Abstract
Introduction
The aim of this study was to compare the outcomes between the LigaSure vessel sealing system and the conventional closed Ferguson hemorrhoidectomy procedure performed by diathermy.
Methods
A series of 84 patients with grades III and IV hemorrhoids were randomized into two groups: (1) LigaSure hemorrhoidectomy with submucosal dissection (42 patients) and (2) Ferguson hemorrhoidectomy (42 patients). The patient demographics, operative details, parenteral analgesic requirement, postoperative pain score (assessed by an independent assessor), operating time, intraoperative blood loss, hospital stay, early and delayed complications, and time off from work or normal activity were recorded. The patients were regularly followed up at 1, 2, 4, 6, and 8 weeks after surgery.
Results
There were no statistically significant differences between the two groups in terms of age, gender, duration of symptoms, grade of the hemorrhoid(s), or number of hemorrhoids resected. The mean operating time for LigaSure hemorrhoidectomy with submucosal dissection was significantly shorter than that for the Ferguson hemorrhoidectomy (11.3 ± 0.4 vs. 34.2 ± 0.7 minutes; P < 0.0001). Patients treated with the LigaSure method had significantly less blood loss (P < 0.0001), a better pain score (P < 0.0001), less parenteral analgesic requirement (P < 0.0001), shorter hospital stay (P < 0.0001), and less time off from work or normal activity (P < 0.0001). There was no difference in the early and delayed postoperative complications between the two groups.
Conclusions
LigaSure hemorrhoidectomy with submucosal dissection is a safe, effective procedure for grade III and IV hemorrhoids. Patients derive greater short-term benefits: reduced intraoperative blood loss, operating time, and postoperative pain as well as earlier resumption of work or normal activity. Long-term follow-up with a larger number of patients is required to confirm the long-term results of this procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hemorrhoids constitute one of the most common problems in surgical practice. Hemorrhoidectomy remains the most definitive procedure to treat symptomatic grades III and IV hemorrhoids.1 Although hemorrhoidectomy is superior to any proposed conservative procedure, including rubber band ligation, sclerotherapy, photocoagulation, and cryotherapy,1 it is usually associated with significant postoperative complications, including pain, bleeding, and anal stricture.2 Conventional standard methods include the Milligan-Morgan open hemorrhoidectomy3 and the Ferguson closed hemorrhoidectomy.4
Recent advances in instruments that include an bipolar electrothermal device,5 ultrasonic scalpel,6 and circular stapler7 have provided effective alternatives, resulting in less postoperative pain and perioperative blood loss. The LigaSure vessel sealing system (Valleylab, Boulder, CO, USA) is a novel, hemostatic device designed primarily for use in abdominal surgery. Using a combination of pressure and electrical energy, it ensures complete coagulation of vessels up to 7 mm in diameter with minimal surrounding thermal spread and limited tissue charring. Theoretically, the LigaSure system is an ideal instrument for hemorrhoidectomy, as it enables effective, bloodless excision of hemorrhoids with minimal tissue trauma.
The limited tissue injury may also reduce wound sepsis, facilitate wound healing, and decrease postoperative pain. Several randomized trials have been performed to compare LigaSure hemorrhoidectomy with conventional hemorrhoidectomy,5,8–12 and the results suggest that LigaSure hemorrhoidectomy is a safe, simple method to improve surgical results.
In the present randomized study, we used LigaSure hemorrhoidectomy with submucosal dissection to ensure that the underlying sphincters remained intact and there was complete removal of hemorrhoid bundles. The operative outcomes of the LigaSure method and the Ferguson closed hemorrhoidectomy were compared to determine their efficacy and safety.
PATIENTS AND METHODS
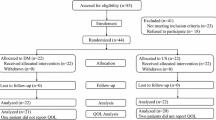
This prospective study included 84 consecutive patients with symptomatic grade III or IV hemorrhoids operated on at the Department of Surgery, Kaohsiung Medical University Hospital between November 2004 and April 2005. Written informed consent was obtained from all of the subjects or guardians after full explanation of the procedure. The exclusion criteria included patients on anticoagulants and those with a hematologic disorder, concomitant anal disease, or a history of anorectal surgery. The recruited patients were randomly allocated to undergo either a LigaSure hemorrhoidectomy with submucosal dissection (42 patients) or a conventional Ferguson hemorrhoidectomy (42 patients).
The operative procedures for hemorrhoidectomy were standardized in each case by the same team of surgeons. Randomization was performed at the time of anesthesia by selecting sealed envelopes.
The operation was performed under general or epidural anesthesia at the discretion of the anesthetist. The patients were placed in the prone jackknife position and a Ferguson retractor was used to expose the hemorrhoids. LigaSure hemorrhoidectomy with submucosal dissection was performed initially with a skin incision at the junction of the hemorrhoid and the flat perianal skin by a scalpel, followed by dissection of the hemorrhoid bundles off the underlying sphincter. A LigaSure handset was applied to the dissected hemorrhoids up to the pedicles, taking care to avoid incorporating the underlying sphincters. The device was activated to seal the mucosal edges. The feedback-controlled sensor signaled the completion of coagulation, and the coagulated tissue was excised along the line of the coagulum. The LigaSure was repeatedly applied as necessary for complete excision of the hemorrhoids.
Conventional Ferguson hemorrhoidectomy was performed by submucosal dissection of the hemorrhoidal tissue from the underlying sphincter using standard monopolar diathermy. The vascular pedicle was ligated with nonabsorbable suture, and the mucosal edges were opposed with a continuous chromic catgut suture. Hemostasis was ensured in both the LigaSure and Ferguson groups, and a hemostatic sponge was inserted in the anal canal.
For postoperative pain relief, oral acetaminophen (500 mg) was prescribed for all of the patients at a dose of one tablet four times a day. Additional parenteral analgesics were administrated when patients complained of intolerable pain. The independent assessor evaluated the pain score by means of the visual analog score (0–10) 24 hours postoperatively. The patient demographics, duration of symptoms, operative details, operating time, intraoperative blood loss, and hospital stay were documented. Follow-up was performed at 1, 2, 4, 6, and 8 weeks in all 84 patients to detect postoperative complications and time away from work or normal activity.
Pain reduction of 50% and operating time reduced by more than 30% were clinically relevant, so these limits were chosen as parameters by which to calculate the study power.8 The initial power calculation suggested that a minimum of 68 patients would be required to achieve statistical significance with a power of 80% at the 5% significance level. All of the data were analyzed using the Statistical Package for the Social Sciences Version 10.0 software (SPSS, Chicago, IL, USA). Results were expressed as the mean ± standard error. The two-sided Pearson’s χ2 test and Student’s t-test were used to compare the variables between the two groups. A value of P < 0.05 was considered statistically significant.
RESULTS
The characteristics of 84 symptomatic patients with grade III or IV hemorrhoids are summarized in Table 1. There were 20 men and 22 women treated by LigaSure hemorrhoidectomy, and 21 men and 21 women treated by Ferguson hemorrhoidectomy (P = 0.827). The mean age was 47.1 ± 2.4 and 47.5 ± 2.3 years for the LigaSure and Ferguson hemorrhoidectomies, respectively (P = 0.926). There was no statistical difference in the duration of symptoms (P = 0.585) or the severity of the hemorrhoids (P = 0.776) between the two groups.
Table 2 shows the operative details and outcomes for the two groups. The mean operating time was 11.3 ± 0.4 minutes and 34.2 ± 0.7 minutes for the LigaSure and Ferguson methods, respectively (P < 0.0001). The mean intraoperative blood loss was considerably less with the LigaSure hemorrhoidectomy than the Ferguson hemorrhoidectomy (0.6 ± 0.2 vs. 25.7 ± 1.3 ml, P < 0.0001). Favorable operative results, such as a lower pain score, less parenteral analgesic requirement, and shorter hospital stay, were all observed for the LigaSure method (all P < 0.0001).
As regards early postoperative complications, three (7.1%), two (4.8%), and one (2.4%) patient developed constipation, urine retention, and hemorrhage, respectively, after LigaSure hemorrhoidectomy, whereas five (11.9%), five (11.9%), and one (2.4%) patient developed the corresponding complications after Ferguson hemorrhoidectomy (all P > 0.05). The incidence of postoperative hemorrhage was similar in the two groups (2.4%), with two patients with underlying diabetic nephropathy undergoing hemodialysis during their admission. Fortunately, none of these patients required surgical intervention.
The incidence of delayed postoperative complications, such as poor wound healing, anal stenosis, or flatus incontinence, did not show any significant difference between the two groups (all P > 0.05). Complete wound healing was achieved in the patients at 6 weeks in both groups. The three patients with anal stenosis improved significantly after anal dilation at the outpatient department. Finally, the return to work or normal activity was significantly earlier after LigaSure hemorrhoidectomy (8.8 ± 0.2 days) than after Ferguson hemorrhoidectomy (13.7 ± 0.4 days) (P < 0.0001).
DISCUSSION
Hemorrhoidectomy is the most effective and definitive treatment for prolapsed hemorrhoids. Nevertheless, excessive tissue trauma can result in considerable postoperative pain. The resulting pain-related complications after conventional hemorrhoidectomy are often the major factors that account for prolonged hospital stays and delayed recovery. Various techniques and modifications have been developed with the aim of overcoming postoperative pain, including modification procedures such as diathermy excision without ligation,13 the introduction of various surgical instruments,5–7 the use of preoperative lactulose14 and metronidazole,15 and the addition of lateral internal sphincterotomy.16 None, however, seems to influence postoperative pain.
The LigaSure vessel sealing system delivers optimal electrocautery energy across the diathermy jaws, which ensures complete coagulation with minimal thermal spread and limited tissue charring, which is in contrast to that produced when using the existing electrocautery instruments. Theoretically, its application in hemorrhoidectomy may reduce anal spasm and pain.
Similar to several recent reports on the LigaSure method,5,8–12 the present study shows that LigaSure hemorrhoidectomy with submucosal dissection is a fast, safe, effective surgical modality for complete removal of the hemorrhoid cushions with a limited complication rate. The LigaSure method of dissection significantly reduces postoperative pain and the parenteral analgesic requirement, possibly because of the reduction of lateral thermal injury and the absence of sutures. Consequently, the LigaSure system facilitates earlier hospital discharge and return to normal work or activity.
Consistent with previous randomized clinical studies,5,8–12 the LigaSure hemorrhoidectomy with submucosal dissection offers technical advantages over conventional hemorrhoidectomy by reducing the operating time and intraoperative blood loss. The mean operating time is about 11 minutes, and the mean blood loss is less than 2 ml for each LigaSure hemorrhoidectomy, which may be explained by its effective hemostatic control. An area of concern for hemorrhoidectomy is the potential for inadvertent anal sphincter injury. However, with the concomitant use of submucosal dissection in the present study, the hemorrhoidal plexuses can be readily elevated off the underlying anal sphincter, allowing safe application of the diathermy forceps and less residual hemorrhoidal tissue.
The early and delayed complication rates of the LigaSure method are comparable to those for conventional hemorrhoidectomy, and no serious complications were noted. After conservative management, all of the patients recovered uneventfully without subsequent surgical intervention. Stapled hemorrhoidectomy is a less painful procedure than LigaSure hemorrhoidectomy, but the latter is a more radical operation,17 with serious complications including pelvic sepsis, anastomotic stenosis, fecal incontinence, and rectovaginal fistula.18 Using LigaSure hemorrhoidectomy with submucosal dissection, concomitant external hemorrhoid components and skin tags can be addressed, and complete removal of the hemorrhoid tissues can be ensured while keeping the underlying sphincter intact.
CONCLUSIONS
LigaSure hemorrhoidectomy with submucosal dissection can provide a safe, fast, bloodless, low-morbidity surgical alternative to various surgical modalities for hemorrhoids. However, long-term follow-up with a larger series is warranted.
References
MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities: a meta-analysis. Dis Colon Rectum 1995;38:687–694
Ho YH, Seow-Choen F, Tan M, et al. Randomized controlled trial of open and closed haemorrhoidectomy. Br J Surg 1997;84:1729–1730
Milligan ET, Morgan CN, Jones LE, et al. Surgical anatomy of the anal canal, and the operative treatment of haemorrhoids. Lancet 1937;2:119–124
Ferguson JA, Heaton JR. Closed hemorrhoidectomy. Dis Colon Rectum 1959;2:176–179
Sayfan J, Becker A, Koltun L. Sutureless closed hemorrhoidectomy: a new technique. Ann Surg 2001;234:21–24
Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled trial. Lancet 2000;355:779–781
Armstrong DN, Ambroze WL, Schertzer ME, et al. Harmonic Scalpel vs. electrocautery hemorrhoidectomy: a prospective evaluation. Dis Colon Rectum 2001;44:558–564
Palazzo FF, Francis DL, Clifton MA. Randomized clinical trial of LigasureTM versus open haemorrhoidectomy. Br J Surg 2002;89:154–157
Jayne DG, Botterill I, Ambrose NS, et al. Randomized clinical trial of LigasureTM versus conventional diathermy for day-case haemorrhoidectomy. Br J Surg 2002;89:428–432
Thorbeck CV, Montes MF. Haemorrhoidectomy: randomised controlled clinical trial of Ligasure® compared with Milligan-Morgan operation. Eur J Surg 2002;168:482–484
Chung YC, Wu HJ. Clinical experience of sutureless closed hemorrhoidectomy. with LigasureTM. Dis Colon Rectum 2003;46:87–92
Franklin EJ, Seetharam S, Lowney J, et al. Randomized clinical trial of LigasureTM vs. conventional diathermy in hemorrhoidectomy. Dis Colon Rectum 2003;46:1380–1383
Andrews BT, Layer GT, Jackson BT, et al. Randomized trial comparing diathermy hemorrhoidectomy with the scissor dissection Milligan-Morgan operation. Dis Colon Rectum 1993;36:580–583
London NJ, Bramley PD, Windle R. Effect of four days of preoperative lactulose on posthaemorrhoidectomy pain: results of placebo controlled trial. BMJ 1987;295:363–364
Carapeti EA, Kamm MA, McDonald PJ, et al. Double-blind randomised controlled trial of effect of metronidazole on pain after day-case haemorrhoidectomy. Lancet 1998;351:169–172
Galizia G, Lieto E, Castellano P, et al. Lateral internal sphincterotomy together with haemorrhoidectomy for treatment of haemorrhoids: a randomised prospective study. Eur J Surg 2000;166:223–228
Basdanis G, Papadopoulos VN, Michalopoulos A, et al. Randomized clinical trial of stapled hemorrhoidectomy vs open with Ligasure for prolapsed piles. Surg Endosc 2005;19:235–239
Oughriss M, Yver R, Faucheron JL. Complications of stapled hemorrhoidectomy: a French multicentric study. Gastroenterol Clin Biol 2005;29:429–433
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, JY., Lu, CY., Tsai, HL. et al. Randomized Controlled Trial of LigaSure with Submucosal Dissection versus Ferguson Hemorrhoidectomy for Prolapsed Hemorrhoids. World J. Surg. 30, 462–466 (2006). https://doi.org/10.1007/s00268-005-0297-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0297-1