Abstract
Background
The reasons for anastomotic leakage in esophago-gastrostomy have been proposed to be poor arterial inflow and insufficient venous drainage at the anastomotic site. In order to improve the congestive status, we developed a novel and easy surgical procedure of transient bloodletting from the short gastric vein after making a gastric tube during esophagectomy, and evaluated tissue blood flow.
Methods
Patients with esophageal cancer, who had received transthoracic esophagectomy and gastric tube reconstruction with intrathoracic anastomosis, were enrolled. After making a slender gastric tube, transient bloodletting from the short gastric vein at the most cardiac site was performed for 30 minutes. The tissue blood flow of the proximal end of the gastric tube was measured using a laser Doppler flowmeter, and was compared in the bloodletting group (n = 68) and the control group without bloodletting (n = 8).
Results
In the bloodletting group, tissue blood flow 5 minutes after the start of bloodletting was markedly increased in comparison to that before bloodletting (9.5 ± 4.9 ml/min/100 g vs. 24.1 ± 5.9 ml/min/100 g). The elevated levels of tissue blood flow remained at almost constant levels after ceasing bloodletting and lasted until esophago-gastrostomy (20.1 ± 3.9 ml/min/100 g). On the contrary, in the control group without bloodletting, tissue blood flows were marginally increased following construction of a gastric tube, but the changes did not reach significant levels. When the tissue blood flow just before esophago-gastrostomy was compared in the bloodletting and control groups, the flows in the bloodletting group were significantly more elevated than those in the control group (20.1 ± 3.9 vs. 15.2 ± 4.9 ml/min/100 g).
Conclusions
Transient bloodletting of the short gastric vein in the gastric tube during esophagectomy may improve the microcirculation of the oral side of the gastric tube.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although control of esophageal cancer at the advanced stage remains difficult, several aggressive treatment modalities including surgical resection with extensive lymphadenectomy, such as 3-field lymph node dissection1,2 and/or chemo-radiotherapy,3,4 have been proposed. During esophagectomy, a gastric tube made by whole or subtotal stomach is commonly used as the reconstructed organ. However, there is a relatively high incidence (3%–24%) of anastomotic leakage with esophago-gastrostomy, which causes stricture formation after spontaneous healing or may lead to fatal septic complications such as pyothorax.5,6 It is important to reduce the incidence of this anastomotic leakage for esophageal surgery. The reasons for anastomotic leakage in esophago-gastrostomy have been proposed to be poor arterial inflow and insufficient venous drainage at the anastomotic site of the gastric tube, mechanical tension with esophago-gastrostomy, technical problems in the suturing of the anastomosis and poor nutritional status.5–7 In order to reduce anastomotic leakage technically, several surgical options have been proposed including the use of a slender gastric tube8, the supercharge technique, which involves additional vascular anastomosis of the gastric tube by microsurgical techniques,9,10 and the use of auto-suturing techniques using a stapler device.11 In particular, the efficacy of the supercharge technique has been reported, although this technique is complicated.9,10 We developed a novel and easy surgical procedure of transient bloodletting from the short gastric vein after making a gastric tube during esophagectomy, resulting in improvement of the microcirculation on the oral side of the gastric tube.
Recently, laser Doppler flowmetry has been developed to measure tissue blood supply quantitatively and evaluate blood flow at the anastomotic site during esophagectomy.8,12,13
In the present study, we performed transient bloodletting of the short gastric vein in the gastric tube during esophagectomy, measured tissue blood flow at the anatomic site of the gastric tube by laser Doppler flowmetry before and after bloodletting, and compared the flow in the treated group and the control group without bloodletting.
MATERIALS AND METHODS
Patients
From August 2001 to June 2005, 68 patients with esophageal cancer (bloodletting group) and 8 patients with esophageal cancer (control group without transient bloodletting), who had received transthoracic esophagectomy and gastric tube reconstruction with intrathoracic anastomosis at the First Department of Surgery, University of Yamanashi Hospital, were enrolled in the present study. Patient characteristics are shown in Table 1 and the stage was defined according to the UICC-TNM classification of esophageal cancer. None of the patients received radiotherapy, chemotherapy, or other medical interventions before surgery. This study was approved by the ethical committee of the University of Yamanashi, and written informed consent was obtained from all individuals.
Operative Procedures
All procedures including esophagectomy and reconstruction were performed by the same surgeon (K.K.) and same procedures except for bloodletting were performed in both the bloodletting group and the control group. Depending on the extent of lymph node metastasis, tumor invasion and also tumor location, 2-field (mediastinal and abdominal lymphadenectomy) or 3-field lymph node dissection (cervical, mediastinal, and abdominal lymphadenectomy) was performed. The operation was started with an abdominal procedure including gastric mobilization and finished with intrathoracic anastomosis in the right chest in the 2-field lymph node dissection group. Also, in the 3-field lymph node dissection group, the operation was started with the abdominal procedure and cervical lymphadenectomy at the same time by the different surgeons, and finished with intrathoracic anastomosis in the right chest.
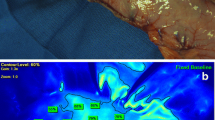
To prepare the slender gastric tube at the upper median laparotomy, the lesser curvature side of the stomach was divided along 4 cm from the greater curvature by a Linear Cutter (Ethicon, Somerville, NJ, USA) with the remaining 3 branches of the right gastric vessels, the greater omentum was resected at 3 cm distal to the side from the right gastroepiploic vessel, and all of the short gastric vessels were resected at the greater curvature (Fig. 1). The left gastric vessel was ligated at the orifice and the lymph nodes along the upper part of the abdominal aorta and along the celiac trunk were dissected.
In the abdomen before gastric pull-up, transient bloodletting from the short gastric vein at the most cardiac site of the slender gastric tube was performed for 30 minutes along with measuring of tissue blood flow (Fig. 1); then the short gastric vein was ligated.
Transthoracic esophagectomy was performed through a thoracotomy at the right fourth intercostal space. Before intrathoracic anastomosis (esophago-gastrostomy), measuring of tissue blood flow was performed again in the thoracic cavity. Intrathoracic anastomosis was performed by the auto-stapling technique using an ILS25 circular stapler (Ethicon), followed by the Lembert suture.
Clinical Follow-up
The anastomosis was tested for leakage by X-ray films with water-soluble contrast medium on the seventh post-operative day, and anastomotic leakage was defined as extravasation of water-soluble contrast medium.
Postoperative pneumonia was diagnosed by chest X-ray films and cardiac complications, such as arrhythmia or ischemic change, were defined as the need for treatment with drugs. Stricture in the esophago-gastrostomy was defined as the need for therapeutic dilation. Hospital mortality was defined as death during hospitalization for the esophageal operation.
Measurement of Tissue Blood Flow of The Gastric Tube
Tissue blood flow of the proximal end of the gastric tube was measured using an Advance laser flowmeter (Model ALF-21; Advance, Tokyo, Japan) with master probe Type S (Advance) at 4 time points: before bloodletting from the short gastric vein, 5 minutes after the start of bloodletting, 15 minutes after ceasing bloodletting, and just before esophago-gastrostomy (Fig. 2A). The master probe with a specific weight ring was positioned until the values become constant. Each measurement was repeated three times and the mean value of these was expressed as tissue blood flow (ml/min/100 g).
In the control group without bloodletting, tissue blood flow of the proximal end of the gastric tube was measured at three time points: just after making the gastric tube, 30 minutes after making the gastric tube, and just before esophago-gastrostomy (Fig. 2B).
Statistics
Differences between blood flow values were determined using the Student’s paired t test and a differences were considered significant at P < 0.05.
RESULTS
Tissue Blood Flow at the Anastomotic Site of the Gastric Tube
Tissue blood flow at the anastomotic site of the gastric tube was measured using a laser Doppler flowmeter. In the bloodletting group (n = 68, Fig. 2A), tissue blood flow 5 minutes after the start of bloodletting was markedly increased in comparison to that before bloodletting (9.5 ± 4.9 vs. 24.1 ± 5.9 ml/min/100 g, P < 0.01). The elevated levels of tissue blood flow remained at almost constant levels after ceasing bloodletting (21.1 ± 4.1 ml/min/100 g), although they did marginally decrease (P = 0.19). Furthermore, the elevated levels of tissue blood flow lasted until esophago-gastrostomy (20.1 ± 3.9 ml/min/100 g).
On the contrary, in the control group without bloodletting, tissue blood flow was gradually increased following construction of a gastric tube, but the changes did not reach significant levels (Fig. 2B). When the tissue blood flow just before esophago-gastrostomy was compared in the bloodletting and control groups, the flow in the bloodletting group was significantly elevated above that of the control group (20.1 ± 3.9 vs.15.2 ± 4.9 ml/min/100 g, P < 0.05). These observations indicated that transient bloodletting resulted in the improvement of tissue blood flow at the anastomotic site of the gastric tube.
Clinical Course
The clinical course is summarized in (Table 2). Of the 68 patients in the bloodletting group, 1 patient (1.4%) had a minor leakage of the esophago-gastrostomy, which was cured by conservative therapy within 2 weeks. During the transient bloodletting, patients suffered from extra bleeding of 76 ± 24 ml. One patient in the bloodletting group received re-operation due to the postoperative bleeding.
DISCUSSION
The current report provides the finding that the novel surgical procedure of transient bloodletting of the short gastric vein in the gastric tube during esophagectomy may improve the microcirculation of the oral side of the gastric tube.
The reasons for anastomotic leakage of esophago-gastrostomy during esophagectomy have been proposed to be poor arterial inflow and insufficient venous drainage on the anastomotic site of the gastric tube, mechanical tension with esophago-gastrostomy, technical problems in the suturing of the anastomosis, and poor nutritional status.5–7 Ikeda et al. reported that patients with tissue blood flow of less than 10 ml/min/100 g tissue blood flow, measured by laser flowmeter at the anastomotic site, had anastomotic leakage, indicating that blood flow at the anastomotic site may be a dominant predictive factor for leakage.12 Also, it is likely that the congestive state of the anatomic site in the gastric tube is one of the major factors in anastomotic leakage with esophago-gastrostomy. Murakami et al. reported that the additional supercharging anastomosis of arteries and veins of the gastric tube induced a significant increase in blood flow at the anastomotic site.14 This procedure may lead to complete resolution of the congestive state of the gastric tube. It has been reported that with the advance of microsurgical techniques, microvascular anastomosis should become more reliable. At present, the patency rates of microvascular anastomosis have increased to as high as 95%.15 However, Sekido et al. reported that the use of the supercharge technique required an additional operating time of more than 1 hour.9
In order to improve the congestive state, we performed transient bloodletting of the short gastric vein at the most oral site of the gastric tube as a novel surgical procedure. As a result, we showed that bloodletting could improve the blood flow of the anastomotic site of the gastric tube, as evaluated by laser Doppler flowmetry, in comparison to that in the control group without bloodletting. Moreover, even if bloodletting was transient and terminated after 30 minutes, the elevated blood flow lasted. Although it remains unclear why transient bloodletting could induce elevated blood flow after ceasing bloodletting, it could be speculated that the transient bloodletting could enhance additional communication between blood vessels, thereafter, leading to the improved microcirculation of the gastric tube.
With regard to the blood flow of the gastric tube during esophagectomy, Tabira et al. reported that the width of gastric tubes has no impact on tissue blood flow at the anastomotic site, as well as the frequency of leakage, in a randomized prospective study.8 Matsuzaki et al. and others reported that systemic infusion of prostaglandin E1 (PGE1) increased tissue blood flow in a reconstructed gastric tube.16,17 Furthermore, it has been shown that thoracic epidural anesthesia significantly improves the microvascular perfusion of the distal part of the gastric tube.18 Here, we provide a new finding that transient bloodletting of the short gastric vein in the gastric tube during esophagectomy could improve the microcirculation of the oral site of the gastric tube.
During the transient bloodletting, patients suffered from extra-bleeding of 76 ± 24 ml. We considered that this extra-bleeding due to bloodletting is acceptable in the total bleeding of the esophagectomy (629 ± 220 ml).
Since the present study was not a randomized control study, there are too many weaknesses to draw any definite conclusion from the present study. Currently, we are initiating a randomized control study to enable us to draw conclusions on the significance of transient blood letting in the gastric tube during esophagectomy.
In summary, transient bloodletting of the short gastric vein in the gastric tube during esophagectomy may improve the microcirculation of the oral site of the gastric tube. Transient bloodletting in the reconstructed gastric tube is an easy, less invasive, and efficient procedure during esophagectomy.
References
Akiyama H, Tsurumaru M, Udagawa H, et al. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 1994;220:364–372.
Tachibana M, Kinugasa S, Yoshimura H, et al. Extended esophagectomy with 3-field lymph node dissection for esophageal cancer. Arch Surg 2003;138:1383–1389.
Fiorica F, Di Bona D, Schepis F, et al. Preoperative chemoradiotherapy for oesophageal cancer: a systematic review and meta-analysis. Gut. 2004;53:925–930.
Urba SG, Orringer MB, Turrisi A, et al. Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 2001;19:305–313.
Urschel JD. Esophagogastrostomy anastomotic leaks complicating esophagectomy: a review. Am J Surg 1995;169:634–640.
Walther B, Johansson J, Johnsson F, et al. Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg 2003;238:803–812.
Dewar L, Gelfand G, Finley RJ, et al. Factors affecting cervical anastomotic leak and stricture formation following esophagogastrectomy and gastric tube interposition. Am J Surg 1992;163:484–489.
Tabira Y, Sakaguchi T, Kuhara H, et al. The width of a gastric tube has no impact on outcome after esophagectomy. Am J Surg 2004;187:417–421.
Sekido M, Yamamoto Y, Minakawa H, et al. Use of the “supercharge” technique in esophageal and pharyngeal reconstruction to augment microvascular blood flow. Surgery 2003;134:420–424.
Nagawa H, Seto Y, Nakatsuka T, et al. Microvascular anastomosis for additional blood flow in reconstruction after intrathoracic esophageal carcinoma surgery. Am J Surg 1997;173:131–133.
Santos RS, Raftopoulos Y, Singh D, et al. Utility of total mechanical stapled cervical esophagogastric anastomosis after esophagectomy: a comparison to conventional anastomotic techniques. Surgery 2004;136:917–925.
Ikeda Y, Niimi M, Kan S, et al. Clinical significance of tissue blood flow during esophagectomy by laser Doppler flowmetry. J Thorac Cardiovasc Surg 2001;122:1101–1106.
Pierie JP, De Graaf PW, Poen H, et al. Impaired healing of cervical oesophagogastrostomies can be predicted by estimation of gastric serosal blood perfusion by laser Doppler flowmetry. Eur J Surg 1994;160:599–603.
Murakami M, Sugiyama A, Ikegami T, et al. Additional microvascular anastomosis in reconstruction after total esophagectomy for cervical esophageal carcinoma. Am J Surg 1999;178:263–266.
Harii K. The free flap in head and neck reconstruction. In: Fee WE, editor, Head and neck cancer. Philadelphia: Decker, 1990, pp 33–35.
Matsuzaki Y, Edagawa M, Maeda M, et al. Beneficial effect of prostaglandin E1 on blood flow to the gastric tube after esophagectomy. Ann Thorac Surg 1999;67:908–910.
Miyazaki T, Kuwano H, Kato H, et al. Predictive value of blood flow in the gastric tube in anastomotic insufficiency after thoracic esophagectomy. World J Surg 2002;26:1319–1323.
Lazar G, Kaszaki J, Abraham S, et al. Thoracic epidural anesthesia improves the gastric microcirculation during experimental gastric tube formation. Surgery 2003;134:799–805.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kono, K., Sugai, H., Omata, H. et al. Transient Bloodletting of the Short Gastric Vein in the Reconstructed Gastric Tube Improves Gastric Microcirculation During Esophagectomy. World J. Surg. 31, 780–784 (2007). https://doi.org/10.1007/s00268-006-0285-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-006-0285-0