Abstract
Background
Gunshot injuries to the face in civilian practice are rarely reported. Potential complications in the Emergency Department can have catastrophic consequences, and inappropriate operative management of the facial soft and skeletal tissues are related to outcome.
Methods
A structured diagnostic and management approach is used in our Trauma Unit to deal with gunshot wounds to the face. A retrospective study of 55 patients who sustained gunshot injury to the face was conducted over a 6½-year period. Demographic details, mechanism of injury, and mode of presentation and management were recorded. Mortality and morbidity data were collated.
Results
There were 51 male and 4 female patients. All injuries were caused by low-velocity gunshots, except for one that was a shotgun injury. Overall, 28 of the 55 patients (50%) underwent orotracheal intubation on scene or in the resuscitation room, and 2 had cricothyroidotomy. In addition to the maxillofacial trauma, associated injuries were common. Forty patients underwent operation for maxillofacial trauma, 34 on the day of admission and the remaining 6 within 5 days of injury. Multiple operations over a 2-week period were necessary for 18 of the 40 patients. Complications directly related to the gunshot injury to the face were very limited. Mortality was related to associated injuries.
Conclusions
Gunshot injury to the face in civilian violence is a “benign” condition as long as the Patient’s airway is kept patent and hemorrhage is controlled. Early operative intervention for repair of the soft and skeletal facial structures leads to satisfactory results. Mortality directly related to the facial trauma is uncommon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gunshot injuries to the face do not usually create major resuscitation problems [1]. This is probably the reason for the scarce reporting of such injuries in the trauma literature [2]. There are cases where in-depth knowledge of the management of potential complications is necessary to avoid catastrophic consequences for the patient in the Emergency Department. In the case of gunshot injury to the face, early operative management of the injured soft and skeletal tissues of the face is also closely related to outcome [3]. The purpose of this study is to highlight the arising challenges in the resuscitation room and to assess our overall results of the early management of patients with gunshot injuries to the face.
Patients and methods
This is a retrospective study of 55 civilian patients who sustained gunshot wounds to the face and were treated at Milpark Hospital, a Level 1 trauma center of the University of the Witwatersrand, between January 1999 and July 2005. The trauma resuscitations were conducted by the specialist trauma surgeon on call with an average response time of 10 min. Operative management of maxillofacial trauma during the period of the study was provided by the same maxillofacial surgeon. At the trauma center there is full cover of all other relevant specialties with a response time of approximately 30 min.
The medical records of the patients with gunshot injury to the face were reviewed with respect to demographics, initial evaluation, management, and outcome. “Face” was defined as the area below the eyebrows and zygomatic arches superiorly, the chin inferiorly, and the vertical ramus of the mandible posteriorly. The facial injuries were grouped as lower face (mandible and tongue), mid-face (maxilla, lower portion of nose and zygoma), and upper face (orbits and nasoethmoid complex).
Airway management was our first priority. Definitive airway control was established when the airway was compromised by hemorrhage, swelling, patient combativeness, or low Glasgow Coma Scale from concomitant brain injury. The patient’s mouth was cleansed of all debris, blood, and fragments of bone or teeth, and airway control was established immediately by orotracheal intubation. Nasotracheal intubation was never attempted. When it was not possible to establish a definitive airway, cricothyroidotomy was performed. Tracheostomy was never performed in the Emergency Department but only in the operating room as a primary procedure or as conversion from endotracheal intubation or cricothyroidotomy.
Extensive gunshot injury to the middle or base of the tongue constituted an indication for prophylactic intubation, even in the absence of any of the above indications for intubation. We have observed that this type of injury is sometimes followed by severe edema leading to complete obstruction of the oropharyngeal cavity within a few hours of admission. In such a case, the patient was extubated in 24 h if there was no evidence of obstruction and the airway could be maintained.
After securing the airway and completing the primary survey, a detailed physical examination of the patient followed. The face was inspected for contusions, abrasions, lacerations, swelling, nerve fallout (particularly cranial nerves V and VII), and obvious bruising and bleeding. It was palpated for bone discontinuity, surgical emphysema, and range of movement of the temporomandibular joint. The oral cavity was examined for foreign bodies; lacerations; hematomas; avulsed, missing, or fractured teeth; and dental occlusion. Oral examination also included examination of salivary gland ducts and orifices as well as palatal examination. Bleeding of the face was controlled by suturing or a combination of packing and suturing. Torrential bleeding from the oral cavity was controlled by tight packing of the cavity with one or even more abdominal swabs—after the patient was intubated. In certain circumstances nasal packing was also practiced. In cases of heavy bleeding, packing was occasionally followed by angiography and embolization; however, in most instances simple removal of the packs after 24 to 48 h was not followed by bleeding. This led to the practice of doing angiography in the acute phase only if the torrential bleeding was not controlled by packing or if it recurred after removal of the packs. Injury of the salivary duct or facial nerve was not repaired primarily but later on a semi-elective basis.
Facial x-rays were not taken, but all patients had x-rays of the cervical spine coupled with computed tomography (CT) scans when indicated. The radiological assessment of the facial injury relied on spiral CT scan with 3-dimensional CT reconstruction. A CT scan of the brain was performed in all patients with altered level of consciousness or if the bullet trajectory was near the base of the skull. Diagnostic angiography was performed if there was any suspicion that the bullet had crossed zone III of the neck. With the recent availability of a last generation CT scanner in our hospital (64 slices), diagnostic angiography gave place to CT angiography. In certain cases gastrografin swallow and/or endoscopy were performed to exclude injuries to the pharynx or upper esophagus. All patients were given iv augmentin, 1.2 g on arrival.
On assessing patient management, conservative versus surgical treatment was evaluated, as was the timing (early, delayed) of necessary surgical procedures. Concomitant injuries and their management were also recorded. Complications related to infection, bone healing, and function were recorded with a mean follow-up of 2½ years.
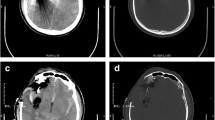
Patients with open wounds intra- or extraorally, active bleeding for any facial fracture and/ or discontinuity of bone, particularly in cases threatening the airway with obstruction, were immediately operated on (Fig. 1A). All other patients had debridement and drainage as soon as possible on the day of admission or the next day. If there was a mandibular bone continuity defect threatening the integrity of the patient’s airway, a reconstruction plate was immediately placed to bridge the defect. This plate served to re-establish the mandibular continuity and to afford correct soft tissue drape. In all such cases a titanium prosthesis was used. Our protocol for reconstruction includes leaving the prosthesis in situ even after grafting is completed. Thus the plate is removed only at the patient’s request. Because of the possibility that the plate will be in situ for a long time, titanium is favored over stainless steel because of its known biocompatibility. This was replaced by a bone graft 6–8 weeks later. We prefer indefinite retention of the reconstruction plate. Graft procedures involved particulate cancellous bone and marrow, combined with autogenous protein rich plasma, placed into a soft tissue bed with continuity to resident bone at either end. All grafts were harvested from the anterior iliac crest and were placed extra-orally (Fig. 1B). The presence of gross contamination, infection, extreme comminution, and physiological instability precluded definitive operative management within the first 24 h after admission. The presence of extensive edema was also an indication for definitive operation on the 5th day postadmission when the edema had settled. Tracheostomies were performed at any time if the airway was compromised because of the initial injury or as a necessary adjunct to operative management.
Where appropriate, psychiatric consultation was obtained during the postoperative period.
Results
During the period of this study, a total of 3.930 trauma patients were admitted to the Milpark Hospital Trauma Unit. Of these 684 (17.4%) had gunshot wounds, and 55 had sustained gunshot wounds to the face (8% of the all patients with gunshot patients and 1.4% of all admitted trauma patients). With the exception of a single patient who had sustained a shotgun injury to the face, all of the injuries were from low-velocity guns (Fig. 2).
Of the patients included in this study, 51 were men and 4 were women (mean age: 36.2 years). The age range of the men was 17–84 years (mean: 35.6 years) and that of the women was 28–63 years (mean: 44 years) (Fig. 3). The injury was a result of a crime in 38 (69.1%) patients and a suicide attempt in 15 (27.3%) patients; in 2 patients (3.6%) the injury was accidental. Of the 51 male patients, 12 (23.5%) had attempted suicide, whereas this was the case in 3 of the 4 female patients.
On scene, the systolic blood pressure of the 55 patients in our study was systolic between 80 and 90 mmHg in 4 patients and more than 90 mmHg in 41; there were no records in 10. In all patients other than the one with the shotgun injury, there was no deterioration of the systolic BP reading recorded in the resuscitation room compared with the reading taken on scene. All patients were rendered normotensive after hospital resuscitation. Eighteen of the 55 patients (32.7%) were intubated on scene, 10 patients (18.2%) were intubated in the resuscitation room, and 2 patients (3.6%) underwent cricothyroidotomy. Overall, 30 of the 55 patients (54.5%) had to have definitive airway control on scene or in the resuscitation room (Fig. 4). Six of these patients had to be intubated for concomitant head injury with a low GCS score. Of the 28 patients who underwent intubation (Fig. 4) 6 had emergency tracheostomy immediately after resuscitation; 11, at a later stage. Of the 23 patients who were initially managed by oxygen administration via facial mask, 6 patients underwent tracheostomy at a later stage as an adjunct to the operative management of their facial bone injuries. Both patients who had the cricothyroidotomies performed in the resuscitation room were later converted to tracheostomies. All tracheostomies were performed in the operating room.
The average time of resuscitation was 40 min (range: 10 min to 1 h 53 min). This does not include 2 patients whose resuscitation time was 3 h 32 min and 3 h 50 min, respectively. The first patient had sustained a shotgun wound with complete destruction of the lower face, and the second patient had concomitant multiple gunshot wounds in other areas of the body.
All but 4 of the patients were admitted to Trauma ICU/Trauma High Care.
Thirty-seven patients sustained a single gunshot wound, and 18 sustained more than one. In the first group there were 19 associated injuries: involvement of the neck in 11 patients (one with fracture of C1/2), the brain in 6, the scapula in 1, and the glenohumeral joint in 1. In the second group of 18 patients there were 33 associated injuries: 5 of the neck, 3 of the brain, 14 of the upper limbs, 3 of the lower limbs, 2 of the pelvis, 4 of the thorax (one of them with lung contusion), 1 of the back and of the thoracic spine.
Sixteen patients sustained combined face and neck trauma. In 14 of those patients the injury resulted from a single bullet; in the other 2, the face and neck had separate wounds. Eight of the 16 patients underwent emergency exploration of the neck. There was a significant number of vascular injuries, 3 involving the carotid artery, 1 the internal jugular vein, 2 the subclavian arteries, 1 the subclavian vein, 2 the facial artery, 1 the maxillary artery, and 4 the vertebral artery. Three of these injuries were dealt with by interventional radiology.
Forty-four of our patients sustained maxillofacial fractures, the remaining 11 only soft tissue injuries. The soft tissue injuries sustained in 6 of these 11 patients were to the nose (3 patients), eyelid (2 patients), tongue, tonsil, facial nerve, pharynx, lip, and ear (each in 1). The remaining 5 patients sustained only minor soft tissue injuries. The injured facial nerve was marked for later repair.
In this series of patients with gunshot wounds to the face, peripheral nerve injuries were not very common. However, injuries to the facial nerve, and to a lesser extent the mandibular branch of the trigeminal nerves, were not unexpected. Our protocol is for later nerve repair. Table 1 shows the overall number and the type of facial fracture in our patients. Table 2 shows the number of patients who sustained significant local injuries from the bullet that caused the facial trauma and the type of those injuries.
Retained bullets were not uncommon (24 [46%] of our patients). In 7 patients the retained bullet was in the neck; in 2, the brain; and in 1 each, the scapula, glenohumeral joint, zygoma, maxilla, mandible, temporomandibular joint, jaw, tongue, and mastoid. In 2 patients the anatomical area of the retained bullet was not recorded. Shrapnel was present in 21 other patients.
Four patients were transferred to other hospitals for administrative reasons after physiological stabilization. Two of them were put on mask and two had to be intubated.
Apart from the operations related to airway management, 40 patients underwent operations for facial trauma (71 operations) and 15 patients had operations at other anatomical areas (23 operations). Of the 40 patients who underwent operations for facial trauma, 34 underwent surgery the same day which always involved debridement and control of bleeding. In those patients where immediate soft tissue coverage could be obtained without creating flaps or compromising further localized blood supply to the bone, reduction and plating was carried out. This was done in order to afford bone continuity and stabilization of the associated soft tissues. Creation soft tissue flaps in low-velocity injuries is rarely a necessity. When required, local rotation flaps sufficed. The high-velocity shotgun injury was treated with a radial forearm flap. The remaining 6 patients were treated within 5 days of injury. Of the 40 patients, 18 required multiple operations over a 2-week period. In this group the bone injuries were panfacial and/or involved extensive soft tissue destruction and/or delayed presentation, requiring repeated debridement of hard and soft tissue, and a staged repair involving soft tissue flaps with the assistance of the plastic and reconstructive surgeon. Dental hard tissues deemed not salvageable at the initial operation were removed as part of the debridement. The patients were referred for dental rehabilitation when ambulant.
Twelve patients developed complications directly related to the facial injuries within the first month. These were wound infection (5), fistula or sinuses (4), osteomyelitis (1), sepsis due to a broken tooth (1), unilateral hearing loss (1), and enophthalmos (1). Twenty-two patients developed a total of 38 complications not related to the facial injury. Although injuries and the subsequent treatment to the lower third of the face resulted in limited mouth opening because of disuse and/ or muscle injury, a combination of elastic therapy, physiotherapy, and mouth-opening appliance therapy remedied this problem. The later stages of treatment encompassed a multidisciplinary approach that included dentist, prosthodontist, orthodontist, and speech and hearing therapists.
There were 4 deaths, which all took place in Trauma ICU (mortality 7.3 %). Within the first 24 h after admission 3 of these patients died from concomitant brain injury and 1 with gunshot injury to the pelvis died on day 14 from multiple organ failure.
Another 6 patients had concomitant brain injury. They survived their initial injuries and were discharged with a Glasgow Outcome Scale (GOS) of 3 in 2 patients, 4 in 2 patients, and 5 in 2 patients. The average hospital stay was 15 days. The average of TICU/THC days was 11 days.
Discussion
Ambroise Paré, a French surgeon, had this to say in 1572 about the inventor of gunpowder:
“A germane of obscure birth and condition, who demonstrated the use of Gunpowder to the Venetians when they warred with the Genoveses about Fossa Claudia, in the year of our Lord 1380. I think that the deviser of this deadly Engeine hath this for his recompense, that his name should be hidden by the darkness of perpetuall ignorance, as not meriting for this, his most pernicious invention, any mention from posterity.”
Historically, gunshot injuries to the face in civilian practice have not been extensively reported in the literature, in contrast to high-velocity injuries. With the recent increase of civilian violence in countries where weapons are accessible to the public, however, gunshot injury has become a common sequel of civilian human conflict. Most such injuries are due to the handgun; consequently, the low-velocity type of injury has become synonymous with civilian violence [4–6]. The socioeconomic climate in South Africa has perpetuated internal strife and violence similar to the human conflict in other countries such as Northern Ireland and Central America. A feature common to South Africa and Northern Ireland is the proximity of hospital facilities to “troubled areas” [7]. Most such cases are due to hand guns and are related mainly to assault, followed by accidental shootings, and failed suicide attempts. What is of clinical importance to the maxillofacial and oral surgeon is that low- and high-velocity missiles produce characteristic injuries [6–9]. However; no two injuries from the same type of weapon are identical. Other factors that influence injury apart from velocity, which is the key determinant, are tissue resistance, range, the mass and the missile’s ability to fragment, as well as the yaw and tumbling effect [10–12]. Contrary to gunshot wounds to the face in civilian practice, wartime patterns of gunshot injuries and treatment methods have been extensively discussed in the medical literature [11, 13–16].
Gunshot wounds of the face usually present with a frightful amount of deformity. The reason for this is the extreme concentration of vital structures compacted into a small space: the brain with its 12 cranial nerves, 4 of the 5 senses, the airway, an intricate bone configuration, the cervical spine, major blood vessels, salivary glands, and the centers for speech and deglutition. The potential for death or long-lasting effects is great.
In the present study, the most life-threatening early problem was airway compromise. A high percentage of our patients had to undergo orotracheal intubation: 33% (18 patients) on scene and 18% (10 patients) immediately on admission to the resuscitation unit. In most cases the airway was compromised as a result of bleeding or jaw instability. Only a few patients had to be intubated without clinical evidence of airway compromise, as they were combative. All but one patient underwent orotracheal intubation, and the procedure was successful without major difficulties in 27 patients.
We avoided nasotracheal intubation, not only because it is more time consuming, but also because there is a possibility of inflicting catastrophic penetration of the intracranial vault through a possible fracture of the cribriform plate. There is discussion in the literature about the practicality of administering a paralyzing agent in a difficult intubation. We were liberal in administering short-acting succinylcholine, and we did not have any adverse results. The administration of this paralyzing agent was always coupled with the availability of a cricothyroidotomy set so that cricothyroidotomy could be performed by the resuscitating trauma surgeon if intubation attempts failed. With this routine we had no adverse results from inability to secure airway control, and we never used steroids for control of airway edema, thus avoiding an increased risk of septic complications. Our patients were all extubated at the expected time, and there was no need for re-intubation for unresolved airway edema. It is worth mentioning that none of our patients were physiologically unstable when they arrived in the resuscitation unit, a fact that greatly facilitated their management. All our patients with gunshot wound to the middle or upper third of the face underwent a spiral CT scan of the brain together with the CT scan of the face (including coronal views and 3-dimensional reconstruction). The use of CT scan of the brain in patients with gunshot mid-face could be criticized, but because bullets can zigzag, we believe it to be the safest option for excluding a breach of the base of the skull. It is worth pointing out that a high GCS score does not exclude the possibility of brain injury, as a brain contusion of the frontal lobe that will not progress to a more severe injury later on. It is safest for the patient if this is detected on admission. The possibility of brain injury leads to increased alertness of the medical staff. Also, the possibility of a follow-up CT scan of the brain can be considered.
It is interesting that in this series of patients there were only two with cervical spine injury; one such injury was unstable, a situation that is not common with low-velocity injuries. Upper neck hematomas required further investigations, mainly angiography, to exclude vascular injuries requiring immediate attention. It was found in the majority of cases that the hematoma was not due to major vessel bleeding, but there were eight injuries of major vessels that necessitated exploration of the neck. Angiography and interventional radiology was practiced for bleeding of anatomical areas where clinical diagnosis is unreliable and surgical access technically difficult. McLean et al. [17] in their literature review report the efficacy of arterial embolization in controlling intra-oral bleeding as well as facial bleeding. Contrary to that, if the bleeding was mainly in the oral cavity, we were pleasantly surprised by the efficacy of tight packing of the oral cavity with abdominal swabs. This controlled the hemorrhage in the great majority of cases, rendering angiography and embolization necessary only in the few cases where bleeding recurred after removal of the packs. Torrential bleeding from the neck that was not controllable by insertion of a Foley catheter into the wound, necessitated immediate exploration for hemorrhage control. We feel that CT angiography with the new generation multi-slice CT scanners, which was used in a considerable number of our patients, will replace conventional angiography in the management of this type of injury. Although our recent experience with CT angiography was satisfactory, our series is not large enough to serve as the basis for drawing solid conclusions.
The amount of soft tissue injury produced by low-velocity missiles is considerably less than that from high-velocity weapons, an important consideration in the management of facial injuries. The extent of injury by low-velocity bullets is more predictable and usually confined to the bullet tract [1, 2]. The entrance wound is smaller than the diameter of the bullet and can be expected to heal without major scarring. The rich blood supply of the face allows conservative debridement of soft tissue injuries. In our series, most soft tissue injuries were treated by primary repair after debridement, and there was no significant infection rate.
The staged sequence of treatment as described by Behnia and Motamedi [18] stresses the importance of timing the treatment of hard and soft tissues, a factor that is dependent to a large extent on the surgeon’s judgment, the extent of injury, and the general condition of the patient. Selection of the appropriate surgical technique is as important as timing, because incorrect selection or improper application of surgical techniques may lead to infection, sequestration, wound dehiscence, graft rejection, facial deformity, and subsequent revisional operations. Such complications will prolong hospital stay and postoperative morbidity and increase treatment costs [19–21].
Surgical management of facial gunshot wounds is generally divided into three stages [19, 21]: (1) debridement, fracture stabilization, and primary closure; (2) reconstruction of hard tissues, provided soft tissue coverage is adequate; and (3) rehabilitation of the oral vestibule, alveolar ridge, and secondary correction of residual deformities. Often, more than one operation may be performed at any stage [19, 21]. Early definitive and comprehensive therapy [22–25] of the facial injury is the mainstay of treatment, and has been shown to result in lower morbidity [22–25]. As with other authors, we have found that the soft tissue attachments to the bone segments should be preserved where possible [18, 19]. In selected patients without severe comminution or infection, osteosynthesis using plates in accordance with AO-ASIF principles may be indicated and performed concomitantly with debridement and primary closure. The bony pieces must be located and reduced. Often, segments remain attached to periosteum and muscle, and in such cases, it is prudent to maintain the periosteal blood supply and tissue attachments during the application of hardware. Whatever the mode of osteosynthesis, application of arch bars for gunshot injuries of the jaws has proved to be invaluable in re-establishing arch form, occlusion, and stabilization of the dento-alveolar fragments. Local harvesting and use of regional soft tissue advancement rotation flaps for primary closure of maxillofacial soft tissue defects at the same operation have also proved beneficial from both an aesthetic and functional point of view [18]. Leaving defects open results in extensive scarring of the facial tissues, complicating subsequent surgical procedures, and it should be avoided, even in contaminated projectile wounds [19, 21]. In such situations, debridement and loose closure of the locally transferred tissue provide a better alternative [18, 21].
The overall number of significant postoperative complications directly related to the maxillofacial gunshot injuries in our series was very limited following early operative intervention.
Gunshot injury to the face in civilian violence is a “benign” condition as long as airway control and hemorrhage is achieved. Early operative intervention for repair of the soft and skeletal facial structures leads to satisfactory results. Mortality directly related to the facial trauma is uncommon. As the incidence of penetrating trauma increases in previously “immune” parts of the world, however, it is important for all surgeons to familiarize themselves with a structured approach of this type of injury leading to acceptable results.
References
Cohen MA, Shakenovsky BN, Smith I (1986) Low velocity hand-gun injuries of the maxillofacial region. J Maxillofac Surg 14:26–33
Demetriades D, Chahwan S, Gomez H, et al. (1998) Initial evaluation and management of gunshot wounds to the face. J Trauma 45/1:39–41
Dolin J, Scalae T, Mannor L, et al. (1992) The management of gunshot wounds to the face. J Trauma 33/4:508–515
Haug RH (1989) Management of low-calibre, low-velocity gunshot wounds of the maxillo-facial region. J Oral Surg 47:1192–1196
Cohen MA, Shakenovsky BN, Smith I (1986) Low velocity handgun injuries of the maxillo-facial region. J Maxillofac Surg 14:26–33
Walker RV, Frame JW (1984) Civilian maxillo-facial gunshot injuries. Int J Oral Surg 13:263–277
Whitlock RIH, Gorman JM (1978) Some missile injuries due to civil unrest in Northern Ireland. Int J Oral Surg 7:240–245
Stiernberg CM, Jahrsdoerfer RA, Gillenwater A, et al. (1992) Gunshot wounds to the head and neck. Arch Otolaryngol Head Neck Surg 118:592–597
Yuksel F, Celikoz B, Ergun O, et al. (2004) Management of maxillofacial problems in self-inflicted rifle wounds. Ann Plast Surg 53:111–117
Osborne TE, Bays RA (1991) Pathophysiology and management of gunshot wounds to the face. In Fonseca RJ, Walker RV, eds., Oral and Maxillofacial Trauma. Philadelphia, WB Saunders Company, pp 672–701
Banks P, Wilson JSP, Sanders R, et al. (1985) Gunshot wounds. In Rowe NL, Williams JL, eds., Maxillo-Facial Injuries, Edinburgh, Churchill Livingstone, pp 561–694
Gant TD, Epstein LI (1979) Low-velocity gunshot wounds to the maxillo-facial complex. J Trauma 19:674–677
Al Shawi A (1995) Open-packing method for the severely comminuted fractured mandible due to missile injury. Br J Oral Maxillofac Surg 33:36–39
Terry BC (1969) Facial injuries in military combat: definitive care. J Oral Surg 27:551–556
Morgan HH, Szmyd L (1968) Maxillo-facial war injuries. J of Oral Surg 26:727–730
Behnia H, Motamedi MHK (1997) Reconstruction and rehabilitation of short-range, high-velocity gunshot injury to the lower face. J Craniomaxillofac Surg 25:220
McLean JN, Moore CE, Yellin SA (2005) Gunshot wounds to the face—acute management. Facial Plast Surg 21(3):191–198
Motamedi MHK, Behnia H (1999) Experience with regional flaps in the comprehensive treatment of maxillo-facial soft-tissue injuries in warfare victims. J Craniomaxillofac Surg 27:256
Motamedi MHK, Hashemi HM, Shams MG, et al. (1999) Rehabilitation of war-injured patients with implants: analysis of 442 implants placed during a 6-year period. J Oral Maxillofac Surg 57:907
Motamedi MHK, Behnia H (1999) Experience with regioinal flaps in the comprehensive treatment of maxillo-facial soft-tissue injuries in warfare victims. J Craniomaxillofac Surg 27:256
Dobson JE, Newell MJ, Shepherd JP (1989) Trends in maxillofacial injuries in wartime (1914–1986). Br J Oral and Maxillofac Surg 27:441–450
Berlin R, Gerlin LE, Jenson B, et al. (1977) Local effects of assault rifle bullets in live tissues. Acta Chir Scand Suppl 477:5–48
Osborne TE, Bays RA (1991) Pathophysiology and management of gunshot wounds to the face. In Fonseca RJ, Walker RV, eds, Oral and Maxillo-Facial Trauma, vol. 2, Philadelphia, WB Saunders Company, 672–679
Williams CN, Cohen M, Schultz RC (1988) Immediate and long-term management of gunshot wounds to the lower face. Plast Reconstr Surg 82/3:433–439
Motamedi HKM (2003) Primary management of maxillofacial hard and soft tissue gunshot and shrapnel injuries. J Oral Maxillofac Surg 61:1390–1398
Acknowledgments
This work was supported by the German Ministry of Defence.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Glapa, M., Kourie, J.F., Doll, D. et al. Early Management of Gunshot Injuries to the Face in Civilian Practice. World J Surg 31, 2104–2110 (2007). https://doi.org/10.1007/s00268-007-9220-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9220-2