Abstract
Minimal access surgery in the thyroid compartment has evolved considerably over the past 10 years and now takes many forms. This study examined the feasibility and reliability of minimally invasive thyroid surgery for the management of small benign thyroid lesions. A total of 68 patients with small thyroid nodules admitted to the Oncology Center of Mansoura University, Egypt, were enrolled in this prospective randomized trial. Patients were allotted to one of two procedures: minimally invasive video-assisted thyroidectomy (MIVAT) or minimally invasive open thyroidectomy using the Sofferman technique of strap muscle transection. Exclusion criteria were nodules > 4 cm, presence of thyroiditis, and thyroid gland volume > 20 ml. Preoperative diagnosis, operating time, blood loss, postoperative pain, complications, and cosmetic outcome were all evaluated. The MIVAT group included 35 patients, and the Sofferman group included 33 patients. The main preoperative pathology was a benign follicular lesion (70.5%), and the main postoperative final pathology was follicular adenoma (54.4%). The two groups were comparable regarding age, sex, and extent of thyroid surgery. Operating time was significantly longer in the MIVAT group (115.4 ± 33.5 minutes) compared to the Sofferman group (65.6 ± 23.7 minutes). The postoperative course was significantly less painful in the MIVAT group (p < 0.05). Although patients in the MIVAT group had smaller incisions (p < 0.05), the cosmetic outcome in the two groups was comparable. No long-term complication was encountered in either group. Two distinct approaches of minimally invasive thyroidectomy are now available and can be performed safely in selected patients. Despite some MIVAT advantages of less postoperative pain and slightly better cosmesis, minimally invasive open thyroidectomy offers an advantage of less operating time with comparable cosmetic results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimal access surgery was popularized after the introduction of laparoscopic cholecystectomy by Mouret [1]. The first description of a minimally invasive approach to the thyroid gland was an endoscopic thyroidectomy performed by Gagner and Inabnet in 1996 [2]. During the following years, various minimally invasive approaches were published [3–5]. These procedures can be classified into pure endoscopic approaches [6], video-assisted endoscopic approaches [7], and minimally invasive mini-incision approaches [8]. Each of these approaches has its own advantages in terms of cosmetic results, invasiveness, tolerability, and ease of use [9].
Endoscopic approaches to the thyroid compartment remain a procedure in evolution. These approaches often require special surgical skills and a significant amount of technological assistance.
A simple but minimally invasive approach to the thyroid compartment for thyroidectomy has recently been developed. The combination of a minimal skin incision (≤6 cm) and the Sofferman technique of transecting the strap muscles (described in unpublished communications by Sofferman) allows a relatively straightforward minimally invasive thyroidectomy in selected patients [10].
Minimally invasive video-assisted thyroidectomy (MIVAT), first described by Miccoli, is one of the most popular techniques. Unlike laparoscopic techniques, this operation does not involve insufflation. Access is through a small 1.5- to 3.0-cm incision in the lower midline of the neck.
Ever since the first report of MIVAT, surgeons remain cautious about implementing this new technique, the real advantage of which even today remains controversial [11]. Many factors had limited the consideration of MIVAT as an advance, including the small subset of patients who fulfill the inclusion criteria for video-assisted thyroidectomy [12, 13] and the volume of thyroid nodules, which often exceeds the present capability of endoscopic neck surgery. The main advantage of MIVAT is improved cosmesis. Technology has also improved such that the operating time may be equal to that of conventional surgery.
Many patients have small thyroid nodules of follicular pathology on fine-needle aspiration cytology (FNAC). In 80% of cases, these nodules turn out to be benign follicular adenomas or colloid nodules [14]. Surgery in these patients is therefore undertaken for the purpose of diagnosis, and no further treatment is warranted. Although the current trend is that hemithyroidectomy is the minimum procedure for the diagnosis of thyroid nodules, it may well be that such patients are best served by a minimally invasive approach given the potential advantage of a small incision, less dissection, and reduced discomfort [15].
We report our experience with two approaches of minimally invasive thyroidectomy (Sofferman technique and MIVAT) in the management of small ( < 4 cm) thyroid nodules of follicular pathology to determine the safety and efficacy of this approach and to determine if there are any advantages associated with the use of one approach over the other.
Patients and Methods
Between March 2005 and September 2006, a prospective randomized study of 68 patients undergoing thyroidectomy was conducted at the Oncology Center, Mansoura University, Mansoura, Egypt. Patients were randomly assigned to one of two groups: minimally invasive thyroidectomy using the Sofferman technique or MIVAT. Demographic and clinical data collected included age, sex, neck ultrasonography (US), pathology, incision length, duration and extent of surgery, blood loss, and complications.
Selection Criteria
Patients in both groups had solitary thyroid nodules of < 4 cm in largest diameter in thyroid glands with a volume < 20 ml (as measured by preoperative thyroid US). There was no suspicion of malignancy on either the clinical examination or neck US. All patients had an FNAC report of a benign thyroid lesion. Other criteria included no history of thyroiditis and no previous neck surgery or irradiation.
The thyroid lesions that were removed were all subjected to frozen section histopathologic examination at surgery. All operations in both groups were performed by a single surgeon (M.H.) assisted by two of the authors.
Sofferman Technique
A minimally invasive incision (<6 cm) was used in conjunction with the Sofferman strap muscle transection technique. An approximately 4-cm incision was marked in the cervical skin crease. Once anesthesia was established, the neck was placed in mild extension using a shoulder roll. The previously marked incision was made and carried down through the platysma, exposing the strap muscles, which were transected horizontally to fully expose the thyroid gland. The superior pole vessels were isolated and ligated. The superior pole was mobilized after identifying the superior parathyroid glands. The middle thyroid vein was ligated. The inferior pole was mobilized sufficiently to identify the inferior parathyroid glands and the recurrent laryngeal nerve. The inferior pole vessels were ligated and the gland dissected free from the trachea. Hemostasis and vessels sealing was accomplished with the use of ultrasonic shears (Harmonic Ultracision Shears; Ethicon Endo-Surgery, Cincinnati, OH, USA). For unilateral lobectomy, the isthmus was divided adjacent to the contralateral lobe. For total thyroidectomy, the contralateral lobe was dissected as described. The strap muscles were approximated, the subcutaneous tissue and platysma were closed, and the skin was sutured.
Minimally Invasive Video-Assisted Thyroidectomy
Minimally invasive video-assisted thyroidectomy has been described and modified by Miccoli and his colleagues [4]. MIVAT is a three-part procedure starting with an open technique followed by the endoscopic component and then completed in an open fashion.
Open Component (Early)
The early open component of the operation is performed under general anesthesia with endotracheal intubation. The patient is situated supine with slight neck extension but without the use of a shoulder roll (a departure from conventional thyroidectomy). The primary surgeon is situated to the right of the patient. Two assistants are required, with the first assistant opposite the main surgeon and the second assistant situated at the head of the patient. The operating room nurse and the instruments are at the right of the primary surgeon. The video stack is at the head of the bed to the left of the second assistant. A 1.5- to 2.0-cm incision is made approximately 4 cm above the suprasternal notch. The skin incision is brought through the subcutaneous tissue, and the midline (linea alba) of the neck is identified and opened superiorly and inferiorly for at least 3 cm. The strap muscles are dissected off the underlying thyroid lobe on the side to be removed. During this dissection, the middle thyroid vein branches are identified and then sealed and divided with the Ultracision Harmonic Scalpel. We agree with Terris et al. [10] that whereas ultrasonic shears are desirable for conventional thyroidectomy they are indispensable for MIVAT. At this point, an Army-Navy retractor is placed laterally around the strap muscles and medially around the thyroid gland itself to retract the gland up and over the trachea. This facilitates continued open dissection of the thyroid gland. Adequate visualization for the endoscopic portion of the procedure is possible only with carefully placed retraction employing Army-Navy retractors.
Endoscopic Component
For the endoscopic component of the operation, a 30-degree laparoscopic telescope is introduced pointing initially caudally and held by the first assistant. Partial division of the sternothyroid muscle insertion into the laryngeal cartilage with the ultrasonic shears helps exposure. A pediatric right-angled clamp is helpful for isolating the superior thyroid artery and vein. These vessels are coagulated and divided by ultracision shears, working laterally to medially after preserving the external branch of the superior laryngeal nerve (Fig. 1). Once the vessels are ligated, the superior pole can be freed up and mobilized inferiorly. The superior parathyroid gland is usually readily identified at this point and dissected gently away from the thyroid gland (Fig. 2).
The 30-degree telescope is now directed caudally to allow identification of the recurrent laryngeal nerve (RLN). The inferior pole is mobilized to facilitate the identification. The inferior parathyroid gland is located and gently mobilized away from the gland. The inferior thyroid vessels are individually isolated and sealed and divided with the Harmonic Scalpel (Fig. 3). After this step is accomplished, the gland is removed using an open approach.
Open Component (Late)
For the late open component of this surgery, the mobilized superior pole is exposed, and any remaining attachments are divided, allowing the superior pole to be delivered into the wound with an artery forceps. This facilitates delivery of the remaining thyroid lobe into the wound using constant but gentle traction on the artery forceps (Fig. 4). Mobilizing and dividing the thyroid isthmus with the ultrasonic shears may help to avoid difficulty at delivery. The previous exposed RLN is traced to the cricothyroid joint. The gland now remains attached mainly by Berry’s ligament. Any small vessels close to the RLN in this situation are clipped and ligated rather than using ultracision shears close to the nerve. If the other side of the thyroid is to be removed, it is done at this point.
After removing the thyroid specimen, the isthmus is not oversewn (Fig. 5) and no drains are used (although in the early six cases we inserted a small drain that emerged through the skin incision). The strap muscles are loosely apposed (Fig. 6), and the skin is approximated with Dermabond.
Postoperative Assessment
Patients received the same protocol of postoperative analgesia: 30 mg ketorlac administered intravenously at the end of the procedure and at 8 and 16 hours postoperatively. Postoperative pain was assessed by means of a visual analog scale (VAS), where 0 cm = “no pain” and 10 cm = worst pain imaginable.” The VAS was explained to the patients during the preoperative visits. All patients were asked to evaluate their pain 6, 24, and 48 hours after the operation by indicating its level on the VAS scale.
The patients were discharged 48 hours after the operation; the longer in-hospital stay allowed us to evaluate the postoperative course more closely. Postoperative follow-up consisted of thyroid function tests, serum calcium level, and indirect laryngoscopy. The cosmetic result was evaluated by both a numeric scale and a verbal response scale. The numeric scale ranged from 0 to 10. The verbal response scale had four options: 1, poor; 2, acceptable; 3, good; 4, excellent. All patients were asked to grade the cosmetic appearance of their wounds 1 month after surgery.
Statistical Methods
Statistical analysis was performed using the t-test for age; the Mann-Whitney test for operating time and cosmetic result; Fisher’s exact test for sex, surgical procedures, preoperative diagnosis, and complications. SPSS software was used (SPSS, Chicago, IL, USA). A value of p < 0.05 was considered statistically significant.
Results
All patients undergoing thyroidectomy in the Oncology Center, Mansoura University who were deemed suitable for minimally invasive thyroidectomy, as already stated, were included in this study over an 18—month period between March 2005 and September 2006. They were randomly allocated to either of two groups: the nonendoscopic Sofferman-based minimally invasive thyroidectomy group or the MIVAT group.
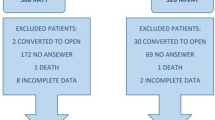
A total of 74 patients were candidates for minimally invasive thyroid surgery. At surgery, six patients required conversion to conventional thyroidectomy and were excluded, leaving 68 patients in the study (35 in the Sofferman group and 33 in the MIVAT group). Conversion was required in two patients for technical reasons: bleeding or insufficient visualization of the RLN. In one case, the gland size had been underestimated clinically and proved impossible to deliver. In the remaining three cases, the frozen section pathology examination revealed follicular carcinoma; thus, the operations were converted to open surgery, with total thyroidectomy and sentinel lymph node biopsy being carried out.
Preoperative ultrasonography had revealed 21 solid nodules, 8 mixed cystic/solid nodules, and 6 cystic nodules in patients of the Sofferman group. Among those operated on with MIVAT, 22 of the lesions were solid nodules, 9 were mixed cystic/solid nodules, and 2 were cystic. Table 1 reveals the FNAC and permanent section histopathology findings.
On frozen section examination, malignancy was identified in six cases; three of these cases were excluded from the study and converted to open surgery. In the remaining three cases, micropapillary carcinoma was diagnosed on frozen section, and total thyroidectomy was performed by minimally invasive techniques.
Nine patients underwent total thyroidectomy: five in the Sofferman group and four in the MIVAT group. This was done because of “suspicious” pathology at frozen section examination. The final pathology in these nine patients revealed micropapillary carcinoma in three cases, a hyperplastic nodule in four cases, and Hurthle cell adenoma in two cases.
As shown in Table 2, age, sex, location of the nodule, and size of the nodule did not differ in the two groups. The mean operating time for hemithyroidectomy was 65.6 minutes for the Sofferman group and 115.4 minutes for the MIVAT group, with a significant p value. For patients who underwent total thyroidectomy, the mean operating time was 102 minutes for the Sofferman group and 141.3 minutes for the MIVAT group. The difference was statistically not significant.
The mean incision length in the Sofferman group was 4.9 ± 1.1 cm compared with 2.2 ± 0.4 cm in the MIVAT group (p < 0.05). The estimated blood loss was slightly lower in the MIVAT group (39.4 ± 23.5 ml) compared with the patients in the Sofferman group (31.0 ± 12.7 ml), but the difference was statistically not significant.
Patients in the MIVAT group experienced significantly less pain than those in the Sofferman group 6, 24, and 48 hours after the operation as evaluated by the VAS (p < 0.05). Patients in the MIVAT group were slightly more satisfied with the cosmetic result as evaluated by both the verbal response and the numeric scale, but the difference was statistically not significant.
There were no cases of prolonged hypocalcemia or permanent RLN palsy in either group. Transient RLN palsy was observed in two patients, one in each group. Temporary hypoparathyroidism developed in one patient in the MIVAT group who underwent total thyroidectomy for micropapillary carcinoma. There was one hematoma in a patient in the Sofferman group that responded to conservative measures and did not require surgical evacuation (Table 3). The complication rate was insignificant between the two groups.
Discussion
Conventional thyroid surgery has stood the test of time for more than a century after being described and perfected by Theodor Kocher. Modern thyroid surgeons are beginning to embrace minimal access thyroid surgery. It is widely recognized that small incisions with minimal disruption of tissue planes promote more rapid wound healing and yield more cosmetic and functional surgical results. There are a number of ways in which minimally invasive access to the thyroid compartment can be accomplished, including minimal incisions with conventional retraction, video-assisted endoscopic thyroidectomy, and totally endoscopic thyroidectomy.
Terris et al. [10, 16] reported that minimally invasive thyroidectomy using the Sofferman technique yields excellent results. The approach involves a combination of a minimally invasive incision, transection of the strap muscles, and the routine use of ultracision shears to control the upper pole vessels. With the Sofferman technique, subplatysmal flap elevation is unnecessary; and once the strap muscles are transected, the thyroid compartment is readily accessible. This technique not only allows minimally invasive surgery it reduces the operating time. Miccoli et al. [4, 7] pioneered the MIVAT technique and reported it suitable in approximately 1 in 10 patients requiring thyroidectomy under their care. This technique uses a single 2-cm incision in the suprasternal notch, which allows a combination of direct and endoscopic views and bilateral exploration without the need for additional incisions. We present here our initial experience with minimally invasive thyroid surgery over an 18-month period with particular reference comparing MIVAT and minimal incision open thyroidectomy.
There are a number of advantages to the endoscopic approach. The most compelling benefit is the superior visualization afforded by the endoscopic magnification (up to 20×). Although difficult to measure or prove, wound healing is undoubtedly more rapid by virtue of the reduced dissection—and therefore tissue trauma—involved [17]. No subplatysmal flap is raised, and no muscles are divided with MIVAT. Edema surrounding the tissues is therefore minimal. This is reflected on a less painful postoperative course that was documented with minimally invasive techniques over conventional thyroid surgery. Moreover, a reduced incision length and avoidance of transecting the strap muscles reduced pain significantly in the MIVAT group (as determined by VAS) compared with patients in the Sofferman group (p < 0.05). These data are comparable to those of Ballantone et al. [18] and Miccoli et al. [7], who reported less postoperative pain using the endoscopic approach.
The cosmetic outcome was expressed by patients by means of both a verbal response scale and a numeric scale, and once again it was in favor of MIVAT, although the difference was statistically not significant. The cosmetic advantages are self-evident in that patients manifest a final scar that is less than an inch, which is smaller than a typical tracheostomy scar Fig. 7.
The endoscopic approach is equally safe when compared with mini-thyroidectomy. The mean blood loss was even less for the MIVAT group (31.0 ml) compared to mini-thyroidectomy (39.4 ml) with a nonsignificant p value. Miccoli et al. [7] reported complication rates for MIVAT similar to those seen with conventional thyroid surgery. They carried out the procedure successfully in 572 patients and reported definitive RLN palsy in 1.3% of patients and hypoparathyroidism in 0.2% of patients. In our series, complications were encountered in 5.7% of patients in the Sofferman group and 6.1% in the MIVAT group. One patient in the Miccoli et al. series developed hematoma requiring reexploration, as did one patient in our study. Our patient responded well to conservative measures.
The disadvantages of MIVAT include the need for additional equipment and two surgical assistants and the longer time required for surgery. The equipment used for this procedure that would not be needed for conventional thyroidectomy is a high-resolution endoscope, which is available in all modern operating rooms. Thus, no additional direct expense is incurred [16]. The ultrasonic technology (nonelectrical frictional energy) is used for most thyroidectomies performed in our center because it is known to shorten operating times by up to 30 minutes. Therefore, although we used a Harmonic Scalpel for almost all of our cases in both groups, it did not represent an incremental expense in our practice. As with most new techniques, there is a learning curve for this procedure. In their most recent publication Miccoli et al. reported that the average operating time for hemithyroidectomy fell from 73.6 minutes for their first 67 patients to an average of 47.0 minutes for this procedure [19]. In our study, the median operating time for the first 15 patients of MIVAT group was 135.0 ± 18.5 minutes and fell during the subsequent 18 cases to 105.0 ± 22.7 minutes. The median time of 115.4 minutes in this study is longer than that reported by Miccoli’s group but is comparable to that reported by Ruggieri et al. [20], and Terris et al. [16]. Moreover, although the number of patients who underwent total thyroidectomy was small (five in the Sofferman group and four in the MIVAT group), the results suggest that after an adequate learning curve MIVAT can successfully rival any open technique.
The data of this study confirm that thyroid surgery through a 2-cm lateral incision, either open or endoscopically assisted, is feasible and can be performed safely in selected patients. The other limb of this study was devised to answer the question of whether minimally invasive thyroid surgery is an appropriate operation for the diagnosis of follicular thyroid nodules.
Thyroid nodules are found in 4% to 7% of the general adult population on clinical examination and in up to 25% on ultrasound examination [21]. This incidence increases with age, and autopsy studies have revealed an incidence of thyroid nodules as high as 50% [22]. Rapidly growing, nontender nodules are likely to be malignant, as are nodules associated with cervical lymphadenopathy or RLN palsy, a history of ionizing irradiation exposure, or a family history of thyroid malignancy. The presence of any of these factors makes surgery more imperative. Most patients, however, do not have any of these factors. Patients with follicular neoplasm do, though, present a quandary. Although most thyroid FNAs reveal a follicular neoplasm, more than 80% of them are benign [23] especially if they are small. Barbaro et al. [24] suggested differentiating between low- and high-risk cytologic features of follicular neoplasms to avoid surgical intervention for benign lesions. In their review of 79 patients with follicular neoplasm diagnosed by FNAC, only 6 patients (7.6%) had carcinoma. Similarly, Mikosch et al. [25] reported that among patients in whom malignancy could not be ruled out by FNA only 10% had thyroid carcinoma. In our series of an initial 74 patients with benign follicular lesions found by FNAC, 6 of the lesions (8.1%) proved to be malignant. The tumor pathology was follicular carcinoma in three cases and micropapillary carcinoma in the other three.
Currently, fluorodeoxyglucose positron emission tomography (FDG-PET) scanning [26], proton magnetic resonance spectroscopy (MRS) [27], and immunodiagnostic techniques for FNAC (monoclonal antibodies against VD44v6 and galectin-3) [28] are modalities employed to enhance the diagnostic accuracy for follicular neoplasms. Until such modalities are proven and their use becomes widespread, no reliable way exists to differentiate benign from malignant follicular neoplasms other than by surgical excision.
At our center, hemithyroidectomy is accepted as the minimum procedure for diagnosing follicular thyroid nodules. The principal reason is the need to remove the lesion with the capsule intact, as the final diagnosis of cancer relies on careful examination of the entire capsule for vascular or capsular invasion. Another reason is that hemithyroidectomy allows safer subsequent completion thyroidectomy without the need to enter the ipsilateral operative bed [29]. In our study, this procedure could be performed safely by minimally invasive techniques. Moreover, when total thyroidectomy was indicated in nine patients in our series (five in the Sofferman group and four in the MIVAT group), the procedure was safely performed with a minimally invasive technique.
Conclusions
Minimal access thyroid surgery is feasible in the hands of well trained surgeons. Open techniques allow utilization of an incision of approximately 1.5 to 2.0 inches and requiring no specialized instruments or skills. MIVAT can be accomplished through an incision of less than an inch but requires specialized instrumentation and skills. Despite some MIVAT advantages of less postoperative pain and slightly better cosmesis, minimally invasive open thyroidectomy offers an advantage of less operating time with comparable cosmetic results. MIVAT probably has the most benefit for young female patients with little or no skin creases who have a small follicular lesion with benign histology. It offers potential advantages of better cosmesis and less postoperative distress.
References
Mouret P (1996) How I developed laparoscopic cholecystectomy. Ann Acad Med Singapore 25:744–747
Gagner M, Inabnet MB (2000) Minimally invasive thyroid surgery. In: Gagner M, Inabnet WB, (editors), Minimally Invasive Endocrine Surgery Workshop, New York, Mount Sinai Hospital, pp 1–10
Husscher CSG, Napolitano C, Chiodini S, et al. (1997) Video assisted thyroidectomy. Eur J Coelio 3:57
Miccoli P, Berti P, Conte M, et al. (2000) Minimally invasive video-assisted surgery of the thyroid: a preliminary report. Langenbecks Arch Surg 385:262–264
Ishii S, Ohgami M, Arisawa Y, et al. (1998) Endoscopic thyroidectomy with anterior chest wall approach. Surg Endosc 12:611
Takami H, Ikeda Y (2002) Endoscopic thyroidectomy via an axillary or anterior chest approach. In: Gagner M, Inabnet WB, (editors). Minimally Invasive Endocrine Surgery, 1st edition. Philadelphia, Lippincott Williams & Wilkins, pp 56–63
Miccoli P, Berti P, Raffaelli M, et al. (2000) Comparison between minimally invasive video assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 130:1039–1043
Ferzli G, sayad P, Abdo Z, et al. (2001) Minimally invasive non-endoscopic thyroid surgery. J Am Coll Surg 192:665–668
Takami H, Ikeda Y (2006) Minimally invasive thyroidectomy. Curr Opin Oncol 18:43–47
Terris DJ, Bonnett A, Gourin CG, et al. (2005) Minimally invasive thyroidectomy using the Sofferman technique. Laryngoscope 115:1104–1108
Lo Gerfo P (1998) Invited commentary. Surg Endosc 3:206
Ikeda Y, Tamaki H, Sasaki Y, et al. (2002) Comparative study of thyroidectomies: endoscopic surgery vs. open surgery. Surg Endosc 16:1741–1745
Ohgami M, Ishii S, Ohmori T, et al. (2000) Scarless endoscopic thyroidectomy: breast approach better cosmesis. Surg Laparosc Endosc Percut Tech 10:1–4
Reeve TS, Delbridge L, Sloan D, et al. (1986) The impact of fine needle aspiration biopsy on surgery for single thyroid nodules. Med J Aust 145:308–311
Sackett WR, Barraclough BH, Sidhu S, et al. (2002) Minimal access thyroid surgery: is it feasible, is it appropriate? ANZ J Surg 72:777–780
Terris DJ, Gourin CG, Chin EM (2006) Minimally invasive thyroidectomy: basic and advanced techniques. Laryngoscope 116:350–356
Terris DJ, Chin E (2006) Clinical implementation of endoscopic thyroidectomy in selected patients. Laryngoscope 116:1745–1748
Ballantone R, Lombardi CP, Bossola M, et al. (2002) Video-assisted vs conventional thyroid lobectomy: a randomized trial. Arch Surg 137:301–304
Miccoli P, Berti P, Materazzi G, et al. (2004) Minimally invasive video- assisted thyroidectomy: five years of experience. J Am Coll Surg 199:243–248
Ruggieri M, Straniero A, Mascaro M, et al. (2005) The minimally invasive open video- assisted approach in surgical thyroid diseases. BMC Surg 27:9
Burguera B, Gharib H (2000) Thyroid incidentalomas: prevalence, diagnosis, significance, and management. Endocrinol Metab 14:559–575
Mortensen IC, Woolner LB, Bennett WA (1955) Gross and microscopic findings in clinically normal thyroid glands. J Clin Endocrinol Metab 15:1270–1280
Zdon MJ, Fredeland AJ, Zaret PH (2001) Follicular neoplasms of the thyroid: predictors of malignancy? Am Surg 67:880–884
Barbaro D, Simi U, Lopan P, et al. (2001) Thyroid nodules with microfollicular findings reported on fine needle aspiration: invariably surgical treatment? Endocr Pract 7:352–357
Mikosch P, Wartner U, Keresnik E, et al. (2001) Results of preoperative ultrasound guided fine needle aspiration biopsy of solitary thyroid nodules as compared with histology: a retrospective analysis of 538 patients [abstract]. Nuklearmedizin 40:148–154
Cohen MS, Arslan N, Dehdashi F, et al. (2001) Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose- positron emission tomography. Surg 130: 941–946
Mackinnon WB, Delbridge L, Russel P, et al. (1996) Two dimensional proton magnetic resonance spectroscopy for tissue characterization of thyroid neoplasms. World J Surg 20:841–847
Barolazzi A, Gasbarri A, Papotti M, et al. (2001) Application of an immunodiagnostic method for improving preoperative diagnosis of nodular thyroid lesions. Lancet 537:1644–1650
Reeve TS, Delbridge L, Cohen A (1987) Total thyroidectomy: the preferred option for multinodular goiter. Ann Surg 206:782
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hegazy, M.A.F., Khater, A.A., Setit, A.E. et al. Minimally Invasive Video-Assisted Thyroidectomy for Small Follicular Thyroid Nodules. World J Surg 31, 1743–1750 (2007). https://doi.org/10.1007/s00268-007-9147-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9147-7