Abstract
Partial hepatectomy is a major upper abdominal operation associated with certain stress to the patient. Successful adaptation to such stress is a prerequisite for survival. Donor hepatectomy with maximal safety is a principal concern during living donor liver transplantation. The purpose of the study was to compare the stress response by assessing cytokines and the acute-phase response induced by hepatectomy in patients with a healthy liver and those with a diseased liver. Fourteen patients undergoing partial right hepatectomy were enrolled in this study. Seven of them were donors for living related liver transplantation (group I, or GI); the other seven were patients with hepatocellular carcinoma due to chronic hepatitis B (Child’s class A) (GII). Blood samples for interleukin-6 (IL-6), tumor necrosis factor-α (TNFα), and C-reactive protein (CRP) assays were collected before the operation, at the beginning and end of the operation, and 24 and 48 hours after the operation. The data were analyzed and compared in the same group using the Friedman test and between groups using the Mann-Whitney U-test. A value of p < 0.05 was regarded as significant. Results showed that resection of the liver in patients with both healthy and disease livers leads to significant increases in IL-6 and CPR but not TNFα. Significantly lower levels of IL-6 before and after operation in GI patients compared to those in GII patients suggests that GI patients adapted to surgical stress more easily than did the GII patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Living related donor liver transplantation (LRLT) is a new form of therapy for pediatric and adult patients with end-stage liver disease that is being used to overcome the problem of organ donor shortage. The major medical and ethical concern of this technique is the risk to the donor. This concern is legitimate, as hepatectomy is major upper abdominal surgery, and the liver plays a major role in maintaining host-defense homeostasis [1]. The reported mortality and morbidity rates associated with hepatectomy are mostly high in patients with liver disease. Although Fan et al. recently reported no in-hospital mortality in their series of 110 patients [2], most centers have reported hospital mortality varying from 2% to 16% and morbidity from 21% to 31% [2, 3, 4]. In contrast, the mortality and morbidity associated with hepatectomy in donors for LRLT is extremely low. Broelsch et al. reported only one death (0.8%) among 228 cases in Europe [5]. Low complication rates with no mortality have also been reported in our series [6] and others [7]. Acceptable stress and safety levels for LRLT donors have been assessed using the arterial ketone body ratio and liver function tests [8].
Surgical stress results in adaptive responses encompassing three major homeostatic axes: endocrine responses involving the hypothalamic-pituitary-adrenal axis; sympathetic nervous system responses; acute-phase response [9]. Successful adaptation to stress is a prerequisite for survival. The net outcome of a successful response is the return of the host to a sustainable homeostatic plateau [9]. If tissue injury from the operation is sufficiently severe to overwhelm local defense mechanisms, overexpression of these essentially protective mechanisms, especially persistent up-regulation of various mediator systems (particularly cytokines), may lead to autodestructive host defense failure disease [10]. Because the outcomes of LRLT donor and liver disease patients undergoing the same hepatectomy are not identical, some differences must exist in host response and defense between the two groups. Interleukin-6 and C-reactive protein, an acute-phase protein, have been shown to be the most specific and sensitive indicators of trauma and infection [11, 12, 13]. The purpose of this study was to evaluate the cytokines and the acute-phase response induced by hepatectomy in patients with healthy and diseased livers and to compare them.
Patients and Methods
The Hospital Ethics Committee approved this study. After obtaining written informed consent, 14 patients undergoing partial right hepatectomy were enrolled in the study. Seven were donors for LRLT (group I, or GI); the other seven were patients with hepatocellular carcinoma due to chronic hepatitis B (Child’s class A) (group II, or GII).
All patients were subjected to the same anesthesia, which was induced with sodium pentothal, fentanyl, and succinylcholine intravenously for tracheal intubation. The anesthesia was maintained with isoflurane and N2O/O2 (1:1). Atracurium was used as a muscle relaxant. All patients were monitored with electrocardiography (ECG), an arterial line for continuous blood pressure monitoring, central venous pressure (CVP), pulse oximetry, end-tidal CO2, body temperature, and urine output. Blood samples were collected before the operation, at the beginning and end of the operation, and 24 and 48 hours after operation. The blood was collected in a heparinized tube, which was immediately placed on ice and centrifuged. The serum was stored at −70°C until measurement. C-reactive protein (CRP) was assessed with an enzyme-linked immunosorbent assay (ELISA) using a commercial ELISA kit (Eurogenetics, Tessenderlo, Belgium), the sensitivity of which is 1 μg/ml. Interleukin-6 (IL-6) and tumor necrosis factor-α (TNFα) were also assessed by ELISA kits (Endogen, Woburn, MA, USA) whose sensitivities were < 1 pg/ml and < 5 pg/ml, respectively.
The preoperative diagnosis, intraoperative complications (e.g., blood loss), the blood products used, and the postoperative morbidity and mortality were recorded, analyzed, and compared. Morbidity was defined as a systemic inflammatory response such as fever > 38°C, tachypnea (> 20 breaths/min), or tachycardia (> 90/beats/min) for more than 48 hours and dysfunction of at least one organ (prolonged ventilatory support or vasopressors required for more than 48 hours). Data were given as the mean ± SD. Differences between groups were tested using the Mann-Whitney U-test. Changes in the same group were tested using Friedman’s test. A value of p < 0.05 was considered significant.
Results
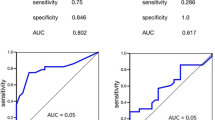
Table 1 shows the patients’ characteristics and changes in the serum CRP, IL-6, and TNFα levels. Figure 1 shows the changes in IL-6, which increased significantly in both groups 24 hours after the operation; GII patients consistently had significantly higher levels than GI patients. Figure 2 shows the changes in CRP, which increased significantly 24 hours after the operation in both groups, with no significant difference noted between groups. Patients from the donor group were all free from morbidity and mortality, whereas two of the seven patients from the hepatoma group had morbidity due to sepsis and multiple organ dysfunction.
Discussion
Our results show that resection of the liver in patients with healthy or diseased liver leads to a significant increase in IL-6 and CPR but not in TNFα. Among them, only IL-6 exhibited a significant difference between groups. The difference was observed even before the operation and remained higher postoperatively in GII patients than in GI patients.
Interleukin-6, a cytokine that has both pro- and antiinflammatory properties [14], is known to have multiple functions. It is important not only for inflammation and immunologic function, it is required for acute-phase induction, which has been regarded as part of the attempt to maintain homeostasis [15]. Furthermore, IL-6 is an important component of the early signal pathway leading to liver regeneration [16, 17]. Impaired hepatocyte proliferation and regeneration with subsequent liver failure after hepatectomy was observed in IL-6 −/− knockout mice [18]. Liver failure in such mice after partial hepatectomy can be prevented and the capacity of hepatocyte proliferation restored by injecting IL-6 before the operation. This indicates that IL-6 is fundamentally important for liver regeneration [18]. An elevated IL-6 level before operation in a hepatoma patient was probably due to the tumor and the associated hepatitis having injured the liver cells. After hepatectomy, there was a significant increase in the IL-6 level associated with increased CRP, indicating that the liver regeneration process was activated in both patient groups (Table 1; Figs. 1, 2). Although IL-6 is necessary for initiating the process of liver regeneration, uncontrolled and prolonged action of cytokines is potentially harmful. Elevated IL-6, but not IL-1 or TNFα, has been found to be correlated with the state of critical illness, such as septic shock [19, 20] or multiple organ failure [21]; it has also been correlated with the mortality rate [19, 20]. Therefore excessive expression of IL-6 is thought to be a sensitive predictor of the development of multiple organ failure [19, 21]. The significantly higher IL-6 levels before and after operation in GII patients compared to those in GI patients suggests that the GII patients are at higher risk of developing postoperative complications than are those in group I.C-reaction protein, an acute-phase protein, is now accepted to be an important indicator of the acute-phase response to surgical injury [12, 13]. It serves an important function in restoring homeostasis after infection and inflammation [22]. The production of acute-phase proteins requires a proinflammatory cytokine as mediator [23, 24]. Among the proinflammatory cytokines, only recombinant IL-6 is capable of inducing CRP mRNA and CRP-protein synthesis [25]. Activation of the IL-6 receptor complex activates JAK tyrosine kinases [26, 27], and it subsequently induces the production of acute-phase proteins [27, 28]. Some reports showed that a high preoperative CRP level is associated with increased postoperative infectious complications after cardiac surgery [13, 29], but another found that CRP is less sensitive than IL-6 as an early predictor of the outcome of pancreatitis [21].
The arterial ketone body ratio, which reflects the hepatic mitochondrial redox potential, and liver enzyme assays have been used to show that the stress of hepatectomy in living liver donors is acceptable [8, 30]. The current study shows that resection of healthy and diseased livers leads to a significant increase in IL-6 and CPR but not TNFα. A significantly lower IL-6 level before and after operation in the GI patients compared to that in the GII patients suggests that the GI patients adapted to surgical stress better than did the GII patients.
Résumé.
L’hépatectomie partielle est une intervention chirurgicale majeure associée à certain stress pour le patient. Vaincre ce stress est essentiel à la survie. La sécurité est un souci réel au cours d’une transplantation hépatique avec donneur vivant. L’objectif de cette étude a été de comparer la réponse au stress par l’évaluation des cytokines et de la réponse de la phase aiguë induites par l’hépatectomie et de les comparer entre les patients porteurs d’un foie sain et malade. Quatorze patients ayant eu une hépatectomie droite ont été inclus dans cette étude. Sept étaient des donneurs vivants (Groupe I); les sept autres étaient des patients avec un cancer hépatocellulaire sur hépatite chronique B (Child A) (Groupe II). On a fait des prélèvements sanguins pour doser l’ll-6, le TNFα et la C-reactive protéine avant, au début et à la fin de l’opération, 24 et 48 heures après la fin de l’intervention. Les données ont été analysées et comparées entre elles par le test de Friedman à l’intérieur d’un même groupe et par le test de Mann-Whitney entre les deux groupes. La valeur p < 0.05 a été prise comme significative. Les résultats montrent que la résection du foie qu’il soit sain ou malade, était associée à une augmentation significative de l’ll-6 et de la CPR mais pas du TNFα. Un niveau significativement plus bas d’ll-6 avant et après opération dans le groupe I en comparaison au groupe II suggère que les patients du groupe I s’adaptent mieux au stress que les patients du groupe II.
Resumen.
La hepatectomía parcial es una de las operaciones del compartimento superior del abdomen que más estresan al paciente. Su adaptación a este estrés es un prerequisito fundamental para su supervivencia. La seguridad en la extracción de la porción del hígado que se dona es condición indispensable para el trasplante con donantes vivos. El objetivo del estudio fue comparar, mediante la determinación de las citocinas y otros parámetros de la fase aguda postraumática, la respuesta a la agresión, producida por la hepatectomía entre pacientes con hígado sano frente a los que aquejaban una afección hepática. Se estudiaron 14 pacientes que sufrieron una hepatectomía parcial derecha. 7 eran donantes vivos y sanos (GI); otros 7 padecían de un carcinoma hepatocelular secundario a una hepatitis B (estadio A de Child) (G II). Se obtuvieron muestras de sangre para la determinación de la IL-6, TNF α y proteína C reactiva (CPR) antes de la intervención, al principio y al final de la misma y a las 24 y 48 horas del postoperatorio. Los parámetros obtenidos se analizaron y compararon utilizando la prueba de Friedman entre sujetos del mismo grupo y el test U de Mann-Whitney para la comparación entre ambos grupos; una p < 0.05 se consideró como significativa. Los resultados demostraron que la hepatectomía, tanto en sujetos con hígado sano como en pacientes con el hígado enfermo, originaba un incremento significativo de la IL-6 y de la CPR, pero no del TNFα. Los niveles más bajos de IL-6 antes y después de la operación en el grupo GI en relación con los obtenidos en el grupo GIl sugieren, que los sujetos del grupo GI estaban mejor adaptados al estrés que los del grupo GII.
References
G Matuschak J Rinalfo M Pinsky et al. (1987) ArticleTitleEffect of end-stage liver failure on the incidence and resolution of the adult respiratory distress syndrome J. Crit. Care 2 162–173
ST Fan CM Lo CL Liu et al. (1999) ArticleTitleHepatectomy for hepatocellular carcinoma: toward zero hospital deaths Ann. Surg. 229 322–330 Occurrence Handle10.1097/00000658-199903000-00004 Occurrence Handle1:STN:280:DyaK1M7nsVKlsw%3D%3D Occurrence Handle10077043
R Doci L Gennari P Bignami et al. (1995) ArticleTitleMorbidity and mortality after hepatic resection of metastases from colorectal cancer Br. J. Surg. 82 377–381 Occurrence Handle1:STN:280:ByqA3MnjvFA%3D Occurrence Handle7796016
S Miyagawa M Makuuchi S Kawasak et al. (1955) ArticleTitleCriteria for safe hepatic resection Am. J. Surg. 169 589–594 Occurrence Handle10.1016/S0002-9610(99)80227-X
CE Broelsch M Malago G Testa et al. (2000) ArticleTitleLiving donor liver transplantation in adults: outcome in Europe Liver Transpl. 6 S64–S65 Occurrence Handle1:STN:280:DC%2BD3M%2FmtlCqug%3D%3D Occurrence Handle11084088
CL Chen YS Chen VH Villa Particlede et al. (2000) ArticleTitleMinimal blood loss living donor hepatectomy Transplantation 69 2580–2586 Occurrence Handle1:STN:280:DC%2BD3czmsFKmsg%3D%3D Occurrence Handle10910280
ST Fan (2000) ArticleTitleDonor safety in living donor liver transplantation Liver Transpl. 6 250–251 Occurrence Handle1:STN:280:DC%2BD3c3kt1KjsQ%3D%3D
Y Shimahara M Awane Y Yamaoka et al. (1993) ArticleTitleSafety and operative stress for donors in living-related partial liver transplantation Transplant. Proc. 25 1081–1083 Occurrence Handle1:STN:280:ByyC1c7psFA%3D Occurrence Handle8442049
R Udelsman NJ Holbrook (1994) ArticleTitleEndocrine and molecular responses to surgical stress Curr. Probl. Surg. 31 653–720 Occurrence Handle1:STN:280:ByuA38%2FkslE%3D Occurrence Handle8045159
FB Cerra JH Siegel B Coleman et al. (1980) ArticleTitleSeptic autocannibalism: a failure of exogenous nutritional support Ann. Surg. 192 570–580 Occurrence Handle1:STN:280:Bi6D3sfhvVw%3D Occurrence Handle6775605
M Shimada T Matsumata A Taketomi et al. (1995) ArticleTitleThe role of interleukin-6, interleukin-16, tumor necrosis factor-alpha and endotoxin in hepatic resection Hepatogastroenterology. 42 691–697 Occurrence Handle1:STN:280:BymA2MfotFM%3D Occurrence Handle8751236
N Brewster C Guthrie J McBirnie (1994) ArticleTitleCRP levels as a measure of surgical trauma: a comparison of different general surgical procedures J. R. Coll. Surg. Edinb. 39 86–88 Occurrence Handle1:STN:280:ByuA3svos1I%3D Occurrence Handle7520075
U Boeken P Feindt N Zimmermann et al. (1998) ArticleTitleIncreased preoperative C-reactive protein (CRP) values without signs of an infection and complicated course after cardiopulmonary bypass (CPB) operations Eur. J. Cardiothorac. Surg. 13 541–545 Occurrence Handle10.1016/S1010-7940(98)00062-1 Occurrence Handle1:STN:280:DyaK1czis1Klug%3D%3D Occurrence Handle9663535
SM Opal VA DePalo (2000) ArticleTitleAnti-inflammatory cytokines Chest 117 1162–1172 Occurrence Handle1:CAS:528:DC%2BD3cXjtFahsb0%3D Occurrence Handle10767254
KL Streetz T Luedde MP Manns et al. (2000) ArticleTitleInterleukin 6 and liver regeneration Gut 47 309–312 Occurrence Handle10.1136/gut.47.2.309 Occurrence Handle1:CAS:528:DC%2BD3cXlvVygu7k%3D Occurrence Handle10896929
M Koga H Ogasawara (1991) ArticleTitleInduction of hepatocyte mitosis in intact adult rat by interleukin-1 alpha and interleukin-6 Life Sci. 49 1263–1270 Occurrence Handle10.1016/0024-3205(91)90139-3 Occurrence Handle1:CAS:528:DyaK3MXmtVGksbg%3D Occurrence Handle1943441
D Maione E Carlo ParticleDi W Li et al. (1998) ArticleTitleCoexpression of IL-6 and soluble IL-6R causes nodular regenerative hyperplasia and adenomas of the liver EMBO J. 17 5588–5597 Occurrence Handle10.1093/emboj/17.19.5588 Occurrence Handle1:CAS:528:DyaK1cXmvVyjs7w%3D Occurrence Handle9755159
DE Cressman LE Greenbaum RA DeAngelis et al. (1996) ArticleTitleLiver failure and defective hepatocyte regeneration in interleukin-6-deficient mice Science 274 1379–1383 Occurrence Handle10.1126/science.274.5291.1379 Occurrence Handle1:CAS:528:DyaK28XntFKlsrg%3D Occurrence Handle8910279
P Damas D Ledoux M Nys et al. (1992) ArticleTitleCytokine serum level during severe sepsis in human IL-6 as a marker of severity Ann. Surg. 215 356–362 Occurrence Handle1:STN:280:By2B3MvpvV0%3D Occurrence Handle1558416
CJ Fisher SuffixJr SM Opal JF Dhainaut et al. (1993) ArticleTitleInfluence of an anti-tumor necrosis factor monoclonal antibody on cytokine levels in patients with sepsis: the CB0006 Sepsis Syndrome Study Group Crit. Care Med. 21 318–327 Occurrence Handle8440099
AC Beaux ParticleDe AS Goldie JA Ross et al. (1996) ArticleTitleSerum concentrations of inflammatory mediators related to organ failure in patients with acute pancreatitis Br. J. Surg. 83 349–353
H Baumann J Gauldie (1994) ArticleTitleThe acute phase response Immunol. Today 15 74–80 Occurrence Handle10.1016/0167-5699(94)90137-6 Occurrence Handle1:CAS:528:DyaK2cXisVWrurc%3D Occurrence Handle7512342
I Kushner DL Rzewnicki (1994) ArticleTitleThe acute phase response: general aspects Baillieres Clin. Rheumatol. 8 513–530 Occurrence Handle1:STN:280:ByqD2c3nvFw%3D Occurrence Handle7525083
MZ Mazlam HJ Hodgson (1994) ArticleTitleInterrelations between interleukin-6, interleukin-1 beta, plasma C-reactive protein values, and in vitro C-reactive protein generation in patients with inflammatory bowel disease Gut 35 77–83 Occurrence Handle1:STN:280:ByuC2c%2FitF0%3D Occurrence Handle8307455
JV Castell MJ Gomez-Lechon M David et al. (1990) ArticleTitleAcute-phase response of human hepatocytes: regulation of acute-phase protein synthesis by interleukin-6 Hepatology 12 1179–1186 Occurrence Handle1:CAS:528:DyaK3MXktVOlsA%3D%3D Occurrence Handle1699862
T Kishimoto T Taga S Akira (1994) ArticleTitleCytokine signal transduction Cell 76 253–262 Occurrence Handle8293462
UM Wegenka J Buschmann C Lutticken et al. (1993) ArticleTitleAcute-phase response factor, a nuclear factor binding to acute-phase response elements, is rapidly activated by interleukin-6 at the posttranslational level Mol. Cell. Biol. 13 276–288 Occurrence Handle1:CAS:528:DyaK3sXhsVGktbs%3D Occurrence Handle7678052
S Akira Y Nishio M Inoue et al. (1994) ArticleTitleMolecular cloning of APRF, a novel IFN-stimulated gene factor 3 p91-related transcription factor involved in the gp130-mediated signaling pathway Cell 77 63–71 Occurrence Handle1:CAS:528:DyaK2cXkslGjtLk%3D Occurrence Handle7512451
W Haupt W Hohenberger R Mueller et al. (1997) ArticleTitleAssociation between preoperative acute phase response and postoperative complications Eur. J. Surg. 163 39–44 Occurrence Handle1:STN:280:ByiC1c%2FlvVI%3D Occurrence Handle9116110
Y Shimahara M Awane Y Yamaoka et al. (1992) ArticleTitleAnalyses of the risk and operative stress for donors in living-related partial liver transplantation Transplantation 54 983–988 Occurrence Handle1:STN:280:ByyC3c3hvFY%3D Occurrence Handle1465792
Acknowledgments.
This study is partly supported by grant NSC87-2314-B182-049 from the National Science Council, Republic of China.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lan, AM., Luk, HN., Goto, S. et al. Stress Response to Hepatectomy in Patients with a Healthy or a Diseased Liver. World J. Surg. 27, 761–764 (2003). https://doi.org/10.1007/s00268-003-6955-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-6955-2