Abstract
It has been suggested that gastric cancer has a worse prognosis in young patients, but the data are controversial. The aim of this study was to compare the 5-year survivals after gastrectomy for gastric cancer in two groups of patients (those ≤45 years of age and those (>45 years) and to determine some of the prognostic factors. The 5-year survival was significantly better for patients ≤45 years of age. Survival was also better for young patients with a curative resection and also for those with lymph node metastases. However, survival was not significantly different for the two groups when the resection was not curative and when the lymph nodes were not involved. Survival was no different for the two groups when compared at each stage, although a multivariate analysis showed that age >45 years, moderate or poor degree of differentiation of the tumor, advanced tumors, the presence of lymph node involvement, and a noncurative resection were independent negative prognostic factors. Long-term survival after gastrectomy for gastric cancer depends on the stage of the disease; the age of the patient is not a decisive factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer is the second most frequent cause of death due to malignancy worldwide. It occurs mainly in older patients, with a peak incidence over 60 years of age.1 The frequency of gastric carcinoma in the young is relatively low and the prognosis in young patients after gastrectomy has been a controversial subject. Some authors have suggested that young patients have a worse prognosis, mainly due to delayed diagnosis and more aggressive tumor behavior, whereas others have shown that age is not an independent factor for survival.2 The aim of this study was to compare the survival of patients younger and older than 45 years of age operated on for a gastric carcinoma and to determine the prognostic factors affecting these patients.
MATERIAL AND METHODS
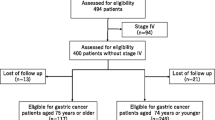
From 1985 to 2002, a total of 442 patients with gastric carcinoma underwent gastric resection in our department. All of the patients were studied and treated according to a prospective protocol. Preoperative studies included routine laboratory analysis, endoscopy and biopsy, chest radiography, and abdominal ultrasonography or computed tomography (CT). The age and gender of the patient; the type of operation performed; the site, size, gross type, and histologic type of the tumor; and the depth of tumor invasion in the gastric wall were analyzed. The number and level of lymph node metastases were determined according the rules of Japanese Research for the Study of Gastric Cancer, and the patients were staged according the TNM system from the 1997 American Joint Committee on Cancer (AJCC).3
Total gastrectomy was performed in patients with tumors located in the upper third and the upper middle third of the stomach, and a subtotal gastrectomy was done in those with tumors in the inferior and low middle third of the stomach. Radical gastrectomy included omentectomy, D2 lymphadenectomy, and splenectomy (during total gastrectomy). D2 lymphadenectomy included the perigastric nodes, the celiac group, and the hepatic artery nodes (groups 1–9). During total gastrectomy the nodes of the splenic hilum and those of the splenic artery were also resected (groups 10 and 11). Curative resection (R0) was recorded if macroscopically and microscopically no tumor was left after surgery. The criteria used to determine a curative or a noncurative resection were the absence of tumor invasion in the surgical margins and in the last lymph node resected barrier, (according to the rules of Japanese Research for the study of Gastric Cancer), and if there was no or minimal serosal invasion.
Patients were divided into two groups: group A, patients ≤45 years old; group B, patients >45 years old. The age limits for the two groups was determined using Receiver Operating Characteristic (ROC) curves. There were no significant differences between the two groups in terms of the depth of tumor invasion, the presence of lymph node metastases, the curative resection rate, the degree of differentiation of the tumor, or the stage of the disease. Total gastrectomy was performed in 40 patients of group A (68.9%) and in 230 patients of group B (59.9%). The cumulative long-term survival was calculated with the Kaplan-Meier method using the disease-specific mortality figures. A multivariate analysis for prognostic factors was done for the age of the patients, the degree of differentiation of the tumor, the depth of tumor invasion in the gastric wall (early or advanced cancer), and the presence of lymph nodes metastases.
Statistical analysis was performed with the log-rank, Cox, and χ2 tests. A value of P < 0.05 was considered statistically significant.
The median follow-up for the whole series was 49 months. The median follow-up of the survivors was 92 months.
RESULTS
Among the 442 patients there were 282 men and 160 women, with a male/female ratio of 1.8:1.0. The mean age of the patients was 62 ± 13 years. Group A (≤ 45 years) included 58 patients (13%), and group B (>45 years) included 384 patients (87%). The mean ages were 39.1 ± 5.2 years for group A and 65.5 ± 9.5 years for group B. The stage distribution of the patients was not significantly different between the two groups (Table 1). There was no postoperative mortality in group A, whereas in group B the mortality rate was 3.6% (14 patients). Postoperative morbidity was not significantly different between the two groups: Postoperative complications were observed in 11 patients (18.9%) in group A and in 59 patients (15.4%) in group B.
The overall 5-year survival rate was 44.3%. The 5-year survival of group A patients was significantly better (63.8%) than that of group B (41.4%) (P = 0.0016). The patients in group A with a curative resection had also a significantly better 5-year survival (78%) than those of group B with a curative resection (59%) (P = 0.01). However, patients with a noncurative resection did not show any difference in survival when the groups were compared: Group A had a 5-year survival of 29.4% and group B 15.8% (P = 0.33).
The overall 5-year survival of the patients was significantly different depending on the stage of the tumor. Survival of those with stage IA was 91.5%, IB 72.5%, II 60.9%, IIIA 32.7%, IIIB 19.5%, and IV 12.7% (P = 0.001). However, there was no significant difference in survival when patients from group A were compared with patients of group B at each stage. Lymph node metastases were found in 290 (66%) of the 440 patients. In group A 35 patients (60%) had lymphatic metastases, whereas in group B 225 (66%) had lymph node involvement (not significant, or NS). When studied relative to the presence of lymphatic metastases, patients without metastases had a significantly better 5-year survival (73.6%) than did patients with metastases (27.6%) (P = 0.0001). When a comparison was done among patients of both groups relative to the presence of lymph node metastases, a significant difference in survival was shown in patients with metastases (group A 45.7% vs. group B 25.1%; P = 0.0078). For patients without lymphatic metastases, the better survival observed in group A (91.3%) versus group B (73.6%) was not significantly different (P = 0.06).
Only 34 of the 442 patients (7.7%) had a well differentiated adenocarcinoma in the histologic study. Moderately differentiated adenocarcinomas were observed in 102 (23%) and poorly or undifferentiated carcinomas in 306 (69.3%) patients. There was no significant difference in the distribution of patients according to the degree of differentiation of the tumors in the two groups, although the poorly and undifferentiated tumors numbered 49 (84.5%) in the younger patients and 257 (66.9%) in the others (NS).
The multivariate analysis showed that the following factors were independent negative prognostic factors for the 5-year survival: age >45 years, moderate or poor degree of differentiation of the tumor, advanced tumors (those with tumor invasion of the gastric wall to the proper muscular layer or deeper), the presence of lymph node metastases, and a noncurative resection.
DISCUSSION
Gastric carcinoma is usually diagnosed in elderly people. The mean age of the patients in this study, as in a previous report from our department, is 62 years.4 It is interesting to observe that although the mean age of our patients is similar to the age reported in the literature,1,5 the proportion (13%) of young patients (≤45 years) is one of the highest reported. The proportion of young patients with gastric cancer, in general, varies from 2% to 8%. Only a few articles have reported a higher proportion of young patients than we report here. Theuer et al. 6 reported that 15% and Medina-Franco et al. 7 reported that 16.2% of the patients were <40 years of age in their respective series. On the other hand, Kitamura et al., 8 showed that there was a trend toward a decline of gastric cancer in young patients during the last 20 years. Most authors have shown a tendency toward a decrease in the male/female ratio among younger patients compared to that of older patients; it is mainly due to an increasing frequency of gastric cancer in young women.7,9 However, the male/female ratio in this study was similar in the two groups.
The prognosis and survival records of young patients after gastrectomy for gastric carcinoma have produced controversial data. Some authors have found that young patients have a worse prognosis mainly due to the different features of the gastric cancers in younger and older patients and a frequent delay in the diagnosis.9–11 It is known that younger patients show a tendency to have a larger proportion of diffuse and undifferentiated tumors and that linitis plastica appears more frequently than in older patients.1,12,13 Other studies have suggested that the delay in the diagnosis is a negative prognostic factor in young patients and that they also have more aggressive disease.7,14,15 The possible influence of morbidity factors associated with the aging process on the long-term results might have been less in our series because we used disease-specific figures for the mortality rates. In the present series, the frequency of moderately and poorly differentiated tumors was not significantly different in the two groups, but moderate and poor degrees of differentiation of the tumor were found to be a significant independent negative prognostic factor in the multivariate analysis. Although the frequency of early gastric cancer was relatively, but not significantly, higher in young patients, the rate of curative resection (and thus long-term survival) were significantly higher in this group.
Survival of the group of younger patients in this series was better than that for the older group. However, when the comparison was done by each stage, survivals were not different for the two groups. This result confirms that the prognosis after surgery depends mainly on the stage of the disease rather than age. Lai et al., 16 also showed that the survival of patients younger than 35 years, despite the more aggressive features of the tumor (higher frequency of diffuse and scirrhous types), depended on the stage of the disease, not on the age of the patients. Others have not found differences in the clinicopathologic characteristics of gastric carcinoma regarding the outcome after treatment among young and elderly patients.2,7
There were no cases of familial or hereditary gastric cancer in this series, as has been reported for other groups of young patients.15,17 Kokkola and Sipponen [2] reported that 11.5% of the patients <41 years old with gastric cancer had a familial component. Ramos-De la Medina et al., 18 showed that 16.9% of their patients <40 years of age had a family history of gastric cancer, but in their experience it had no impact on the prognosis.
Although the diffuse or undifferentiated type of gastric cancer tends to occur relatively more frequently in young patients,6,12,16 in these series the rate of poorly differentiated or undifferentiated tumors in young patients (84.5%) was not significantly different from that in the older patients (66.9%). In the multivariate analysis, however, the moderate or poor degree of differentiation was a negative prognostic factor.
Our results show that patients ≤45 years of age had a better overall survival and that age >45 years was an independent negative prognostic factor. They suggest, however, that the long-term results depend on the stage of the disease and that age is not a decisive factor.
References
Hohenberger P, Gretschel S. Gastric cancer. Lancet 2003;362:305–315
Kokkola A, Sipponen P. Gastric carcinoma in young adults. Hepatogastroenterology 2001;48:1552–1555
American Cancer Society. American Joint Committee on Cancer. AJCC Cancer Staging Manual,. 5th edition, Philadelphia, Lippincott-Raven, 1997
Llanos O, Guzmán S, Pimentel F, et al. Results of surgical treatment of gastric cancer. Dig Surg 1999;16:385–388
Fuchs CS, Mayer RJ. Gastric carcinoma. N Engl J Med 1995;333:32–41
Theuer CP, de Virgilio C, Keese G, et al. Gastric adenocarcinoma in patients 40 years of age or younger. Am J Surg 1996;172:473–476
Medina-Franco H, Heslin Mj, Cortes-Gonzalez R. Clinicopathological characteristics of gastric carcinoma in young and elderly patients: a comparative study. Ann Surg Oncol 2000;7:515–519
Kitamura K, Yamaguchi T, Yamamoto K, et al. Clinicopathological analysis of gastric cancer in young adults. Hepatogastroenterology 1996;43:1273–1280
Matley PJ, Dent DM, Madden MV, et al. Gastric carcinoma in young adults. Ann Surg 1988;208:593–596
Tso PL, Bringaze WL, Dauterive AH. Gastric carcinoma in the young. Cancer 1987;59:1362–1365
Wanebo HJ, Kennedy BJ, Chmiel J, et al. Cancer of the stomach: a patient care study by the American College of Surgeons. Ann Surg 1993;218:583–592
Eguchi T, Takahashi Y, Yamagata M, et al. Gastric cancer in young patients. J Am Coll Surg 1999;188:22–26
Duarte I, Ohmke J, Ciani S, et al. Patterns of carcinoma in gastrectomy specimens from Chilean adults; a multivariate analysis in a high-risk area. Gastr Latinoam 2001;12:12–18
Quijano F, Moreno E, Alvarez JJ, et al. Gastric carcinoma in patients under 35 years. Rev Gastroenterol Mex 1999;64:75–77
Koea JB, Karpeh MS, Brennan MF. Gastric cancer in young patients: demographic, clinicopathological and prognostic factors in 92 patients. Ann Surg Oncol 2000;7:346–351
Lai IR, Lee WJ, Chen CN, et al. Gastric cancer in the young. Hepatogastroenterology 1997;44:1641–1645
Maehara Y, Emi Y, Tomisaki S, et al. Age-related characteristics of gastric carcinoma in young and elderly patients. Cancer 1996;77:1774–1780
Ramos-De la Medina A, Salgado-Nesme N, Torres-Villalobos G, et al. Clinicopathologic characteristics of gastric cancer in a young patient population. J Gastrointest Surg 2004;8:240–244
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Llanos, O., Butte, J.M., Crovari, F. et al. Survival of Young Patients after Gastrectomy for Gastric Cancer. World J. Surg. 30, 17–20 (2006). https://doi.org/10.1007/s00268-005-7935-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-7935-5