Abstract.
Peritoneal implantation from hepatocellular carcinoma (HCC) after hepatic resection is infrequent, and information on risk factors and long-term survival of such patients is lacking. The clinicopathologic features and risk factors of 16 HCC patients after hepatic resection who developed peritoneal implantation from an HCC and the prognosis after surgical resection of these HCC implants were assessed. The clinical features of 16 HCC patients after hepatic resection undergoing resection of peritoneal HCC implants (P-HCC) from 1986 and 2000 were reviewed. The clinical features and outcomes of 195 HCC patients undergoing hepatectomy without recurrence (NR-HCC) were used for comparison. During 1986 and 2000 a total of 749 HCC patients underwent hepatic resection. Of these 749 patients, 465 (62.1%) had HCC recurrence after hepatic resection during the follow-up period (median 26 months). Of the 465 patients, 26 (5.6%) developed peritoneal implants, and 16 of them underwent resection. Multivariate logistic regression analysis revealed that a high α-fetoprotein (AFP) level and capsular invasion by the tumor cells may predispose posthepatectomy patients to peritoneal implantation from their HCCs. The overall survival of the P-HCC patients after peritoneal implant resection was similar to that of the NR-HCC patients. An elevated AFP level might be regarded as a significant prognostic factor for poor overall survival (p = 0.0577) after resection of peritoneal implants from HCCs. Peritoneal implantation occurs infrequently in posthepatectomy patients with an HCC. Elevated AFP values and capsule invasion by tumor cells may predispose posthepatectomy patients to peritoneal implantation from HCCs. Surgical resection of peritoneal implants from HCCs may prolong survival in selected patients. Elevated AFP levels may be regarded as a possibly significant prognostic factor for poor overall survival after resection of peritoneal HCC implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) is a common disease in Taiwan, with an annual age-adjusted incidence of 27.7 per 100,000 population. It is the leading cause of cancer-related death among men and the second most common among women in Taiwan [1].
Peritoneal implantation from an HCC is unusual, being found at autopsy or laparoscopy with an incidence ranging from 2% to 16% [2]. Patients with an HCC who develops peritoneal implantation have generally been considered terminally ill, and surgical treatment has therefore not been considered useful for improving patient survival. Few case reports describe patients surviving for several months following the detection of peritoneal metastasis [3]. Recently, however, surgical resection in HCC patients with peritoneal implantation has been reported to be justified in that it might prolong survival in selected patients [4] The clinicopathologic features predicting the outcome of HCC patients after hepatic resection of HCC peritoneal implants has never been clarified, and the prognostic factors influencing the long-term outcome remain unknown. This aim of this study was determine the risk factors for peritoneal implantation from an HCC after hepatic resection and prognostic factors to predict long-term survival.
Materials and Methods
From 1986 to 2000 a total of 749 consecutive HCC patients underwent hepatic resection at the Department of Surgery, Chang-Gung Memorial Hospital, Taipei, Taiwan. Preoperative evaluation of patients with an HCC included routine laboratory examination, ultrasonography (US), abdominal computed tomography (CT), selective angiography, and magnetic resonance imaging (MRI). All of the 749 patients discharged from the hospital after hepatic resection were closely followed at regular intervals until death or until the time of this writing. The duration of follow-up ranged from 1.2 to 180.3 months (median 26.0 months).
During the follow-up period, 465 patients (62.1%) had a recurrence of HCC after hepatic resection: 382 (82.2%) developed intrahepatic recurrence, 57 (12.2%) distant metastases, and 26 (5.6%) peritoneal implantation. Of the 26 patients with isolated peritoneal implantation, 16 underwent resection (P-HCC group). Peritoneal implantation was defined as metachronous HCC occurrence in the peritoneum after hepatic resection for primary HCC. Patients with concomitant peritoneal involvement or metastasis of the HCC were excluded from this study. Altogether, 43 patients with incomplete data or loss of follow-up and 46 patients dying within 1 month after operation (surgical mortality 6.1%) were excluded from this investigation (51 HCC patients with recurrence and 37 HCC patients without recurrence). The remaining 195 patients had no metastasis or recurrence during the follow-up period (NR-HCC group).
Differences in demographics, symptomatology, physical examination, laboratory data, operative finding, pathologic features, and survival between the P-HCC and NR HCC groups were compared. The histopathologic findings of the HCCs were divided into four grades according to Edmondson and Stainer’s system. Grades I and II were considered low-grade HCCs and grades III and IV high-grade HCCs. Clinical features were grouped as an α-fetoprotein (AFP) level < 400 ng/ml versus AFP level > 400 ng/ml, the presence of hepatitis B surface antigen (HBsAg) versus the absence of HBsAg, and the presence of capsule invasion of the tumor versus its absence.
Follow-up Study
Follow-up evaluation involved clinical physical examinations and blood chemistry tests at each visit. The remnant liver was examined using US every 3 months, and the serum AFP was measured by radioimmunoassay at least every 3 months. When US detected a new lesion or an elevated AFP level was noted, an abdominal CT, MRI, or liver scan was performed for confirmation. Chest radiography was performed every 6 months for pulmonary metastasis evaluation. If a patient complained of bone pain, a bone scan was performed to detect any metastasis that might be present. If any of the above procedures indicated recurrence, the patient was readmitted for further investigation, which included an angiographic evaluation or MRI.
Treatment of Peritoneal Implantation from HCCs
Resection of an HCC recurrence was the treatment of choice if the tumor was considered resectable. There were 16 peritoneal implantation patients who met the criteria of surgical resection and were eligible for resection [3, 4]. All 16 were discharged with an uneventful postoperative course and underwent regular outpatient clinic follow-up ranging from 2.1 to 81.6 months (median 16 months).
Statistical Analysis
All data are presented as the percent of patients or the mean with standard deviation. Continuous data were compared by an independent two-sample t-test. Pearson’s χ2 test and Fisher’s exact test were used for nominal variables if appropriate. Multiple logistic regression analysis was conducted for modeling the combination of clinical features that could predict peritoneal implantation. The survival rate was calculated and plots constructed using the Kaplan-Meier method, and groups were compared using the log-rank test. SPSS computer software package (Version 10.0; SPSS, Chicago, IL, USA) was used for statistical analyses. A p value < 0.05 was considered statistically significant.
Results
There were 13 male patients and 3 female patients with ages ranging from 8 to 87 years (mean 47.1 ± 15.6 years). The P-HCC and NR-HCC groups had similar age distributions, gender ratios, clinical features, and percent of patients with underlying liver cirrhosis or Child-Pugh grades (Table 1. More hepatitis B infections were observed in the P-HCC group (p = 0.004) (Table 1), and more P-HCC patients had an AFP level exceeding 400 ng/ml (measured at the time of presentation with the primary tumor) than did those in the NR-HCC group (p = 0.020). Other biochemical data were similar in the two groups (Table 2).
The P-HCC patients had more capsule invasion (p = 0.029), whereas the other operative, macroscopic, and microscopic findings were similar in the two groups (Table 3). Multivariate analysis revealed that elevated AFP levels and more capsular invasion might predispose posthepatectomy patients to peritoneal implantation from their HCCs (Table 4).
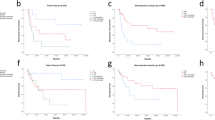
All 211 patients discharged from the hospital after hepatic resection were closely followed up at regular intervals until death or the time of this writing. Follow-up duration ranged from 1.0 to 182.3 months (median 25.3 months). Overall actuarial survival for the P-HCC, NR-HCC, and HCC patients with recurrence is not shown. The 1-, 3-, and 5-year actuarial survival rates for the P-HCC patients were 62.5%, 34.1%, and 30.1%, respectively; and in the NR-HCC group they were 58.0%, 53.7%, and 44.5%, respectively. The P-HCC patients had a better overall survival after surgical resection than did the HCC patients who had a recurrence at another site after hepatectomy, although the difference was not statistically significant. However, after peritoneal implant resection the P-HCC patients had an overall survival similar to that of the NR-HCC patients (Fig. 1A). Comparison of overall survival for the limited number of patients in the P-HCC group, stratified by the presence of HBsAg, capsule invasion, and elevated AFP, showed that an elevated AFP level was possibly a significant prognostic factor for poor overall survival (p = 0.0577) (Fig. 1B–D).
A. Overall survival curves for 16 patients with peritoneal implantation of hepatocellular carcinoma (P-HCC) and 195 patients undergoing hepatectomy without recurrence of HCC (NR-HCC). B. Survival curves for 16 P-HCC patients: hepatitis B surface antigen (HBsAg)-positive versus HBsAg-negative. C. Survival curves for 16 P-HCC patients: α-fetoprotein (AFp) < 400 ng/ml vs. AFp > 400 ng/ml. D. Survival curves of 16 P-HCC patients: with capsular invasion versus without capsular invasion.
Discussion
In this study, 26 (5.6%) of 465 patients with recurrence of their HCC after hepatectomy developed peritoneal implantation, and 16 of them underwent surgical resection. HCC is a highly malignant cancer that frequently metastasizes to other organs. The most common HCC metastatic sites are lungs, bones, brain, and skin. Other sites of metastasis, including portal lymph nodes, spleen, pancreas, bowel, kidney, adrenal glands, and ovaries, are not usually detected until autopsy [5, 6, 7]. The mode of HCC extrahepatic spread is usually hematogenous, most frequently to the lung. Lymphogenous and infiltrating metastases are relatively infrequent. Peritoneal implantation from an HCC is unusual, with an incidence of 2% to 16% at autopsy or laparoscopy. In an autopsy study, Nakashima et al. reported the incidence of HCC metastasis to the Douglas pouch at 6.2% [6]. The current investigation’s incidence of peritoneal implantation from HCC after hepatectomy was 5.6%.The mechanism of peritoneal implantation from HCC is thought to be rupture of an exophytic HCC into the peritoneal cavity and subsequent seeding of metastatic deposits. Ong et al. and Dixon et al. reported similar observations [8, 9]. Sonoda et al. reported that ruptured HCC evokes the risk of implanted metastasis [10]. Only 4 of the 16 patients (25%) in the current investigation developed peritoneal implantation from a preexisting ruptured HCC, however, which was not different from that in patients without any recurrence after hepatectomy.
Demographics, symptomatology, physical findings, biochemical data, hepatitis status, and associated liver conditions were generally similar for the P-HCC and NR-HCC patients. However, the P-HCC group differed from the NR-HCC in three respects. P-HCC patients had higher HBsAg positivity than the NR-HCC group. Our previous report demonstrated that patients with HCC concomitant with hepatitis B virus (HBV) infection were younger than those with nonhepatitis-, hepatitis C-, and dual hepatitis B and C-related HCC [11, 12]. This age difference may explain why P-HCC patients had higher HBsAg positivity, and so it may not an independent factor for peritoneal implantation demonstrated by multivariate analysis.
Prominently elevated AFP values were noted in the P-HCC group. Previous European and Japanese reports have stressed the importance of the preoperative AFP level as a factor affecting the prognosis of surgically treated patients [13, 14]. It is not understood why an elevated AFP level worsens the surgically treated patients’ prognosis. Perhaps AFP is a unique biologic variable expressing the grade of malignancy and has suppressive effects on the immunologic reaction directed against tumor cells [15, 16]. Some have suggested that an elevated serum AFP level is closely related to the growth and development of hepatitis virus-related HCC [17].
Finally, capsular invasion by tumor was observed more frequently in the P-HCC group. The capsule is a biologic characteristic of tumors. Tumor capsule formation is thought to be an early stage of the tumor: the higher the percentage of well encapsulated tumor, the lower the incidence of tumor emboli and the better the tumor cell differentiation [18]. An immunohistochemical study’s morphologic observation revealed large γδ T cells had increased in the tumor capsule, cells that play a role in defense against tumor expansion [18]. Capsule formation did not, however, significantly contribute to better survival of the P-HCC patients. The prognostic significance of capsular invasion by tumors (which demonstrated an associated higher recurrence rate) needs further investigation, as it may partly explain the risk for peritoneal implantation from HCC after hepatectomy.
The prognosis for patients with advanced gastrointestinal cancer with peritoneal metastasis is poor, as most die within 6 months. Peritoneal metastases from gastrointestinal cancer are often widespread, affecting the entire abdominal cavity and leading to the development of ascites. In contrast, the comparable overall survival rate after resection of the peritoneal HCC implants with that of patients without recurrence justifies aggressive surgical resection of the HCC peritoneal implants in selected cases. The P-HCC patients might have better overall survival after hepatectomy than the HCC patients with recurrence at other sites (p = 0.0833). An elevated AFP level, especially if it exceeds 400 ng/ml, may indicate a poor prognosis for posthepatectomy patients with peritoneal HCC implants. Peritoneal implantation occurs infrequently in posthepatectomy patients with HCCs. Elevated AFP levels and capsule invasion by tumor cells may predispose posthepatectomy patients to peritoneal implantation from their HCC. Surgical resection of the peritoneal HCC implants may prolong survival in selected patients. Elevated AFP levels may be regarded as a possibly significant prognostic factor for poor overall survival after resection of peritoneal HCC implants.
Résumé.
L’implantation péritonéale à partir du cancer hépatocellulaire (HCC) après résection hépatique est rare. On ne dispose pas, cependant, de facteurs de risque et de survie à long terme en ce qui concerne l’implantation péritonéale après hépatectomie pour CHC. On a analysé les données cliniques et pathologiques et les facteurs de risque chez 16 patients porteurs de CHC ayant développé des métastases péritonéales après résection hépatique et on a évalué leur pronostic après résection de ces métastases péritonéales. On a analysé les données cliniques de 16 patients porteurs de CHC (CHC-P) entre 1986 et 2000. Les données cliniques et l’évolution de 195 patients porteurs de CHC ayant eu une résection hépatique sans récidive (CHC-NR) ont servi de groupe de contrôle afin de déceler les facteurs de risque d’implantation péritonéale après résection hépatique pour CHC. Entre 1988 et 2000, 749 patients porteurs de CHC ont eu une résection hépatique. 465 des 749 patients (62.1%) ont eu une récidive de leur CHC après résection pendant la période médiane de suivi de 26 mois. Vingt-six des ces 465 patients (5.6%) ont développé des métastases péritonéales et 16 parmi eux ont eu une résection de celles-ci. Par analyse multivariée (régression logistique) on a trouvé que les valeurs d’alpha-féto protéine (AFP) et l’invasion capsulaire par les cellules tumorales prédisposaient aux métastases péritonéales après résection hépatique pour CHC. La survie globale du groupe CHC-P après résection des métastases péritonéales était similaire à celle des patients du groupe CHC-NR. Un taux élevé d’AFP pourrait être considéré comme un facteur de mauvais pronostic de la survie globale (p = 0.0577) après résection péritonéale de métastase d’origine CHC. Les métastases péritonéales sont rares après résection hépatique pour CHC. Un taux élevé d’AFP et l’invasion capsulaire par les cellules péritonéales pourraient prédisposer aux métastases péritonéales. La résection chirurgicale pourrait prolonger la survie chez certains patients sélectionnés. Un taux élevé d’AFP pourrait être considéré comme un mauvais facteur pronostique pour la survie globale après résection des métastases d’origine CHC.
Resumen.
La implantación peritoneal de células procedentes de un carcinoma hepatocelular (HCC) tras resección hepática es poco frecuente. Por otra parte, existe poca o ninguna información sobre el riesgo que esta implantación conlleva, por lo que a la supervivencia tardía se refiere. Para averiguar el pronóstico de la resección quirúrgica de los implantes peritoneales de células procedente de un HCC se estudian los hallazgos clínico-patológicos y los factores de riesgo en 16 pacientes con HCC que tras resección hepática desarrollaron implantes peritoneales. Se revisa el cuadro clínico de 16 pacientes con HCC, tratados entre 1986 y 2000, que tras resección hepática desarrollaron implantes peritoneales de HCC que fueron extirpados (P-HCC). Para averiguar los factores de riesgo de la implantación peritoneal de HCC tras hepatectomía los 16 pacientes mencionados se comparan con el cuadro clínico y resultados terapéuticos de 195 pacientes con HCC que tras la hepatectomía no desarrollaron recidiva alguna (NR-HCC). De 1988 a 2000, 746 paciente con HCC fueron sometidos a una resección hepática, 465 de los 746 pacientes (62.1%) desarrollaron recidivas tras la resección hepática durante el periodo de seguimiento (media 26 meses). En 26 de los 465 pacientes (5.6%) se produjeron implantes peritoneales que en 16 casos fueron extirpados. Un análisis de regresión logística multivariante demostró que niveles elevados de α-fetoproteína (AFP) así como la invasión de la cápsula hepática por células tumorales predispone, tras hepatectomía, al desarrollo de implantación peritoneal del HCC. En el grupo P-HCC la tasa de supervivencia fue similar a la de los pacientes del grupo NP-HCC. Tras la resección de los implantes peritoneales de HCC, la elevación de la AFP es un signo de mal pronóstico por lo que la supervivencia global se refiere (p = 0.0577). La implantación peritoneal posthepatectomía en pacientes con HCC es poco frecuente. La elevación de la AFP y la invasión capsular por células tumorales predispone a la implantación peritoneal de HCC post-hepatectomía. La extirpación quirúrgica de los implantes peritoneales del HCC puede prolongar la supervivencia en pacientes bien seleccionados. Una α -fetoproteina (AFP) elevada tras resección de los implantes peritoneales del HCC, debe considerarse como un mal factor pronóstico, por lo que a la supervivencia se refiere.
References
Annual Report of Cancer Registration. Department of Health, Executive Yuan, Republic of China, 1998
Y Kasai A Tamaki H Kakita (1977) ArticleTitleSurgical treatment of primary hepatocellular carcinoma Geka Shinryo 19 46–54
H Nakayama T Takayama M Makuuchi et al. (1999) ArticleTitleResection of peritoneal metastasis from hepatocellular carcinoma Hepatogastroenterology. 46 1049–1052 Occurrence Handle1:STN:280:DyaK1M3pvVyjsQ%3D%3D Occurrence Handle10370665
CN Yeh MF Chen LB Jeng (2002) ArticleTitleResection of peritoneal implantation from hepatocellular carcinoma Ann. Surg. Oncol. 9 863–868 Occurrence Handle12417507
YTM Lee DA Geer (1987) ArticleTitlePrimary liver cancer: pattern of metastasis J. Surg. Oncol. 36 26–31 Occurrence Handle1:STN:280:BiiA3MzkvFQ%3D Occurrence Handle3041113
T Nakashima K Okuda M Kojiro et al. (1983) ArticleTitlePathology of hepatocellular carcinoma in Japan: 232 consecutive cases autopsied in ten years Cancer 51 863–877 Occurrence Handle1:STN:280:BiyC3c3otVQ%3D Occurrence Handle6295617
InstitutionalAuthorNameLiver Cancer Study Group of Japan (1987) ArticleTitlePrimary liver cancer in Japan Cancer 60 1400–1411 Occurrence Handle3040216
GB Ong EPH Chu FYK Yu et al. (1965) ArticleTitleSpontaneous rupture of hepatocellular carcinoma Br. J. Surg. 52 123–129 Occurrence Handle1:STN:280:CCqD28%2FkvVE%3D Occurrence Handle14255982
JM Dixon D Nirmul O Eremin (1982) ArticleTitleHemoperitoneum due to traumatic rupture of a hepatoma in a patient with hemochromatosis J. R. Coll. Surg. Edinb. 27 362–363 Occurrence Handle1:STN:280:BiyD1crkvVU%3D Occurrence Handle6294292
T Sonoda T Kanematsu K Takenaka et al. (1989) ArticleTitleRuptured hepatocellular carcinoma evokes risk of implanted metastases J. Surg. Oncol. 41 183–186 Occurrence Handle1:STN:280:BiaA3M3mvFA%3D Occurrence Handle2545975
WC Lee LB Jeng MF Chen (2000) ArticleTitleHepatectomy for hepatitis B-, hepatitis C-, and dual hepatitis B- and C-related hepatocellular carcinoma in Taiwan J. Hepatobiliary. Pancreat. Surg. 7 265–269 Occurrence Handle10.1007/s005340070047 Occurrence Handle1:STN:280:DC%2BD3cvotF2jtQ%3D%3D Occurrence Handle10982625
CN Yeh WC Lee LB Jeng et al. (2002) ArticleTitleHepatic resection for hepatocellular carcinoma in Taiwan Eur. J. Surg. Oncol. 28 652–656 Occurrence Handle10.1053/ejso.2002.1292 Occurrence Handle12359203
InstitutionalAuthorNameCancer of the Liver Italian Program (CLIP) Investigators (1998) ArticleTitleA new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients Hepatology 28 751–755
InstitutionalAuthorNameLiver Cancer Study of Japan (1994) ArticleTitlePredictive factors for long-term prognosis after partial hepatectomy for patients with hepatocellular carcinoma in Japan Cancer 74 2772–2780 Occurrence Handle7954236
RA Murgita EA Goidl S Kontianen et al. (1977) ArticleTitleAlpha-fetoprotein induces suppressor T cell in vitro Nature 267 257–259 Occurrence Handle1:CAS:528:DyaE2sXltlajtLc%3D Occurrence Handle68439
S Yachnin K Soltani EP Lester (1980) ArticleTitleFurther studies on the mechanism of suppression of human lymphocyte transformation by human alpha-fetoprotein J. Allergy Clin. Immunol. 65 127–135 Occurrence Handle1:CAS:528:DyaL3cXhsVCrsbY%3D Occurrence Handle6153188
K Hanazaki S Kajikawa N Koide et al. (2001) ArticleTitlePrognostic factors after hepatic resection for hepatocellular carcinoma with hepatitis C viral infection: univariate and multivariate analysis Am. J. Gastroenterol. 96 1243–1250 Occurrence Handle10.1016/S0002-9270(00)02427-8 Occurrence Handle1:STN:280:DC%2BD3MzntVWlsw%3D%3D Occurrence Handle11316177
IOL Ng ECS Lai MM Ng et al. (1992) ArticleTitleTumor encapsulation in hepatocellular carcinoma: a pathologic study of 189 cases Cancer 70 45–49 Occurrence Handle1:STN:280:By2B1MfjtVU%3D Occurrence Handle1318778
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yeh, CN., Chen, MF. Resection of Peritoneal Implantation of Hepatocellular Carcinoma after Hepatic Resection: Risk Factors and Prognostic Analysis. World J. Surg. 28, 382–386 (2004). https://doi.org/10.1007/s00268-003-7319-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-7319-7