Abstract
Background
Troublesome fecal incontinence following a lateral internal sphincterotomy is often attributed to faulty surgical technique. However, it may be associated with coexisting occult sphincter defects. Whether continence is related to the extent of sphincterotomy remains debatable. The aim of the study is to identify fecal incontinence related to chronic anal fissure before and after lateral internal sphincterotomy and its relationship to the extent of internal anal sphincter division.
Methods
One hundred eight patients with chronic anal fissure were prospectively studied before and after lateral internal sphincterotomy. A questionnaire was completed for each patient before and after surgery with regard to any degree of fecal incontinence. Fecal incontinence severity index was assessed using the Cleveland Clinic Incontinence Score. The patients with preoperative perfect continence were randomized into two groups (46 patients in each group): Group 1 underwent traditional lateral internal sphincterotomy (up to the dentate line) and Group 2 were underwent a conservative internal anal sphincterotomy (up to the height of the fissure apex or just below it).
Results
Minor degrees of incontinence were present before surgery in 16 patients (14.8%). Results of the randomized trial revealed that temporary postoperative incontinence was newly developed in 6/92 of patients (6.52 %) who did not have it before surgery. Five of the six (10.86%) were in Group 1 one (2.17%) was in Group 2 (p = 0.039). Persistent incontinence occurred in two in Group 1 (4.35%). All of them were females. All have had a history of one or more vaginal deliveries.
Conclusion
A mild degree of fecal incontinence may be associated with chronic anal fissure at presentation rather than as a result of internal sphincterotomy. Troublesome fecal incontinence after lateral internal sphincterotomy is uncommon. Sphincterotomy up to the dentate line provided faster pain relief and faster anal fissure healing, but it was associated with a significant postoperative alteration in fecal incontinence than was sphincterotomy up to the fissure apex. Care should be exercised in female patients with a history of previous obstetric trauma, as internal anal sphincter division may further compromise sphincter function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Troublesome fecal incontinence following a lateral internal sphincterotomy for chronic anal fissure was described as common but underreported. Postoperative physiology of patients undergoing lateral internal sphincterotomy who become incontinent when compared with those who maintain continence is not reflected in detectable morphologic sphincteric differences [1]. It is often attributed to faulty surgical techniques involving division of an excessive amount of internal sphincter or inadvertent injury to the external sphincter. However, the function of the internal sphincter is disturbed in patients with chronic anal fissure due to persistent hypertonia and it may lead to a certain degree of incontinence as a feature of the condition rather than a consequence of internal sphincterotomy [2]. So, fecal incontinence after a satisfactorily performed lateral internal sphincterotomy may be associated with coexisting occult sphincter defects [3]. Whether continence is related to the extent of sphincterotomy remains debatable [4].
The aim of study was to identify fecal incontinence related to chronic anal fissure in our population, before and after lateral internal sphincterotomy and its relationship to the extent of internal anal sphincter division.
Patients and methods
All consecutive patients presenting to the surgical clinic with chronic anal fissure from May 2003 to May 2006 were considered for the trial. Full clinical assessment was done, including taking a complete history and general, abdominal, and local anal examination. Inspection of the anal and perianal areas was done for soiling, site, and number of fissures. Digital examination and anuscopy were performed in each case to confirm the diagnosis. Female patients with major obstetric injuries and patients with anal fissure who had been operated on before and in whom the fissure was associated with hemorrhoids, suspected inflammatory bowel disease, or malignancy were excluded from the study. Chronic anal fissure was diagnosed if the edges were fibrosed and indurated and the floor showed evidence of the circular muscle fibers of the internal sphincter. Skin tags or fibrous polyps may or may not have been present. The anal fissure was of more than three months duration. History of failure or intolerance to conservative treatment was obtained in all patients.
A prospective questionnaire was filled out before surgery for all patients. It included the demographic data: age, gender, and bowel habits and obstetric history in female patients. Data were collected relating to the history of anal fissure with special regard to a cause or presenting symptoms (pain, bleeding, and pruritus-ani). A special emphasis was made about fecal continence. Extreme patience was devoted to declare that symptom’s details. Fecal incontinence severity index was based on its type and frequency. It was categorized as follows: A, soiling of underclothing, seepage, and/or requirement of wearing a pad; B, lack of flatus control; and C, accidental bowel movement (liquid or solid stool). Each category was further classified into 1, often (daily); 2, occasionally (> one per week); and 3, rarely (< one per week), according to its frequency. Fecal incontinence severity was assessed according to the validated Cleveland Clinic Incontinence Score because it is practical and easy to use and interpret: 0 = perfect continence, 1–7 = good continence, 8–14 = moderate incontinence; 15–20 = severe incontinence, and 21 = completely incontinent [5].
Only the patients with a confirmed diagnosis of chronic anal fissure and preoperative perfect continence were eligible for entry into the prospective, controlled, randomized trial. Fully informed written consent was obtained from each patient prior to entry into the trial. Altogether 92 patients entered the trial. They were randomized into two groups (46 patients in each group): G1 underwent traditional lateral internal sphincterotomy (up to the dentate line) and G2 underwent a conservative internal anal sphincterotomy (up to the height of the fissure apex or just below it) depending on whether the patient’s registration number was odd or even, respectively.
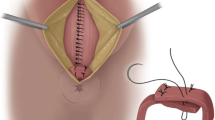
The procedures were performed with the patient under general anesthesia and in the lithotomy position. Lateral subcutaneous internal sphincterotomy was performed on the left side of the patient. Excision of the skin tag or hypertrophied papillae (if they were present) was done just before sphincterotomy. A small incision was made lateral to the lower edge of the internal sphincter, which was located by finger. A sharp Mayo’s scissor was introduced and passed up between the internal sphincter and anal mucosa with the left index finger inserted into the anus to avoid even a small violation of the integrity of mucosa. The intersphincteric groove was identified and the intersphincteric plane separated with the scissor. Then the internal sphincter was cut under direct visualization up to the level of the dentate line or up to the height of the fissure apex or just below it, according to randomization of the patient. The skin incision was partially closed with a single Vicryl suture.
Patients with preoperative incontinence underwent a conservative internal sphincterotomy. They were excluded from randomization and the comparison between the outcomes of both procedures.
Postoperative stool softener and Sitz’ baths were advised for all patients for three weeks to avoid constipation and reduce pain, bleeding, and infection.
Postoperative follow-up after the patient were discharged from the hospital was a visit every three weeks for six visits. The follow-up period of 18 weeks was chosen because complete recovery from postoperative pain and soiling takes about 8–12 weeks. At each follow-up visit, assessment of fissure healing was done by visual inspection and by asking about any pain with defecation. Another questionnaire was filled out for all patients after fissure surgery had healed, and the fecal incontinence severity score was assessed. All data were documented.
Statistical analysis
Statistical analysis was performed with the aid of the SPSS computer program (version 6.0 for Windows; SPSS Inc., Chicago, IL). Continuous variables are expressed as the mean ± standard deviation or number and percentage of patients. Statistical comparisons between the two groups were made with Student’s t test. Statistical significance was defined as p < 0.05.
Results
The mean age of the patients was 33 years (range = 16–68 years). There were 61(56.5%) women and 47 (43.5%) men. The predisposing conditions were constipation only in 47 male patients (100%) compared with 11 female patients (18%), trauma of childbirth in 23 (37.7%), and constipation and trauma of childbirth in 27 patients (44.3%). The duration of the fissures ranged from four months to five years. Pain and bleeding per anus after defecation were the main presenting symptoms in all patients; pruritus-ani was found in 42 patients (38.9%). The indication for surgery was failure of or intolerance to conservative treatment in all patients. The locations of the fissures in the anoderm are shown in Table 1. There were 67 fissures in 61 female cases and 56 fissures in 47 male cases.
Before surgery minor fecal incontinence was documented in 16 of 108 patients (14.8%) with chronic anal fissure. Soiling of underclothing due to fecal seepage was observed in nine cases (8.33 %) and lack of flatus control in seven cases (6.48%). The score of fecal incontinence severity was 2 and 3, respectively, when assessed according Cleveland Clinic Incontinence Score. This is considered good continence but not perfect. These 16 patients underwent a conservative internal anal sphincterotomy. It should be noted that preoperative fecal incontinence problems occurred in 13/61 of women (21.3%) compared with 3/47 of men (6.38 %); this was statistically significant (p = 0.043). All but two of the female patients with minor preoperative fecal incontinence had a history of one or more vaginal deliveries.
Group 1 (46 patients) underwent traditional lateral internal sphincterotomy (up to the dentate line) and Group 2 (46 patients) underwent a conservative internal anal sphincterotomy (up to the height of the fissure apex or just below it). The demographic and preoperative data in the two groups of patients were similar (Table 2).
The time required for relief of pain postoperatively in the dentate line sphincterotomy patients (G1) was significantly shorter than that for the fissure apex sphincterotomy patients (G2). The times required for objective healing in both groups of patients were not statistically significant. No treatment failures or recurrences were noted in the dentate line patients (100% healing rate), while in the fissure apex patients there were two cases of nonhealing at the end follow-up period (Table 3).
At the end of 18-week follow-up period, fecal incontinence was found in all 16 patients who were incontinent before surgery. Following conservative sphincterotomy, all of them had the same incontinence severity score as the the preoperative score. Anal incontinence developed in 6/92 of patients (6.52 %) who did not have it before surgery. Sphincterotomy up to the dentate line caused a significant change in fecal incontinence. Of 46 patients continent before surgery and who had sphincterotomy up to the dentate line, anal incontinence occurred in five of them (10.86 %) following surgery compared with only one patient (2.17%) in the conservative sphincterotomy group (46 patients) (p = 0.039) (Table 4). Following sphincterotomy up to the dentate, incontinence of liquid feces with of lack flatus control occurred in two patients and soiling of their underclothes due to fecal seepage and lack of flatus control occurred in three patients. Their fecal incontinence severity scores were 8 and 6, respectively, when assessed by Cleveland Clinic Incontinence Score. Only one patient complained of lack of flatus control following conservative sphincterotomy and had a fecal incontinence severity score of 3 (Table 5). Incontinence of solid feces did not occur in any patient. It should be noted that patients with postoperative incontinence in the two groups were females. All have had a history of one or more vaginal deliveries.
Patients with postoperative fecal incontinence complied with more than an 18-week follow-up period; three of five patients in the traditional sphincterotomy group improved. At the last follow-up visit (mean = 24 weeks), fecal incontinence with a score of 3 was present in two patients (3.57%) in the traditional sphincterotomy group and in no patient (0 %) in the conservative sphincterotomy group (p = 0.033).
Discussion
The pathophysiology of chronic anal fissure remains unresolved. Internal sphincter hypertonia is thought to prevent relaxation during defecation and it may be relevant to the pathogenesis of this disorder. Hence, relaxation of the internal sphincter permits discrimination of rectal contents by permitting them to come into contact with the sensitive anal mucosa and flatus can be expelled, whereas liquid or solid stool is retained without anal incontinence. Internal sphincter hypertonia and failure of relaxation may be the cause of minor degrees of incontinence in subjects who have not undergone sphincterotomy [5]. Incontinence found in patients who have been treated surgically for anal fissure is usually attributed to the treatment, but whether it is attributed to the sphincter abnormalities associated with the condition remains speculative [6]. Moreover, the true incidence of fecal incontinence is thought to be underestimated and only a minority of physicians actively pursue this “silent affliction,” particularly in patients who do not readily volunteer this information. Multiple factors, e.g., multipartum, increased age, constipation, and previous surgery, were identified in each of the authors’ cases of incontinence [7]. The study disclosed that 14.8% of patients with chronic anal fissure had preoperative minor degrees of fecal incontinence. The female-to-male ratio of patients with preoperative fecal incontinence problems was 13:3. This was statistically significant. All but two of those female patients had a history of one or more vaginal deliveries. Thus, an anal sphincters defect from obstetric trauma was presumed as the pathogenesis factor of fecal incontinence in them.
Lateral internal sphincterotomy is still the treatment of choice for chronic anal fissure. However, morbidity, mainly incontinence, was once thought to be extremely rare but has been substantial in some reports and seems to be permanent in a small percentage. The overall risk of incontinence was about 10% in randomized surgical trials [8, 9]. However, publications describing treatment for incontinence after sphincterotomy for fissure are strikingly absent, implying a lack of need compared with other incontinent populations [10]. Whether the extent of internal sphincterotomy should be confined to the upper limit of the fissure (conservative division) or to the dentate line (traditional sphincterotomy) remains debatable. Doing a shorter sphincterotomy corresponding to the length of the fissure reduces the risk of anal incontinence [11]. Furthermore, a more conservative division could lead to an equivalent healing rate by the time of their outpatient follow-up (mean = 6.9 weeks) [12]. Many surgeons remain skeptical, however, of the nature and impact of incontinence after anal surgery [13, 14]. Controlled sphincterotomy in three steps according to the degree of anal stenosis was reported as a way of overcoming the risk of incontinence [15]. Another report involved tailoring the division of the sphincter according to the degree of the hypertonia by anal manometry and sphincter length [16]. Others found that the influence of anal manometry before surgical management of chronic anal fissure on the outcome is probably superfluous [17]. It was reported that the closed internal sphincterotomy technique had less postoperative pain and less postoperative incontinence but the healing time of the fissure was the same as with the open technique [18]. Recent meta-analysis results demonstrating incontinence rates after sphincterotomy by both techniques seem to be equally efficacious [19, 20]. However, one advantage of the open technique in this study was that the internal sphincter is cut under direct visualization. It worth noting that the precautions made in that study regarding patients with preoperative minor fecal incontinence, by adopting a conservative sphincterotomy using the open technique, were fruitful. None of them had a postoperative incontinence severity score worse than their preoperative score.
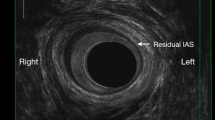
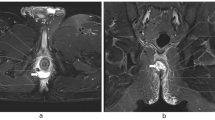
Whether surgery changes the anatomy and causes symptoms is unknown. In one study, endosonography revealed anal sphincter defects after minor anorectal surgery in 70% of patients; however, the sphincter defect did not produce symptoms [21]. The tone of the internal anal sphincter was found to increase gradually during the first year following lateral internal sphincterotomy, showing recovery, but it was still significantly less than before surgery. However, no patient suffered any permanent problems with incontinence, so this decrease in tone may not be clinically significant [22]. Other studies concluded that incontinence due to lateral internal sphincterotomy does not recover after long-term follow-up and appears to be an independent cause of fecal incontinence [23]. A longer follow-up would possibly reveal procedure-dependant incontinence, when the puborectal sling has lost is ability to compensate for continence. This study revealed that conservative division of the internal anal sphincter results in adequate fissure healing and a much lower incontinence rate (2.17%) than that previously recorded in the literature for traditional division of the internal anal sphincter (10%–35%) [8, 9, 24].
In contrast to lateral internal anal sphincterotomy in males, division of the internal anal sphincter in most females tends to be more extensive than intended. This is probably related to their shorter anal canal. Females who have had two or more previous vaginal deliveries should be warned about possible long-term flatus incontinence [24]. Care should be exercised especially in the presence of previous obstetric trauma, particularly in the presence of external sphincter defects, as internal anal sphincter division may further compromise sphincter function [25].
Although disturbances of continence after lateral internal sphincterotomy, no matter how minor, are a concern; careful patient selection, absence of preoperative continence problems, and meticulous surgical techniques are necessary to achieve good results. It should be diagnosed and performed by a surgeon skilled in proctologic surgery.
Conclusion
A mild degree of fecal incontinence may be associated with chronic anal fissure at presentation rather than a result internal sphincterotomy. Troublesome fecal incontinence after lateral internal sphincterotomy is uncommon. Sphincterotomy up to the dentate line provided faster pain relief, albeit faster anal fissure healing, but it was associated with a significant postoperative alteration in fecal incontinence than did sphincterotomy up to the fissure apex. Care should be exercised in female patients with a history of previous obstetric trauma, as internal anal sphincter division may further compromise sphincter function.
References
Zhar AP, Beer-Gabel M, Chiappa AC, et al. (2001) Fecal incontinence after minor anorectal surgery. Dis Colon Rectum 44(11):1610–1619
Ammari FF, Bani-Hani KE (2004) Fecal incontinence in patients with anal fissure: A consequence of internal sphincterotomy or a feature of the condition? Surgeon 2(4):225–229
Tjandra JJ, Han WR, Ooi BS, et al. (2001) Fecal incontinence after lateral internal sphincterotomy is often associated with coexisting occult sphincter defects: a study using endoanal ultrasonography. ANZ J Surg 71(10):598–602
Pernikoff BJ, Eisenstat TE, Rubin RJ, et al. (1994) Reappraisal of partial lateral internal sphincterotomy. Dis Colon Rectum 37(12):1291–1295
Church JM, Fleshman JW, Kane RL, et al. (1999) Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 42(12):1525–1532
Penninckx F, Lestar B, Kerremans R (1992) The internal anal sphincter: mechanisms of control and its role in maintaining anal continence. Baillieres Clin Gastroenterol 6:193–214
Johanson JF, Lafferty J (1996) Epidemiology of fecal incontinence: the silent affliction. Am J Gastroenterol 91:33–36
Khubchandani IT, Reed JF (1989) Sequelae of internal sphincterotomy for chronic fissure in ano. Br J Surg 76:431–434
Nyam DC, Pemberton JH (1999) Long-term results of lateral internal sphincterotomy for chronic anal fissure with particular reference to incidence of fecal incontinence. Dis Colon Rectum 42:1306–1310
Nelson RL (2002) Outcome of operative procedures for fissure in ano. Cochrane Database Syst Rev (1):CD002199
Landsend E, Johnson E, Johannessen HO, et al. (2003) Surgical treatment of anal fissure. Tidsskr Nor Laegeforen 123(23):3366–3367
Garcea G, Sutton C, Mansoori S, et al. (2003) Results following conservative lateral sphincteromy for the treatment of chronic anal fissures. Colorectal Dis 5(4):311–314
Lindsey I, Jones OM, Smilgin-Humphreys MM, et al. (2004) Patterns of fecal incontinence after anal surgery. Dis Colon Rectum 47(10):1643–1649
Tocchi A, Mazzoni G, Miccini M, et al. (2004) Total lateral sphincterotomy for anal fissure. Int J Colorectal Dis 19(3):245–249
Cho DY (2005) Controlled lateral sphincterotomy for chronic anal fissure. Dis Colon Rectum 48(5):1037–1041
Rosa G, Lolli P, Piccinelli D, et al. (2005) Calibrated lateral internal sphincterotomy for chronic anal fissure. Tech Coloproctol 9(2):127–131
Prohm P, Bonner C (1995) Is manometry essential for surgery of chronic fissure-in-ano? Dis Colon Rectum 38(7):735–738
Garcia-Aguilar J, Belmonte C, Wong D, et al. (1996) Open vs closed sphincterotomy for chronic anal fissure: long term results. Dis Colon Rectum 39:440–443
Arroyo A, Perez F, Serrano P, et al. (2004) Open versus closed lateral sphincterotomy performed as an outpatient procedure under local anesthesia for chronic anal fissure: prospective randomized study of clinical and manometric long-term results. J Am Coll Surg 199(3):361–367
Wiley M, Day P, Rieger N, et al. (2004) Open vs. closed lateral internal sphincterotomy for idiopathic fissure-in-ano: a prospective, randomized, controlled trial. Dis Colon Rectum 47(6):847–852
Felt-Bersma RJ, van Baren R, Koorevaar M, et al. (1995) Unsuspected sphincter defects shown by anal endosonography after anorectal surgery. A prospective study. Dis Colon Rectum 38(3):249–253
Ram E, Alper D, Stein GY, et al. (2005) Internal anal sphincter function following lateral internal sphincterotomy for anal fissure: a long-term manometric study. Ann Surg 242(2):208–211
Rotholtz NA, Bun M, Mauri MV, et al. (2005) Long-term assessment of fecal incontinence after lateral internal sphincterotomy. Tech Coloproctol 9(2):115–118
Casillas S, Hull TL, Zutshi M, et al. (2005) Incontinence after a lateral internal sphincterotomy: are we underestimating it? Dis Colon Rectum 48(6):1193–1199
Damon H, Bretones S, Henry L, et al. (2005) Long-term consequences of first vaginal delivery-induced anal sphincter defect. Dis Colon Rectum 48(9):1772–1776
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elsebae, M.M.A. A Study of Fecal Incontinence in Patients with Chronic Anal Fissure: Prospective, Randomized, Controlled Trial of the Extent of Internal Anal Sphincter Division During Lateral Sphincterotomy. World J Surg 31, 2052–2057 (2007). https://doi.org/10.1007/s00268-007-9177-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9177-1