Abstract
Ultrasound is one of the preferred modalities for localization of abnormal parathyroids. Accuracy of ultrasound is technician-dependent. This study was undertaken to determine the accuracy of surgeon-performed ultrasound (SPU) for the localization of parathyroid tumors in comparison to radiology-performed ultrasound (RPU) and nuclear scintigraphy (NS). In this series 74 consecutive patients with untreated primary hyperparathyroidism underwent SPU at the initial clinic visit; 21 of these patients did not undergo surgery and are excluded from the analysis. Of the 53 patients remaining, RPU was obtained in 26, and 52 patients underwent NS. Directed parathyroidectomy was performed with use of the intraoperative parathyroid hormone assay (IOPTH). In all, 46 patients had a single adenoma as indicated by IOPTH and final pathology. Two patients had double gland disease, and 5 patients had multi-gland hyperplasia. The sensitivity of SPU was 82% and the specificity was 90% in detecting the diseased glands on the correct side (right versus left). The sensitivity for RPU was 42% and the specificity was 92% (n = 26). The sensitivity of NS was 44% and the specificity was 98% (n = 52). In only one case did RPU or NS detect a gland not found by SPU. SPU can be done with accuracy comparable to other ultrasound series in the literature, and it may be superior to RPU or NS in some institutions. It is important for surgeons to be aware of local institutional expertise when relying on RPU and NS during preoperative evaluation prior to directed parathyroidectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Directed parathyroidectomy has become a widely accepted approach to the treatment of primary hyperparathyroidism [1]. A major limitation to the success of directed parathyroidectomy is the imperfection of preoperative localization techniques [2]. Standard techniques to localize abnormal parathyroids preoperatively include ultrasound and nuclear scintigraphy.
The sensitivity of ultrasound for parathyroid localization varies widely in the literature. It has been reported from 38% to 98% [3, 4, 5, 6, 7, 8]. This has led some investigators to suggest that there is no role for routine use of ultrasound in patients undergoing initial exploration for primary hyperparathyroidism [4, 9]; others suggest that all patients should undergo ultrasound prior to initial exploration [10, 11]. Undoubtedly operator skill, experience, and interest play a role in determining the accuracy of ultrasound. Many centers expert in endocrine disease have experienced radiologists who have particular interest in these diseases. Many of these same centers are responsible for reports in the literature documenting the accuracy of ultrasound and nuclear scintigraphy for parathyroid localization. Clearly, the results of these highly specialized centers might not translate to general radiology departments.
As a means to bridge this gap we chose to study the accuracy of clinician-performed ultrasound. Our rationale was that if interested clinicians could perform this examination accurately, centers without expert and interested radiologists could more successfully perform directed parathyroidectomy. Secondary benefits would include improved patient convenience and better appreciation of anatomic localization by the operating surgeon. We hypothesized that an interested clinician could perform ultrasound for parathyroid localization with an accuracy equal to traditional radiology departments. This study was designed to compare the accuracy of surgeon-performed ultrasound (SPU) to the literature, and to our local experience with radiology-performed ultrasound (RPU) and nuclear scintigraphy (NS) in the localization of parathyroid abnormalities.
Materials and Methods
From June 2001 to September 2003, 74 consecutive patients were evaluated for untreated primary hyperparathyroidism. Previously operated patients and those with secondary hyperparathyroidism were excluded from the study. Twenty-one patients who did not undergo surgery were also eliminated from the study. The decision against surgery in these patients was not based on imaging studies; diagnosis was confirmed on the basis of elevated serum I-PTH levels, elevated total and/or ionized serum calcium levels, and normal to elevated urinary calcium excretion. During the study period, the senior author (L.K.) transferred to a different institution, so patients from two different Veterans Affairs hospitals and a university hospital were included in the study, as were three different radiology departments. Data were collated and analyzed retrospectively.
All patients were examined with SPU upon initial visit. In most cases this was the initial study performed, although some patients had imaging studies completed prior to referral. The ultrasound exam was performed with the patient lying supine with the neck slightly hyperextended. All SPU scans were performed by the same surgeon using a 7.5 MHz linear array probe to examine the anterior neck. Ultrasound units from various manufacturers were used including Aloka (Tokyo, Japan), GE (Waukesha, WI), and B-K (Copenhagen, Denmark). Multiple images of the structures of the anterior neck were obtained in both the transverse and longitudinal planes. A hypoechoic mass in the appropriate anatomic location posterior or inferior to the thyroid lobe was considered to be representative of a parathyroid adenoma. Presence or absence of a visualized lesion; size of abnormal lesions in transverse, anteroposterior (A/P), and longitudinal dimensions; and other visualized abnormalities were recorded.
Radiology-performed ultrasound (RPU) was accomplished with high-resolution ultrasonography in the radiology department. No special instructions were given to the radiologist other than a request to localize abnormal parathyroids. All of these studies were performed by ultrasound technologists, and static images were sent to the radiologists for interpretation. Although the clinic ultrasound findings were available in the medical record, in most (if not all) cases the technologists and radiologists were unaware of the ultrasound results from the clinic.
Radionuclide localization was performed according to the routine in the various nuclear medicine departments. Single tracer dual phase scintigraphy was used at all institutions. Patients received an intravenous injection of either 925 Mbq or 614 Mbq of Tc-99m-sestamibi. The neck and upper portion of the thorax were imaged at 30 minutes and 3 hours in those that received 925 Mbq and at 30 minutes, 90 minutes, and 3 hours in those that received 614 Mbq. The nuclear medicine staff and radiologists were unaware of this study.
Surgery was performed on all patients by the same surgeon (L.K.). Directed parathyroidectomy was attempted in the standard surgical fashion on 49 of the 51 patients. Two patients underwent thyroid lobectomy for concurrent thyroid disease. Adequacy of parathyroid excision was based on results of an intraoperative parathyroid hormone assay (IOPTH) using previously published criteria [12, 13]. The procedure was converted to a bilateral neck exploration if there was no evidence of an abnormal gland upon directed exploration or if IOPTH level failed to decrease appropriately after excision of suspected pathological gland(s).
Results
The study included 53 patients, 31 men and 22 women. The mean preoperative total serum calcium level was 10.8 mg/dl with a range of 8.8–13 mg/dl (normal range: 8.3–10.3 mg/dl). The mean preoperative intact parathyroid hormone (IPTH) level was 152 pg/ml with a range of 32–311 pg/ml (normal range: 12–72 pg/ml). Postoperative mean calcium levels fell to 9.4 mg/dl, with a range of 8.6– 10.1 mg/dl. IPTH levels fell to a mean of 53 pg/ml, with a range of 18.4–100 pg/ml. Operative and pathologic findings revealed 46 patients with single gland adenomas, one patient with a double adenoma, one patient with a concurrent parathyroid cyst and parathyroid adenoma, and 5 cases of multigland hyperplasia. The mean weight of the excised glands was 704 mg (range: 87–3,000 mg) (Table 1).
All 53 patients underwent preoperative SPU. At least one suspected parathyroid was identified in 47 of 53 (89%) cases. 55 abnormal-appearing glands were identified in 47 patients. In the 3 patients with multiple glands identified preoperatively, one had an adenoma and a concurrent parathyroid cyst and two had only single adenomas on exploration. No abnormal glands were identified in six patients. Of the six patients with no identifiable abnormal glands by ultrasound, four had four gland hyperplasia and two had a single adenoma. Of these adenomas, one was an ectopic gland found in the carotid sheath lateral to the carotid artery and posterior to the clavicular head. This gland was only identified by nuclear scintigraphy and was counted as a true positive for that study and false negatives for all other studies. Mean follow-up for this study was 8.3 months. There were no cases of persistent or recurrent hypercalcemia.
The average gland weight was 704 mg (range: 87–3000 mg). The average gland weight for false-negative examinations by SPU was 553 mg (range: 120–2300 mg). The average gland weight for true-positive examinations by SPU was 723 mg (range: 87–3000 mg). Gland size was assigned by multiplying greatest A/P × transverse × longitudinal diameter. This is obviously not a true volume but rather an index of size. The average gland size identified on SPU was 1282 mm3 [Standard deviation (SD) = 2009], and the average gland size at pathology was 1642 mm3 (SD = 2268). The correlation coefficient between sonographic size and pathology-measured size was 0.9294 (p < 0.0001, confidence interval 0.8556- 0.9662) (Fig. 1).
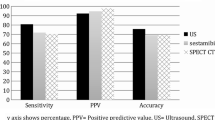
Two sets of calculations were performed for the sensitivity and specificity of each test. The first set addressed the ability of the tests (SPU, RPU, NS) to identify the appropriate side (right versus left) of the diseased gland as confirmed by surgery and pathology. The second set addressed the ability of the tests to identify the correct anatomic position—right inferior versus right superior versus left inferior versus left superior—of the diseased gland as confirmed by surgery and pathology.
The sensitivity of SPU was 82% and the specificity was 90% in detecting the diseased glands on the correct side (right versus left). The positive predictive value was 90% and the negative predictive value was 82%. The sensitivity of SPU was 66% and the specificity was 93% in detecting the gland in the appropriate anatomic location (right inferior versus right superior versus left inferior versus left superior) (Table 2). In most cases where the preoperatively identified gland location did not correlate with the surgically identified gland location, the glands were correctly identified but incorrectly assigned as inferior or superior. The tight correlation between sonographic size and pathologic size (above) further confirms correct identification of the pathologic lesion.
A total of 26 patients underwent RPU. The same-side sensitivity for RPU was 42% and the specificity was 92% (Table 2). Because of its low sensitivity, RPU was abandoned after the initial 26 patients; RPU did not identify any glands that were not identified by SPU.
Nuclear scintigraphy was performed on 52 patients. One patient with concurrent thyroid cancer and a parathyroid adenoma easily identified on SPU did not undergo nuclear scintigraphy. The sensitivity of the parathyroid scan was 44% and the specificity was 98% (Table 2).
In most cases (32 out of 53), SPU preceded other imaging modalities, but in some cases an imaging study preceded referral to the surgeon. In the cases where a radiology study preceded SPU, the surgeon-performed study correctly identified the gland found at operation in 86% of the cases. In those cases where the SPU was performed first, 74% of the examinations correctly identified the gland found at operation. These results were not found to be statistically significantly different (p = 0.33).
Fourteen patients were noted to have concurrent thyroid disease either by ultrasound or at the time of operation. The sensitivity of SPU to identify disease on the correct side (right versus left) in the presence of thyroid disease was 80%, and the specificity was 92%. The sensitivity of SPU to detect disease on the correct side in the absence of thyroid disease was 83%, and the specificity was 89%. The sensitivity of SPU to detect disease in the appropriate anatomic location in the presence of thyroid disease was 61%, and the specificity was 95%. The sensitivity of SPU to detect disease in the appropriate anatomic location in the absence of thyroid disease was 67%, and the specificity was 93% (Table 3). There was no statistical difference with regard to the sensitivity of SPU with concurrent thyroid disease versus the sensitivity in the absence of thyroid disease (p = 0.6).
Discussion
Ultrasound machines (Fig. 2) are being widely marketed to surgeons and other clinicians. While relatively new to general surgery, ultrasound has been used for many years by other non-radiology specialties such as obstetrics and cardiology. Although the equipment is readily available, there are few data regarding the accuracy of examinations performed by general surgeons. Such studies would be potentially helpful in addressing credentialing issues raised as surgeons begin to perform ultrasound examinations. We undertook this study to determine if our ultrasound examinations were as accurate as those performed by our local radiologists and those reported in the literature.
Representative ultrasound examinations. Panels A and C are in the transverse plane; panels B and D are in the sagittal plane. Panels A and B show a small right inferior parathyroid adenoma. Panels C and D show a large ledt superior parathyroid. The identity of the two lesions was confirmed at surgery.
At our institutions SPU was a superior technique for localizing abnormal parathyroids than either RPU or nuclear scintigraphy. There is a broad range of sensitivity reported in the literature, but our results are in general agreement with the best reported series. We believe that this finding supports the notion that clinicians, including surgeons, can proficiently perform ultrasound examinations for specific indications.
In our radiology departments, ultrasound was significantly inferior both to the SPU results on the same patients and to the results reported in the literature. There is an obvious potential explanation for this. It is widely noted that ultrasonography is technician-dependent. While high-volume endocrine surgery centers often have radiologists and sonographers with interest and expertise in this field, many endocrine surgeons must rely on radiology departments whose main expertise lies in other areas. Our radiology departments, while generally excellent, did not have the resources required to become expert in this rather limited field. It is not doubted that these and many other radiology departments could obtain superior results given the resources to focus attention in this area.
While RPU was abandoned during the course of this study, nuclear scintigraphy was not. Although our results were less satisfactory than often reported in the literature [14, 15, 16, 17] and less sensitive than SPU, scintigraphy occasionally added valuable information. Nuclear scintigraphy can identify ectopic parathyroids in the neck and upper thorax and can potentially clarify equivocal findings on ultrasound [15, 18]. In one patient in particular with an ectopic parathyroid adenoma in the carotid sheath posterior to the clavicular head, nuclear scintigraphy was very helpful when ultrasound failed to localize the abnormal gland. Our findings are in general agreement with those of Arici et al., who concluded that concordance between ultrasound and nuclear scintigraphy was highly accurate for detecting solitary adenomas [19].
In this study the sensitivity and specificity of SPU were not influenced when other localization tests were performed earlier. Moreover, the presence of concurrent thyroid disease did not statistically alter the effectiveness of SPU. However, at least the occasional patient will have thyroid nodules with sonographic characteristics that make ultrasound especially difficult.
The inability of ultrasound to correctly identify multigland disease was again noted in our series. No patient with multigland disease was correctly identified preoperatively. However, it should be noted that in two patients with hyperplasia all four identified glands were roughly normal in size. Both of these patients were cured with subtotal parathyroidectomy, suggesting there was not a missed fifth gland adenoma.
Ultrasound for parathyroid localization is easily learned and generally takes less than 10–15 minutes to perform. In our hospital and many others, RPU examination requires scheduling the procedure at a later date with a subsequent office visit for follow-up. The added convenience to the surgeon and the patient of having the study performed immediately at the time of initial evaluation cannot be overemphasized. The added time in clinic is feasible for many, but not all, surgeons. For certain high-volume clinics, the surgeon time required for ultrasound might not be cost-effective. Training in ultrasound is available through the American College of Surgeons, among other organizations. Because the technique is thought to be harmless, it can be practiced on volunteers until adequate experience is achieved. Although our data do not address the learning curve, it is our impression that one can become relatively proficient in a short period of time.
We conclude that SPU is a useful adjunct to preoperative planning for directed parathyroidectomy. In selected institutions it may be superior to either RPU or nuclear scintigraphy in localizing abnormal parathyroids preoperatively. Adoption of this technique should be determined by local expertise of both surgeon and radiologist.
Résumé
L’échographie est une des méthodes préférées pour localiser les parathyroïdes anormales. La précision de l’échographie est opérateur-dépendante. Cette étude a été entreprise pour déterminer la précision de l’échographie réalisée par le chirurgien (EC) comparée à celle réalisée par un radiologue (ER) et la scintigraphie (S). On a analysé les dossiers de 74 patients consécutifs porteurs d’un hyperparathyroïdie primitive, non traités, ayant eu une EC au moment de leur visite initiale. Vingt et un patients n’on pas été opérés et ont été exclus de l’analyse. Parmi les 53 autres patients, on a obtenu des ER chez 26 et 52 patients ont eu des S. La parathyroïdectomie dirigée a été réalisée avec l’aide du dosage peropératoire de la parathormone (IOPTH). 46 patients avaient un adénome solitaire diagnostiqué par l’IOPTH et confirmé par l’examen anatomopathologique final. Deux patients avaient une maladie double alors que cinq patients avaient une hyperplasie multiglandulaire. La sensibilité de l’EC pour détecter une glande atteinte et du bon côté (droit vs gauche) a été de 82% et la spécificité de 90%. La sensibilité de l’ER a été de 42% et la spécificité de 92% (n = 26). La sensibilité de la S a été de 44% et la spécificité, de 98% (n = 52). Dans un cas seulement l’ER et la S ont détecté une glande atteinte, non détectée par l’EC. L’EC peut être réalisée avec une précision comparable aux autres séries d’échographie dans la littérature et pourrait même être supérieure à l’ER ou à la scintigraphie dans certaines institutions. Il est important pour les chirurgiens d’être au courant de l’expertise locale si on compte sur les radiologues ou la S pour l’évaluation préopératoire avant de réaliser la parathyroïdectomie dirigée.
Resumen
El ultrasonido es una de las modalidades de preferencia en la localización de paratiroides anormales. La precisión y certeza de ultrasonido es operador - dependiente. El presente estudio fue emprendido con el propósito de determinar la certeza del ultrasonido practicado por el cirujano (USC) en la localización de tumores paratiroideos en comparación con el ultrasonido practicado por un radiólogo (USR) y la centelleografia nuclear (CN). En 74 pacientes consecutivos con hiperparatiroidismo primario no tratado se practicó USR en la consulta inicial. 21 pacientes no fueron sometidos a cirugía y se excluyeron del análisis. En los 53 restantes, se practicó USR en 26 y en 52 CN. La paratiroidectomía dirigida fue realizada con determinación intraoperatoria de hormona paratiroidea (IOPTH). Cuarenta y seis pacientes presentaron un adenoma único a juzgar por la IOPTH y la patología final. Dos presentaron enfermedad glandular doble y 5 hiperplasia multiglandular. La sensibilidad de la USC fue 82% y la especificidad 90% en cuanto a la detección de glándulas anormales en el lado correcto (derecho vs. izquierdo). La sensibilidad de la USR fue 42% y la especificidad 92% (n = 26). La sensibilidad de la CN fue 44% y la especificidad 98% (n = 52). En sólo 1 caso la USR o la CN detectaron una glándula que no fue hallada en la USC. La USC fue realizada con una certeza comparable a otras series de ultrasonido informadas en la literatura, y puede ser superior a la USR o la CN en algunas instituciones. Es importante que los cirujanos sean conscientes de las pericias disponibles en cada institución cuando se fundamenten en la USR o la CN en el proceso de evaluación previa a una paratiroidectomía dirigida.
References
SH Burkey WH Snyder SuffixIII F Nwariaku et al. (2003) ArticleTitleDirected parathyroidectomy: feasibility and performance in 100 consecutive patients with primary hyperparathyroidism Arch. Surg. 138 604–608 Occurrence Handle10.1001/archsurg.138.6.604 Occurrence Handle12799330
FD Moore SuffixJr F Mannting M Tanasijevic (1999) ArticleTitleIntrinsic limitations to unilateral parathyroid exploration Ann. Surg. 230 382–388 Occurrence Handle10.1097/00000658-199909000-00011 Occurrence Handle10493485
SJ Gallacher P Kelly J Shand et al. (1993) ArticleTitleA comparison of 10 MHz ultrasound and 201-thallium/99m-technetium subtraction scanning in primary hyperparathyroidism Postgrad. Med. J. 69 376–380 Occurrence Handle1:STN:280:ByyA2cfhtVA%3D Occurrence Handle8346133
DF Hewin TJ Brammar J Kabala et al. (1997) ArticleTitleRole of preoperative localization in the management of primary hyperparathyroidism Br. J. Surg. 84 1377–1380 Occurrence Handle10.1111/j.1365-2168.1997.00598.x Occurrence Handle1:STN:280:DyaK1c%2FislKlsQ%3D%3D Occurrence Handle9361592
SB Reeder TS Desser RJ Weigel et al. (2002) ArticleTitleSonography in primary hyperparathyroidism: review with emphasis on scanning technique J. Ultrasound Med. 21 539–552 Occurrence Handle12008817
HT Billy DR Rimkus S Hartzman et al. (1995) ArticleTitleTechnetium-99m-sestamibi single agent localization versus high resolution ultrasonography for the preoperative localization of parathyroid glands in patients with primary hyperparathyroidism Am. Surg. 61 882–888 Occurrence Handle1:STN:280:ByqA1Mfgt1A%3D Occurrence Handle7668462
DB Koslin J Adams P Andersen et al. (1997) ArticleTitlePreoperative evaluation of patients with primary hyperparathyroidism: role of high-resolution ultrasound Laryngoscope 107 1249–1253 Occurrence Handle10.1097/00005537-199709000-00017 Occurrence Handle1:STN:280:ByiH3snmtl0%3D Occurrence Handle9292612
JN Attie A Khan WM Rumancik et al. (1988) ArticleTitlePreoperative localization of parathyroid adenomas Am. J. Surg. 156 323–326 Occurrence Handle1:STN:280:BiaD38znsVc%3D Occurrence Handle3052123
PO Hasselgren JP Fidler (1992) ArticleTitleFurther evidence against the routine use of parathyroid ultrasonography prior to initial neck exploration for hyperparathyroidism Am. J. Surg. 164 337–340 Occurrence Handle1:STN:280:ByyD3snit1A%3D Occurrence Handle1415940
OA Preventza S Yang JJ Karo et al. (2000) ArticleTitlePre-operative ultrasonography guiding minimal, selective surgical approach in primary hyperparathyroidism Int. Surg. 85 99–104 Occurrence Handle1:STN:280:DC%2BD3crht1yhsA%3D%3D Occurrence Handle11071323
GP Purcell FM Dirbas RB Jeffrey et al. (1999) ArticleTitleParathyroid localization with high-resolution ultrasound and technetium Tc 99m sestamibi Arch. Surg. 134 824–828 Occurrence Handle10.1001/archsurg.134.8.824 Occurrence Handle1:STN:280:DyaK1MzntFCjtg%3D%3D Occurrence Handle10443804
JE Boggs GL Irvin SuffixIII AS Molinari et al. (1996) ArticleTitleIntraoperative parathyroid hormone monitoring as an adjunct to parathyroidectomy Surgery 120 954–958 Occurrence Handle1:STN:280:ByiC3MnjvFY%3D Occurrence Handle8957480
LL Gordon WH Snyder SuffixIII F Wians SuffixJr et al. (1999) ArticleTitleThe validity of quick intraoperative parathyroid hormone assay: an evaluation in seventy-two patients based on gross morphologic criteria Surgery 126 1030–1035 Occurrence Handle10.1067/msy.2099.101833 Occurrence Handle1:STN:280:DC%2BD3c%2Fms1Wgsw%3D%3D Occurrence Handle10598184
NR Borley RE Collins M O’Doherty et al. (1996) ArticleTitleTechnetium-99m sestamibi parathyroid localization is accurate enough for scan-directed unilateral neck exploration Br. J. Surg. 83 989–991 Occurrence Handle1:STN:280:BymH3cfotFU%3D Occurrence Handle8813796
RS Haber CK Kim WB Inabnet (2002) ArticleTitleUltrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m) technetium sestamibi scintigraphy Clin. Endocrinol. (Oxf.) 57 241–249 Occurrence Handle10.1046/j.1365-2265.2002.01583.x
F Pattou G Torres A Mondragon-Sanchez et al. (1999) ArticleTitleCorrelation of parathyroid scanning and anatomy in 261 unselected patients with sporadic primary hyperparathyroidism Surgery 126 1123–1131 Occurrence Handle10.1067/msy.2099.101579 Occurrence Handle1:STN:280:DC%2BD3c%2Fms1Wntg%3D%3D Occurrence Handle10598197
W Shen U Sabanci ET Morita et al. (1997) ArticleTitleSestamibi scanning is inadequate for directing unilateral neck exploration for first-time parathyroidectomy Arch. Surg. 132 969–974 Occurrence Handle1:STN:280:ByiH2cjhsFw%3D Occurrence Handle9301609
RA Sofferman MH Nathan (1998) ArticleTitleThe ectopic parathyroid adenoma: a cost justification for routine preoperative localization with technetium Tc 99m sestamibi scan Arch. Otolaryngol. Head Neck Surg. 124 649–654 Occurrence Handle1:STN:280:DyaK1czgtFentw%3D%3D Occurrence Handle9639474
C Arici WK Cheah PH Ituarte et al. (2001) ArticleTitleCan localization studies be used to direct focused parathyroid operations? Surgery 129 720–729 Occurrence Handle10.1067/msy.2001.114556 Occurrence Handle1:STN:280:DC%2BD3MzitVOhsg%3D%3D Occurrence Handle11391371
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Husen, R., Kim, L. Accuracy of Surgeon-performed Ultrasound in Parathyroid Localization. World J. Surg. 28, 1122–1126 (2004). https://doi.org/10.1007/s00268-004-7485-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-004-7485-2