contraindicated. Patients also received local infiltration and intraperitoneal bupivicaine hydrochloride. In a recent systematic review by Kehlet et al. [7], quantitative analysis of a visual analog scale (VAS) demonstrated that intraperitoneal analgesia had a significant effect when compared with placebo in the 0–6–h postoperative group (p < 0.001), although nonsignificant findings occurred for the 6–12–h group (p > 0.05) and the 12–24–h group (p > 0.05). VAS scores were significantly improved for incisional analgesia versus placebo in all groups: 0–6 h (p < 0.001), 6–12 h (p < 0.001), and 12–24 h postoperatively (p < 0.001). Systemic NSAIDs were also shown to improve VAS scores compared with placebo.
Infusion of intraperitoneal saline followed by postdeflation suctioning has been shown to significantly reduce postoperative pain [8], and irrigation of both hemidiaphragms has been effective in reducing shoulder pain [9].
Postoperative nausea and vomiting (PONV) is a complex multifactorial problem where predisposition of the patient, type of operation, types of anaesthetic agent, use of postoperative opioids, fluid administration pre- and intraoperatively [10–14], and the judicious use of antiemetics all play a part. Saunders et al. [2] examined 506 LC procedures to assess the appropriateness of same-day surgery. It was found that nausea and vomiting occurred in 32% of patients on the day of operation, with 10% suffering on the first postoperative day. Overnight admission due to PONV has been found to vary from 1% to 6% in a number of studies [4–6, 15–17]. The success of our day-surgery LC lies in the multimodal approach in managing PONV and postoperative pain. Our patients received total IV anesthesia with a combination of antiemetics, including ondansteron, cyclizine/metaclopramide, and dexamethasone. In spite of this, however, 13 patients (7%) needed admission due to persistent nausea, vomiting, over sedation, or pain. Ondansetron has been widely used in the treatment of PONV. The lowest dose recommended is 4 mg [18] and, as it is short–acting, it is best given at the end of the operation [19]. Dexamethasone has been used successfully in the treatment of chemotherapy-induced emesis. It has also been demonstrated as effective against PONV and in reducing pain, fatigue, and the duration of convalescence [20–22]. While the minimum recommended dose is 8 mg [23, 24] lower doses have been reported to be effective [25–27]. The timing of dexamethasone administration influences outcome. Wang et al. [28] found that giving dexamethasone before induction was more effective than when administered at the end of the operation. However, one side effect is the development of severe perineal discomfort and therefore it has been recommended that it be given immediately after induction [29]. Combination therapy of 5HT3 with dexamethasone has been shown to be effective [23, 30].
Our patients received 2–3 L of Hartmann’s solution intraoperatively. High fluid fusion regimes (40 ml/kg) have been associated with improved pulmonary function and exercise capacity, reduced stress response, nausea, dizziness, and fatigue, and improved same-day discharge [31]. Yogendran et al. [13] found that even a high infusion regime (20 ml/kg) 30 min preoperatively followed by 1 ml/kg/h was associated with a significantly lower incidence of thirst, drowsiness, dizziness, and nausea. However, McCaul et al. [12] found no difference in PONV after fluid challenge and, unlike Cook et al. [10], found that dextrose was associated with increased nausea, opioid requirement, and thirst.
Previous studies have shown that age was a significant predictor for admission [6, 15, 32]. However, Voitk [33] showed that day-case LC can be safely performed in the elderly (>70 years) and high-risk (ASA III) patients. Our results found that age over 50 years was associated with a significantly higher risk of admission; however, ASA grade and operative time did not significantly influence outcome. Establishing limitations to treat a very narrow spectrum of patients with symptomatic gallstone disease may improve the discharge and admission rates, but they also potentially deny surgery to patients who may benefit from day-case LC.
It is our practice to perform IOC during LC. This has the added advantage of detecting unsuspected bile duct stones and giving information about any abnormality in the biliary tree or any bile duct injury. From the IOC findings there were nine cases that required bile duct exploration (5%). This study has also shown that transcystic bile duct exploration could be performed on a day-case basis with a success rate of 66.7% and a similar discharge rate. There were no major complications in this group of patients and follow-up of the successfully performed transcyctic explorations showed normal bile ducts.
Day-case laparoscopic surgery is feasible with an acceptable discharge rate and level of patient satisfaction. The selection of patients is important in the initial development of the service in order to maintain a satisfactory rate of same-day discharge. With experience, however, selection criteria may be broadened to encompass a wider spectrum of patients. Those over 50 years of age or those with a surgical complication adversely affected discharge rates and should be taken into consideration. The success of the operation depends on well-trained staff, appropriate patient education, and skillful operative technique together with safe anesthesia.
References
Department of Health (2000) The NHS Plan. London, Stationary Office
Saunders CJ, Leary BF, Wolfe BM (1995) Is outpatient laparoscopic cholecystectomy wise? Surg Endosc 9(12):1263–1268
Ammori BJ, Davides D, Vezakis A, et al. (2003) Day-case laparoscopic cholecystectomy: a prospective evaluation of a 6-year experience. J Hepatobiliary Pancreat Surg 10(4):303–308
Kumar A, Seenu V, Mohan N, et al. (1999) Initial experience with day case laparoscopic cholecystectomy at a tertiary care hospital in India. Natl Med J India 12(3):103–107
Smith R, Kolyn D, Pace R (1994) Outpatient laparoscopic cholecystectomy. HPB Surg 7(4):261–264
Robinson TN, Biffl WL, Moore EE, et al. (2002) Predicting failure of outpatient laparoscopic cholecystectomy. Am J Surg 184(6):515–518
Kehlet H, Gray AW, Bonnet F, et al. (2005) A procedure-specific systematic review and consensus recommendations for postoperative analgesia following laparoscopic cholecystectomy. Surg Endosc 19(10):1396–1415
Tsimoyiannis EC, Glantzounis G, Lekkas ET, et al. (1998) Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc 8(6):416–420
Cunniffe MG, McAnena OJ, Dar MA, et al. (1998) Prospective randomized trial of intraoperative bupivacaine irrigation for management of shoulder-tip pain following laparoscopy. Am J Surg 176(3):258–261
Cook R, Anderson S, Riseborough M, et al. (1990) Intravenous fluid load and recovery. A double-blind comparison in gynaecological patients who had day-case laparoscopy. Anaesthesia 45(10):826–830
Habib AS, Gan TJ (2004) Evidence-based management of postoperative nausea and vomiting: a review. Can J Anaesth 51(4):326–341
McCaul C, Moran C, O’Cronin D, et al. (2003) Intravenous fluid loading with or without supplementary dextrose does not prevent nausea, vomiting and pain after laparoscopy. Can J Anaesth 50(5):440–444
Yogendran S, Asokumar B, Cheng DC, et al. (1995) A prospective randomized double-blinded study of the effect of intravenous fluid therapy on adverse outcomes on outpatient surgery. Anesth Analg 80(4):682–686
Apfel CC, Laara E, Koivuranta M, et al. (1999) A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 91(3):693–700
Lau H, Brooks DC (2001) Predictive factors for unanticipated admissions after ambulatory laparoscopic cholecystectomy. Arch Surg 136(10):1150–1153
Leeder PC, Matthews T, Krzeminska K, et al. (2004) Routine day-case laparoscopic cholecystectomy. Br J Surg 91(3):312–316
Singleton RJ, Rudkin GE, Osborne GA, et al. (1996) Laparoscopic cholecystectomy as a day surgery procedure. Anaesth Intensive Care 24(2):231–236
McKenzie R, Kovac A, O’Connor T, et al. (1993) Comparison of ondansetron versus placebo to prevent postoperative nausea and vomiting in women undergoing ambulatory gynecologic surgery. Anesthesiology 78(1):21–28
Tang J, Wang B, White PF, et al. (1998) The effect of timing of ondansetron administration on its efficacy, cost-effectiveness, and cost-benefit as a prophylactic antiemetic in the ambulatory setting. Anesth Analg 86(2):274–282
Huang JC, Shieh JP, Tang CS, et al. (2001) Low-dose dexamethasone effectively prevents postoperative nausea and vomiting after ambulatory laparoscopic surgery. Can J Anaesth 48(10):973–977
Wang JJ, Ho ST, Liu YH, et al. (1999) Dexamethasone reduces nausea and vomiting after laparoscopic cholecystectomy. Br J Anaesth 83(5):772–775
Bisgaard T, Klarskov B, Kehlet H, et al. (2003) Preoperative dexamethasone improves surgical outcome after laparoscopic cholecystectomy: a randomized double-blind placebo-controlled trial. Ann Surg 238(5):651–660
Elhakim M, Nafie M, Mahmoud K, et al. (2002) Dexamethasone 8 mg in combination with ondansetron 4 mg appears to be the optimal dose for the prevention of nausea and vomiting after laparoscopic cholecystectomy. Can J Anaesth 49(9):922–926
Lee Y, Lai HY, Lin PC, et al. (2004) A dose ranging study of dexamethasone for preventing patient-controlled analgesia-related nausea and vomiting: a comparison of droperidol with saline. Anesth Analg 98(4):1066–1071
Coloma M, White PF, Markowitz SD, et al. (2002) Dexamethasone in combination with dolasetron for prophylaxis in the ambulatory setting: effect on outcome after laparoscopic cholecystectomy. Anesthesiology 96(6):1346–1350
Eberhart LH, Mauch M, Morin AM, et al. (2002) Impact of a multimodal anti-emetic prophylaxis on patient satisfaction in high-risk patients for postoperative nausea and vomiting. Anaesthesia 57(10):1022–1027
Wang JJ, Ho ST, Uen YH, et al. (2002) Small-dose dexamethasone reduces nausea and vomiting after laparoscopic cholecystectomy: a comparison of tropisetron with saline. Anesth Analg 95(1):229–232
Wang JJ, Ho ST, Tzeng JI, et al. (2000) The effect of timing of dexamethasone administration on its efficacy as a prophylactic antiemetic for postoperative nausea and vomiting. Anesth Analg 91(1):136–139
Neff SP, Stapelberg E, Warmington A (2002) Excruciating perineal pain after intravenous dexamethasone. Anaesth Intensive Care 30(3):370–371
McKenzie R, Tantisira B, Karambelkar DJ, et al. (1994) Comparison of ondansetron with ondansetron plus dexamethasone in the prevention of postoperative nausea and vomiting. Anesth Analg 79(5):961–964
Holte K, Klarskov B, Christensen DS, et al. (2004) Liberal versus restrictive fluid administration to improve recovery after laparoscopic cholecystectomy: a randomized, double-blind study. Ann Surg 240(5):892–899
Simpson JP, Savarise MT, Moore J (1999) Outpatient laparoscopic cholecystectomy: what predicts the need for admission? Am Surg 65(6):525–528
Voitk AJ (1997) Is outpatient cholecystectomy safe for the higher-risk elective patient? Surg Endosc 11(12):1147–1149
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Psaila, J., Agrawal, S., Fountain, U. et al. Day-Surgery Laparoscopic Cholecystectomy: Factors Influencing Same-Day Discharge. World J Surg 32, 76–81 (2008). https://doi.org/10.1007/s00268-007-9225-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9225-x