Abstract
The aim of this study was to determine whether there was any relation between consumption of chilies and postoperative symptoms after hemorrhoidectomy in patients with grade III or IV hemorrhoidal disease. A total of 60 patients were randomly assigned to receive antibiotics and analgesics alone (control patients) or daily consumption of 3 g of chili powder along with identical antibiotics and analgesics (chili group). The evaluation of symptoms—pain, anal burning, pruritus, bleeding—during the postoperative period was assessed by means of patients’ self-questionnaires. A global score for evaluating each postoperative symptom was compared between the two groups at the 1-week follow-up. No significant difference in age, sex distribution, or grade of disease was noted between the two groups at baseline. The incidence of posthemorrhoidectomy symptoms was higher in the group consuming chilies during the first postoperative week. The global score for postoperative pain (14.60 for the chili group vs. 7.97 for the control group, p < 0.001) and for anal burning (12.90 for the chili group vs. 7.82 for the control group, p < 0.0001) were significant. Although bleeding (6.95 in the control group and 7.57 in the chili group, p < 0.81) and pruritus (8.06 in the control group and 8.75 in the chili group, p < 0.69) were more common in the chili group, the difference did not achieve statistical significance. This study shows that consumption of 3 g of red chilies per day during the postoperative period after hemorrhoidectomy increases the intensity of typical postoperative symptoms, stool frequency, and the consumption of analgesics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Indian cuisine is rich in various spices, and among them the most commonly used ingredient is chili [1] (Capsicum annuum). It is empirically believed that consumption of spices and chilies has a role in the pathogenesis or exacerbation of various anorectal disorders, mainly anal fissures and hemorrhoidal disease [2].
There are only a few studies that have demonstrated a direct relation between consumption of chilies and the development or deterioration of anorectal disease [3]. Sun-dried chilies contain capsaicin and dihydrocapsaicin, which in turn contain nitrophenols. These substances, by producing nitrosation of foodstuffs, are often believed to be gastric stimulants and are known to cause toxicity in the gastrointestinal tract [4]. Capsaicin is known to affect visceral sensory perception, and chilies have been shown to accelerate gut transit, increasing the frequency of bowel evacuation [5].
In an experimental study, it was found that consumption of red chilies produced exfoliation of intestinal epithelium in the rat lumen [6]. Chilies have been labeled an ulcerogenic food substance [7].
For the reasons mentioned above, we initiated a trial to evaluate any cause-and-effect relation between the ingestion of dried chilies and postoperative symptoms after Milligan-Morgan’s open hemorrhoidectomy. The study was a prospective, randomized, placebo-controlled, double-blind trial.
Materials and Methods
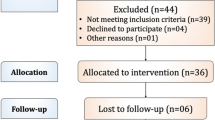
Adult patients with an indication for hemorrhoidectomy were eligible for the study, provided they met the following inclusion criteria: symptomatic, prolapsing grade III/IV hemorrhoids and informed consent. Patients with associated fistula or fissure in ano, inflammatory bowel disease, alcoholism, drug abuse, dermatitis, or proctitis were excluded from the study. Also excluded were indivicuals who were unable to understand the endpoints of the study or to complete the forms for data recording.
The study was conducted by following a randomized, control design. A total of 60 patients (23 women, 37 men) with an average age of 45 years (range 28–64 years) were recruited from February to November 2005 in our hospital. The study population was then randomly assigned by a computer-based sequential method to either posthemorrhoidectomy antibiotic and analgesic therapy plus placebo (described below) (control group, n = 30) or identical antibiotic and analgesic therapy plus chilies (chili group, n = 30).
Preparation of Capsules of Chilies and Placebo
After analyzing cookbooks from five expert cooks and the medical literature [1], it was estimated that about 1.5 g of dried chili powder must be added to a normal dish to make it spicy enough. Therefore, this amount of chili was placed in a capsule. The capsules were prepared by an independent pharmacy not attached to the hospital. Capsules were numbered consecutively, but the sequence of placebo and chili powder was randomized. The chili powder, which contained ground sun-dried red chilies, was obtained through a commercially available pack of chili powder approved by the Food and Drug Administration in India.
The active capsule contained 1.5 g of chili powder and 0.5 g of lactose-free microcrystalline cellulose. Placebo capsules contained 2 g of microcrystalline cellulose alone. Both capsules were colored black to prevent identification of the contents.
Surgery
A standardized general anesthesia technique was used for the surgery with thiopentone sodium and succinylcholine chloride and endotracheal intubation. A single surgeon performed all the procedures, with the patient in the lithotomy position. Patients underwent a standard Milligan-Morgan hemorrhoidectomy that consisted of retraction of the pile mass with artery forceps and radiofrequency dissection with excision. Ligature of the vascular pedicle was performed clear of the internal sphincter.
The Ethics Committee of Fine Morning Hospital and Research Center, Nagpur, approved the protocol of this study.
Drug Treatment
During the study period, patients were instructed to avoid any other food potentially related to gastrointestinal or hemorrhoidal symptoms such as spices, alcohol, tobacco, tea, and coffee. During the immediate postoperative period, 50 mg of tramadol hydrochloride was administered by the intramuscular route. Patients were routinely discharged on the first postoperative day unless otherwise indicated clinically. All patients were supplied with standard analgesic tablets containing a combination of tramadol hydrochloride 37.5 mg and acetaminophen 500 mg (Tab Acuwin; Nicholas Piramal India, Mumbai, India): two tablets orally a day or more as needed but no more than four tablets per day. The patients also received tablets containing 250 mg of metronidazole to be taken twice daily for the next 7 days. In addition, they were prescribed a fiber supplement, Naturolax (Organon India, Mumbai, India), 10 g daily, and were instructed to maintain a high fluid intake. Each patient was given a pack containing 14 capsules (containing placebo or chili powder) numbered consecutively to be taken after lunch and dinner each day for the next 7 days. Both the patients and the doctors associated with this study were unaware of the contents of the capsules.
Assessment and Evaluation of Symptoms
Patients were asked to self-assess specific symptoms and any bleeding encountered and then report back 7 days after hospital discharge. Symptoms included pain, anal burning (described as a burning sensation in the anus after defecation), pruritus, and bleeding. Each symptom was allocated a score from 0 to 3: 0, no symptoms; 1, mild; 2, moderate; 3, severe intensity. They were provided with a diary in which the patients were asked to note the pain intensity from 0 to 3; the pain intensity assessment was completed as an average for the day and the maximum pain experienced during that day. The patients also recorded the total daily number of analgesic tablets ingested, the food they had eaten on that day (food diary), and the number of stools passed each 24 hours from day 1 to day 7 during the postdischarge period. During the follow-up, the observer assessed that patients had eaten no foodstuffs that contained chilies in any form.
Statistical Analysis
A sample size calculation estimated that a minimum of 25 patients in each arm would be required to detect a difference of 1 SD increase in postoperative symptoms at a 5% significance level with a power of 95%. In our analysis, we used Friedman’s test for categorical variables as the mean scores for each symptom analyzed—pain, anal burning, pruritus, bleeding—and the Mann-Whiney U-test for continuous variables (for global scores).
The Friedman test does not allow comparison between two treatments. Therefore, a global score (GS) was constructed to compare any increase in symptoms in the chili group with those in the control (placebo) group. For each symptom the global score was calculated by adding up mean scores throughout the 7-day study period. This was done for each group (control and chili). The Mann-Whiney U-test was used to compare aggravation of the global score for each symptom in both groups over the study period. The mean frequency of stool passed and the number of analgesic tablets consumed during these 7 days was also assessed.
Results
Of the 30 patients recruited into the chili group, 3 were found to have consumed spicy food, which could have altered the results of this study, so they were excluded from the current study.
Comparison of Patient Groups
Patients were assessed at baseline for demographic characteristics, history of hemorrhoids, and hemorrhoid grade. There were no significant differences in these variables between the two groups (Table 1). No complications were recorded during the period of hospitalization.
Evaluation of Symptoms
Pain
The daily mean ± SD pain score was significantly lower in the placebo group throughout the study period (Fig. 1) (GS = 14.60 ± 2.88 in the chili group and 7.97 ± 2.28 in the control group, p < 0.001). There was no significant difference in the mean analgesic requirement during the first 24 hours (2.2 injections of tramadol in the controls and 2.4 injections in the chili group). However, patients used an average of 19 tablets (range 8–36 tablets) in the placebo group during the first 7 days after surgery compared with 24 tablets (range 17–40 tablets) in the chili group.
Anal burning
There was a significant burning sensation experienced by the patients in the chili group (GS = 12.90 ± 3.11 for the chili group vs. 7.82 ± 1.88 for the control group, p < 0.0001) (Fig. 2).
Bleeding and pruritus
The mean global scores for bleeding (GS = 6.95 ± 1.5 in control group and 7.57 ± 1.48) in the chili group, p < 0.81) (Fig. 3) and pruritus (GS = 8.06 ± 1.01 in the control group and 8.75 ± 1.65 in chili group, p < 0.69) (Fig. 4) were higher in the chili group than in the control group. The difference, however, did not reach statistical significance.
Bowel evacuation frequency
The mean number of stool evacuations over the study period was 18 for patients in the chili group and 13 for the control group.
Discussion
The epidemiologic features of hemorrhoidal disease are not well known because available studies have provided widely variable conclusions [8]. Risk factors frequently mentioned include heredity, high socioeconomic level, obesity, and smoking. A diet rich in fats, alcohol, spices, and pepper as well low fluid intake have been implicated [9]. In women, certain obstetric events have been reported to favor symptom development [10]. The role of intestinal transit has been discussed, which is maintained as influential in the rare studies examining diarrhea but subject to contradictory conclusions regarding constipation [11].
With regard to the relation of chilies and hemorrhoids, the literature is sparse, with very few articles describing the effect of pepper or chilies on hemorrhoids or hemorrhoidal symptoms. The exact mechanism by which chilies influence the colonic and rectal physiology is not well understood. Capsaicin, the pungent principle of hot pepper, has the ability to excite and later defunctionalize a subset of primary afferent neurons [12]. Chilies are known to cause rectal hyperalgesia in patients with irritable bowel syndrome [13]. A significant increase in the number of mucosal inflammatory cells and an increase in BrdU-immunoreactive nuclei have been detected following mucosal exposure to capsaicin in the colon [14]. One study showed that chili supplementation promotes colon carcinogenesis [15]. A case of small bowel obstruction and localized ileal perforation caused by an undigested green chili has been reported [16].
The most important study was that by Altomare et al. [17]. In a randomized, controlled study, they found that there is no relation between consumption of red chilies and aggravation of hemorrhoidal symptoms. However, we believe that the amount of capsicum used for their study was much less (10 mg) than what is actually contained in the usual Indian diet [18]. Second, the conclusion was made after a very short period of chili ingestion (48 hours), which we think is too brief to reach to any significant conclusion.
There are a few studies that have shown chilies to have an adverse effect in the gastrointestinal tract, causing duodenal ulcer [7], esophageal and gastric cancer [19], ileal perforation, pruritus ani [20], incisor tooth wear [21], and cancer of the abdomen [22]. A few other studies have found that spices do have an adverse effect on hemorrhoid and anal fissure symptomatology, although they did not mention chilies specifically [23].
Chilies are known to cause accelerated gut transit, increasing the frequency of stool evacuation, which itself could be a factor aggravating hemorrhoidal symptoms [24]. In our study, there was a definite increase in stool frequency in patients consuming chilies when compared to the placebo group, causing an increased incidence of anal burning and bleeding. Our study has clearly demonstrated that consumption of red chili powder increases the postoperative symptoms after hemorrhoidectomy, demonstrating a direct relation between chili consumption and hemorrhoidal symptoms. This was more significant with regard to pain and anal burning.
There are studies that have noted significant relief of anal pruritus following application of capsaicin ointment. However, most of the patients in these studies experienced a burning sensation at the site of application, indicating that chili or its extract causes burning and irritation [25, 26].
We admit that a note on the overall time for healing of the hemorrhoidectomy wound and a patient satisfaction grade between the two groups would have consolidated the conclusions of our study.
Conclusions
This study showed that consumption of 3 g of red chilies per day during the postoperative period after hemorrhoidectomy increases the extent and duration of typical postoperative symptoms (pain, anal burning, bleeding, anal itch). Consumption of chilies also increases stool frequency. Thus, it is concluded that consumption of chilies should be forbidden during the immediate postoperative period in patients who have undergone hemorrhoidal surgery.
References
Desai HG, Venugopalan K, Antia FP (1973) Effect of red chili powder on DNA content of gastric aspirates. Gut 14:974–976
Denis J (1976) A study of some etiological factors in hemorroidal disease (author’s transl). Arch Fr Mal App Dig 65:529–536
Brooks MH, Brooks R (1996) Red pepper effect. Br J Gen Pract 46:759
Mende P, Siddiqi M, Preussmann R, et al. (1994) Identification of nitrophenols as nitrosation products from capsaicin and red chilies. Cancer Lett 83:277–282
Agarwal MK, Bhatia SJ, Desai SA, et al. (2002) Effect of red chilies on small bowel and colonic transit and rectal sensitivity in men with irritable bowel syndrome. Indian J Gastroenterol 21:179–182
al-Qarawi AA, Adam SE (1999) Effects of red chili (Capsicum frutescens L) on rats. Vet Hum Toxicol 41:293–295
Lewis EA, Aderoju EA (1978) Factors in the aetiology of chronic duodenal ulcer in Ibadan. Trop Geogr Med 30:75–79
Pigot F, Siproudhis L, Allaert FA (2005) Risk factors associated with hemorrhoidal symptoms in specialized consultation. Gastroenterol Clin Biol 29:1270–1274
Jensen SL (1988) Diet and other risk factors for fissure-in-ano: prospective case control study. Dis Colon Rectum 31:770–773
Johanson JF, Sonnenberg A (1994) Constipation is not a risk factor for hemorrhoids: a case-control study of potential etiological agents. Am J Gastroenterol 89:1981–1986
Delco F, Sonnenberg A (1998) Associations between hemorrhoids and other diagnoses. Dis Colon Rectum 41:1534–1541
Abdel-Salam OM, Szolcsanyi J, Mozsik G (1997) Capsaicin and the stomach: a review of experimental and clinical data. J Physiol Paris 91:151–171
Schmulson MJ, Valdovinos MA, Milke P (2003) Chili pepper and rectal hyperalgesia in irritable bowel syndrome. Am J Gastroenterol 98:1214–1215
Hoffmann P, Mazurkiewicz J, Holtmann G, et al. (2002) Capsaicin-sensitive nerve fibres induce epithelial cell proliferation, inflammatory cell immigration and transforming growth factor-alpha expression in the rat colonic mucosa in vivo. Scand J Gastroenterol 37:414–422
Nalini N, Manju V, Menon VP (2006) Effect of spices on lipid metabolism in 1,2-dimethylhydrazine-induced rat colon carcinogenesis. J Med Food 9:237–245
Rajaratnam SS, Boyle N, Owen WJ (2001) ‘Always chew your chilies’: a report of small bowel obstruction with perforation. Int J Clin Pract 55:146
Altomare DF, Rinaldi M, La Torre F, et al. (2006) Red hot chili pepper and hemorrhoids: the explosion of a myth—results of a prospective, randomized, placebo-controlled, crossover trial. Dis Colon Rectum 49:1018–1023
Kumar N, Vij JC, Sarin SK, et al. (1984) Do chilies influence healing of duodenal ulcer? Br Med J (Clin Res Ed) 288:1803–1804
Siddiqi M, Kumar R, Fazili Z, et al. (1992) Increased exposure to dietary amines and nitrate in a population at high risk of oesophageal and gastric cancer in Kashmir (India). Carcinogenesis 13:1331–1335
Aucoin EJ (1987) Pruritus ani. Postgrad Med 82:76–80
Addy L, Antonarakis G (2005) Incisor toothwear caused by a dietary habit involving chilies: a case report. Dent Update 32:213–214, 216
Balachandran B, Sivaramkrishnan VM (1995) Induction of tumours by Indian dietary constituents. Indian J Cancer 32:104–109
Sielezneff I, Antoine K, Lecuyer J, et al. (1998) [Is there a correlation between dietary habits and hemorrhoidal disease?] Presse Med 27:513–517
Kang JY, Alexander B, Barker F, et al. (1992) The effect of chili ingestion on gastrointestinal mucosal proliferation and azoxymethane-induced cancer in the rat. J Gastroenterol Hepatol 7:194–198
Lysy J, Sistiery-Ittah M, Israelit Y, et al. (2003) Topical capsaicin—a novel and effective treatment for idiopathic intractable pruritus ani: a randomised, placebo controlled, crossover study. Gut 52:1323–1326
Anand P (2003) Capsaicin and menthol in the treatment of itch and pain: recently cloned receptors provide the key. Gut 52:1233–1235
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, P.J. Effect of Red Chili Consumption on Postoperative Symptoms During the Posthemorrhoidectomy Period: Randomized, Double-blind, Controlled Study. World J Surg 31, 1822–1826 (2007). https://doi.org/10.1007/s00268-007-9148-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9148-6