Abstract
Background
The main goal of the Essential Trauma Care (EsTC) project is to promote affordable and sustainable improvements in trauma care, on the ground in individual countries and their health care facilities. This has been occurring in several countries, including Ghana.
Results
The EsTC project has helped to solidify previously haphazard interactions between stakeholders from different sectors. It has allowed trauma care clinicians to interact more effectively with other groups, such as the Ministry of Health and the WHO country office. It has allowed the clinicians and other stakeholders to more effectively lobby government for increased attention to trauma care services. These interactions have led to a high-profile stakeholders meeting, the Road Safety and Essential Trauma Care Workshop, which has represented the highest level of attention to trauma care in the country thus far. This meeting has generated a set of policy recommendations, which has been presented to Parliament for study, and, it is hoped, adoption.
Conclusions
To convert these recommendations to solid, sustainable action in improving care for the injured, we need to continue to engage in advocacy and to work with Parliament, the Ministry of Health, and other stakeholders, as well as to confront the deeper problems of Ghana’s brain drain, civil strife, and poverty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Injury has become a leading health problem in Ghana. The toll of death and disability is increasing daily, especially from road traffic crashes. Only in the past few years has there been the beginning of an organized response to this tragedy. Included in this response are increased attention and efforts toward road safety. Such increased attention has only very lately been applied to trauma care.
Although it is a major contributor to patient volume and costs in Ghana’s health care system, there has been no organized government program to strengthen trauma care in Ghana. This is quite unlike the very notable improvements from organized efforts to confront other health problems including vaccine-preventable diseases, malaria, tuberculosis, maternal child health, and HIV/AIDS. In this article, we outline developments in trauma care in Ghana over the past decade and indicate how the Essential Trauma Care Project has helped to catalyze and accelerate these developments.
PRIOR EFFORTS AND FRUSTRATIONS
Ever since her independence in 1957, Ghana has had many notable, well-qualified professionals caring for the injured. This includes doctors, nurses, and other professionals, many of whom have worked against considerable frustrations and odds to create the best possible care at individual institutions. However, up until the 1990s, there had been very little in the way of unified calls for system-wide improvements. This changed in 1997 when several surgeons who were active in the care of the injured, drafted a proposal to the government entitled, “Recommendations on Strengthening the Trauma System in Ghana.” This 20-page document addressed prehospital care, as well as care at the spectrum of facilities in Ghana from small, primary health clinics (PHC) up to tertiary care teaching hospitals. The recommendations looked primarily at how improvements could be made within Ghana without the need to depending on or waiting for external funding. All recommendations were low cost and eminently achievable and sustainable. There was an initial glimmer of hope as persons in the Ministry of Health had requested such a plan. However, after development of these recommendations, and after re-presenting them to representatives of five successive ministries of health serving under three regimes, the document had basically gathered dust over a 9-year period.
Our frustration was characterized by the fact that our ministers in various government ministries had their own agendas, which they had to fight for in order to hold to power. What was more, they did not see the immediate results of trauma care improvements coming early enough to be to their advantage during electioneering. Compounding the situation was the fact that trauma care was a non-issue on both the public agenda and the agenda of international donor agencies.
During this time, several pieces of research were carried out that highlighted the ongoing tragedy of trauma deaths in Ghana. The resulting reports showed that the death rate could have been lowered by various low-cost improvements. These studies included one that looked at the facilities for trauma care in hospitals located on the major roadways of Ghana. These were all district hospitals staffed primarily by general practitioners. However, by virtue of their location on these main roads, they all received high volumes of injured patients, primarily from road traffic crashes. At all 11 hospitals surveyed, low-cost equipment for care of the injured was frighteningly absent. For example, none of the 11 hospitals had chest tubes, a low-cost item that is vitally important for the care of life-threatening chest injuries. Only 4 of the 11 hospitals had airway equipment. Even in those 4, the airway equipment was locked in the operating rooms and not promptly available in the casualty wards.1
Another study looked at the patterns of death among trauma patients in Ghana, demonstrating that 80% of all trauma deaths occurred in the field, before the patients had any chance of receiving hospital-based care. This study highlighted the importance of addressing the prehospital setting in efforts to lower the overall trauma mortality in Ghana.2
One additional study looked at the process of trauma care at one of the major teaching hospitals in Ghana. This facility was considerably better equipped than the district hospitals mentioned above. Nevertheless, there were considerable deficiencies in care. For example, there was very low utilization of chest tubes, even thought they were physically available. There were prolonged delays in emergency surgery, with a mean of 13 hours between presentation and start of emergency operations. There was also low utilization of blood and fluid resuscitation for patients in shock. The study concluded with a call for establishment of basic medical audit programs (quality assurance) as a way to address deficiencies in process of care in a comprehensive fashion.3 These studies, which were highly publicized within Ghana, helped to stimulate increased attention to trauma care, along with the international developments mentioned below.
RECENT IMPROVEMENTS
Several local and international developments have helped to promote greater understanding of the importance of trauma care among government ministers and politicians. Locally, there has been a growing cry of outrage from the public at the increasing toll of death on Ghana’s roadways. Everyday in the newspapers, tragic crashes such as those involving multiple deaths in buses are highlighted. In 2003, the Ghana Medical Association hosted a public meeting to publicize this problem. This 2-day conference was titled “The Carnage on Our Roads,” and was widely covered in the press.
Internationally, in 2004, World Health Day was dedicated to the topic of road safety. This day was used to launch the World Health Organization (WHO) publication World Report on Road Traffic Injury Prevention.4 Interestingly, in the same year, Ghana’s Minister of Health was Chairperson for the Executive Committee of the World Health Assembly (the governing board for the WHO). His role in helping to promote World Health Day and the related WHO publication helped to increase the prominence of this topic both internationally and locally in Ghana. That publication was primarily devoted to road safety, but it included a component on strengthening trauma care services, including a mention of the forthcoming Guidelines for Essential Trauma Care.5 Two months later (June 2004) WHO released that publication as well. This national and international attention greatly assisted promotion of the issue of strengthening trauma care in Ghana.
The Guidelines for Essential Trauma Care calls for creation of national trauma plans and provides a template or framework to do that. It is envisioned in this publication that various stakeholders in trauma care from different backgrounds would work collaboratively to implement the recommendations of the Guidelines. With this goal in mind, various stakeholders in Ghana came together to work on the Road Safety and Essential Trauma Care meeting.
AKOSOMBO WORKSHOP: ROAD SAFETY AND ESSENTIAL TRAUMA CARE
With the active input of clinicians caring for trauma patients in Ghana. A working group was established involving several lead agencies, among them the Ghana chapter of the Global Road Safety Partnership (GRSP). This international non-government organization is headquartered in Geneva and works closely with the International Federation of Red Cross and Red Crescent Societies. It has local chapters in many developing countries. The Ghana chapter of the GRSP obtained a small amount of funding to conduct this meeting. Its principal partner is the National Road Safety Commission (NRSC), an agency of the Ghana government. These two groups, working collaboratively, drew up a plan for the Akosombo workshop. Early on, they sought the endorsement and involvement of the WHO country office.
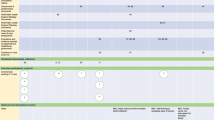
The plan for this meeting was to adapt the Guidelines for Essential Trauma Care to Ghana’s circumstances, as well as to develop an implementation plan and set of policy recommendations. The meeting was attended by a multi-sectoral group, including those involved with clinical care, transport, emergency response, disease surveillance, and other aspects of road safety and trauma care, as indicated in Table 1. Most participants agreed that this was the highest level attention to trauma care that had ever been achieved in Ghana. Three working groups were established: Injury Surveillance, Prehospital Care, and Facility-based Care.
Injury Surveillance
Any effort to improve trauma care must be based on solid fact and must be monitored with such solid fact to assure that these efforts are having the desired consequences of lowering injury death rates. If not, such efforts need to be modified to be successful. Hence, there is a need for accurate and timely information on injury-related deaths. Hence, any improvements in trauma care are closely linked to developing accurate injury surveillance systems. The working group developed plans for strengthening Ghana’s existing injury surveillance systems.
Prehospital Care
Given the aforementioned fact that 80% of injury deaths in Ghana occur in the prehospital setting, any improvements in trauma care must address this topic. Represented in this working group were members of Ghana’s newly established National Ambulance Service. Also represented were members of the formal first response system, primarily the Fire Service, as well as groups that worked with lay-first responders such as the Ghana Red Cross.
Facility-based Care
Represented in the working group on facility-based care were clinicians who provide care for injured persons at Ghana’s network of hospitals and other health care facilities. It was notable that the representatives of all four levels of health care in Ghana were represented. This included PHC, which are primarily non-doctor-staffed rural clinics. Capabilities for trauma care at these clinics are miniscule. Nonetheless, because they are the only health care facilities for wide, rural areas, many injured patients do receive care at a PHC. Input for this level of care was provided by a representative from Ghana’s Nurse and Midwife Council. A second group was made up of doctors who care for injured persons at district hospitals (small, primarily general practioner-staffed hospitals), regional hospitals (at which there is usually at least one surgeon), and teaching hospitals (the two tertiary care facilities in Ghana).
The meeting was also attended by five members of Ghana’s Parliament, including representatives of the Committee on Health and the Committee on Transport. It was also attended by members of the ruling party as well as the main opposition party, who worked together closely during the meeting.
RESULTS OF THE MEETING
Participants drew up a set of policy recommendations addressing the spectrum of trauma care in the country, as indicated in Table 2. This is titled “Strengthening Care for Injury Victims: Recommendations for a National Policy.” These recommendations adapt the resource matrices from the Guidelines for Essential Trauma Care to the Ghanaian context. They also address methods for implementation of these resource matrices, as well as for improvements in injury surveillance and prehospital trauma care. Since the meeting, these recommendations have been provided to the two main committees of Ghana’s parliament that have expressed an interest, the Committee on Health and the Committee on Transport. These recommendations are based on the premise that improvements in care and resultant decreases in injury-related death and disability can be achieved at low cost and in a sustainable fashion, primarily through improved organization and planning.
The meeting has also contributed to publicity and advocacy for trauma. A communiqué from the meeting was printed in Ghana’s newspapers, and features appeared on television and radio, as well as in print media.
A key player in developing health policy in all African nations is the WHO. Every African country has a WHO country office, which works closely with the Ministry of Health. Prior to the Akosombo meeting, the WHO country office in Ghana had never had any involvement with trauma care. After the meeting, the WHO country office has now integrated elements of trauma care planning into its pivotal 2-year plan of collaboration with the Ghana Ministry of Health. This is a very significant development in trauma-related health policy in our country.
Obviously, continued efforts are needed to convert the preliminary policy recommendations into real action. However, the above events are very promising and notable for a country whose Ministry of Health was barely considering trauma as a health problem until a few years ago.
Challenges
We must continue the processes that started at the Akosombo meeting. In so doing, we must be aware of major challenges to progress and that are difficult to change.
Brain Drain
As in many African nations and other developing countries, Ghana has lost many of its health care professionals to the higher-paying industrialized world. Ghana’s two medical schools graduate 200 new doctors each year. Yet, the number of doctors in the country has remained at around 2000 for each of the past 10 years. Loss of nurses is even more problematic, as many are being actively recruited by agencies from developed countries. Even within the country, there is a silent migration of qualified doctors and nurses from rural facilities to urban areas. Efforts at promoting Essential Trauma Care will be meaningless unless we can assure an adequate health care work force. Thus, efforts to promote Essential Trauma Care need to link with efforts to stem the brain drain.
Wars and Civil Strife
Parts of northern Ghana have seen repeated ethnic conflict. Health care personnel have left the conflict areas for fear of their lives. In addition huge sums of state resources are directed toward peace keeping, thus hindering provision of social services such as health care.
Poverty
Many of the services in Ghana’s health care system need to be paid for at the time of use, sometimes prior to use. This has represented a considerable barrier to trauma care, especially for the poor. In an effort to make health care more affordable, the government has implemented the nationwide Health Insurance Scheme. Although the annual contribution to this can be as low as US$6–$7, even this amount is unavailable to many families who exist on the daily minimum wage of $0.50 and especially rural families that do not even earn the minimum wage. This individual poverty is compounded by the actions of the World Bank and the International Monetary Fund, which have imposed tight financial restrictions on Ghana’s economy, including limitations on the amount that may be spent on health care.
CONCLUSIONS
The Essential Trauma Care Project has helped to catalyze improvements in trauma care in Ghana. It has provided trauma care clinicians with a tool for advocacy in approaching officials in our Ministry of Health. It has served as a foundation to build on in partnering with other stakeholders in trauma care, including the WHO country office. These interactions led to a high-profile stakeholders meeting, titled Road Safety and Essential Trauma Care, which represented the highest level attention to trauma care in the country thus far. This meeting generated a set of policy recommendations that were presented to Parliament for study and, it is hoped, adoption. To convert these recommendations to solid, sustainable action in improving care for the injured, we need to continue to engage in advocacy and work with Parliament, the Ministry of Health, the WHO country office, and other stakeholders, as well as to confront the deeper problems of Ghana’s brain drain and poverty.
References
Quansah R. Availability of emergency medical services along major highways. Ghana Med J 2001;35:8–10
Mock CN, Jurkovich GJ, nii-Amon-Kotei D, et al. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma 1998;44:804–814
London JA, Mock CN, Quansah RE, et al. Priorities for improving hospital based trauma care in an African city. J Trauma 2001;51:747–753
Peden M, Scurfield R, Sleet D, et al. World Report on Road Traffic Injury Prevention. Geneva, World Health Organization, 2004
Mock C, Lormand JD, Goosen J, et al. Guidelines for Essential Trauma Care. Geneva, World Health Organization, 2004
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the 41st World Congress of Surgery, Durban, South Africa, 22 August, 2005.
Rights and permissions
About this article
Cite this article
Quansah, R. Essential Trauma Care in Ghana: Adaptation and Implementation on the Political Tough Road. World J. Surg. 30, 934–939 (2006). https://doi.org/10.1007/s00268-005-0766-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0766-6