Abstract
Cirrhosis of the liver appears to have an unfavorable prognosis in the surgical patient. The aim of this study was to determine risk factors for morbidity and mortality in patients with cirrhosis undergoing nonhepatic surgery. We studied 135 patients with liver cirrhosis undergoing nonhepatic procedures and 86 controls matched by age, sex, and preoperative diagnosis. Preoperative, intraoperative, and postoperative variables associated with 30-day mortality and morbidity were assessed by univariate and multivariate analyses. Patients with cirrhosis showed higher blood transfusion requirements, longer length of hospital stay, and a higher number of complications than controls. The mortality rate was 16.3% in cirrhotics and 3.5% in controls. By univariate analysis, the need for transfusions, prothrombin time, and Child-Pugh score were significantly associated with postoperative liver decompensation, whereas duration of surgery, prothrombin time, Child-Pugh score, cirrhosis-related complications, and general complications were significantly associated with mortality. In the multivariate analysis, Child-Pugh score (odds ratio [OR] 24.4; 95% confidence interval [CI] 5.5 to 106); duration of surgery (OR 5; 95% CI 1.2 to 15.6), and postoperative general complications (OR 3.7; 95% CI 3.4 to 6.4) were independent predictors of mortality. Patients with cirrhosis undergoing nonhepatic operations are at significant risk of perioperative complications leading to death. Independent variables associated with perioperative mortality include preoperative Child-Pugh score, the duration of surgery, and the presence of postoperative general complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
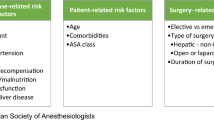
A variety of conditions requiring operation, particularly gallstone disease and the complications of peptic ulcer disease, often arise in patients with liver cirrhosis. Anesthesia and surgery are known to have decompensatory effects on patients with compromised liver function, and previous publications have reported greater morbidity and mortality in patients with cirrhosis undergoing nonhepatic procedures [1, 2, 3, 4, 5, 6]. Retrospective investigations have identified multiple clinical and laboratory variables that contributed to increased perioperative morbidity and mortality rates in cirrhotic patients who underwent nonderivative abdominal surgery [7, 8, 9]. Moreover, it has been shown that there is a correlation between the number of risk factors identified by multivariate analyses and the rate of perioperative complications [9].
We compared our experience with nonhepatic surgery in patients with cirrhosis and controls matched by age, sex, and preoperative diagnosis. The purpose of this study was to provide information about the mortality and morbidity rates for operation in cirrhotic patients and to identify factors associated with mortality within 30 days after surgery.
Materials and Methods
Patients
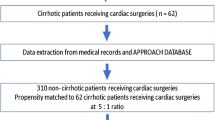
The study population consisted of a cohort of 135 consecutive patients with liver cirrhosis, 89 men and 46 women, with a mean [± standard deviation (SD)] age of 61.5 ± 12.9 years, who underwent any nonhepatic surgical procedure with anesthesia at the Department of Surgery of our hospital between January 1993 and January 2000. For patients with more than one operation during the study, data were collected and analyzed for only the first perioperative experience. The study was approved by our institutional review board.
The diagnosis of liver cirrhosis was made on the grounds of histology and/or laparoscopy, or by direct examination of the liver during abdominal surgery. Cirrhosis was diagnosed preoperatively in 107 patients and at the time of operation in the remaining 28. The etiology of liver cirrhosis was established according to standard criteria for infection with hepatitis B virus (HBV) (positive serum test for hepatitis B surface antigen [HBsAg] (n = 4), hepatitis C virus (HCV) (seropositivity for HCV antibody) (n = 47), and alcoholism (a daily intake of more than 60 g of ethanol in women and more than 80 g in men for more than 5 years) (n = 30). Other causes included autoimmune disease (n = 9) and HCV infection in combination with alcohol use in 36 patients. When no cause was identified, liver cirrhosis was classified as cryptogenic (n = 9). The clinical condition of the patients was graded according to the Child-Pugh classification [10]. Comorbid conditions were classified according to the index developed by Charlson et al. [11].
The control group included 86 nonconsecutive patients, 51 men and 35 women, with a mean (± SD) age of 58.5 ± 16.3 years, who underwent anesthesia and surgery during the same study period and whose characteristics in relation to age, sex, and type of surgical procedure were matched to patients in the group with cirrhosis. It was required that none of these patients had clinical, analytical, or echographic stigmata of liver dysfunction.
Methods
Preoperative data included age; sex; coexisting medical disease; previous surgery; blood cell count; serum albumin; total bilirubin; creatinine concentration; prothrombin time; cause of cirrhosis; the presence of ascites, upper gastrointestinal bleeding, and encephalopathy; Child-Pugh score; and diagnosis of conditions requiring operation categorized into six groups (intestinal disorders, gastric diseases, nonhepatic malignant tumors, biliary tract diseases, abdominal wall diseases, and miscellaneous procedures). Intraoperative data included duration of operation and transfusion requirements. Emergent operations were those performed within 24 hours of admission or from the time surgical consultation was requested.
Postoperative morbidity was defined as complications that occurred during the same hospitalization or as long as 30 days after operation. Recorded surgical wound complications included infection, dehiscence, abscess, fistula, and eventration. Cirrhosis-related complications included ascites (as a new finding or if ascitic volume increased from mild to severe after operation); encephalopathy; upper gastrointestinal bleeding; acute renal failure (defined as an increase of 2 mg/dL or more in the serum creatinine concentration compared with preoperative values, or the need for dialysis in a patient with previously adequate renal function); and liver failure. Pneumonia, congestive heart failure, exacerbation of chronic obstructive pulmonary disease [COPD], urinary tract infection, phlebitis, and paralytic ileus were considered postoperative complications if they represented new findings, and they required that the patient receive additional medical therapy. Other postoperative data recorded included blood cell count, serum albumin, total bilirubin, prothrombin time, Child-Pugh score, length of hospital stay, and death within 30 days of surgery.
Statistical Analysis
The SPSS computer program (MS-DOS, Windows 6.1.2) was used for the analysis of data. The distribution of variables in the group of liver cirrhosis and in the control group was compared. The presence of risk factors for complications and perioperative mortality among patients with cirrhosis was also assessed. Statistical analyses were carried out by using Pearson’s χ 2 test or Fisher’s exact test for the comparison of proportions, and Student’s t-test or analysis of variance (ANOVA) for the comparison of means. Univariate or multivariate linear regression methods and logistic regression models for estimation of odds ratio (OR) and 95% confidence intervals (CI) were used.
Results
Table 1 shows that the group of patients with cirrhosis and the control group were similar with respect to demographic characteristics and preoperative data, including comorbidity, results of laboratory tests, indications of operation, and number of emergent procedures. In the group of 135 patients with cirrhosis, the degree of liver dysfunction before operation was scored as Child-Pugh grade A in 83 patients, B in 41, and C in 11. Most patients (74%) presented with compensated cirrhosis.
In relation to morbidity and mortality data (Table 2), there were statistically significant differences between patients with cirrhosis and controls in the following variables: intraoperative transfusion requirement (39% of cirrhotic patients versus 15% of controls), average length of hospital stay (18 ± 14.4 versus 13.4 ± 13.4 days), overall rate of complications (50.4% versus 29.1%), and 30-day mortality rate (16.3% versus 3.5%). However, as shown in Table 2, there were no significant differences in the occurrence of surgical wound complications and general complications between patients with cirrhosis and controls. Thus the higher number of complications found among patients with cirrhosis was related primarily to decompensation of liver function status. When patients with cirrhosis were grouped according to preoperative Child-Pugh score (Table 3), statistically significant differences between cirrhotic patients and controls persisted for the variables of intraoperative transfusion requirement and average length of hospital stay. With regard to the presence of any complication and mortality within 30 days after surgery, significant differences between cirrhotics and controls were encountered only for Child-Pugh scores B and C (Table 3). Class A patients and controls behaved similarly.
In the group of patients with cirrhosis and in relation to morbidity, univariate analysis identified duration of operation, length of stay, anemia, and preoperative Child-Pugh score as being associated with surgical wound-related complications; transfusion requirements, prothrombin time, and Child-Pugh score with cirrhosis-related complications; and duration of operation only with other general complications (Table 4). In the multivariate analysis, high preoperative Child-Pugh score and blood transfusion were independently associated with the occurrence of cirrhosis-related complications (Table 5).
In the group of patients with cirrhosis and in relation to mortality, duration of operation, high Child-Pugh score, prothrombin time, decompensation of cirrhosis, and other general complications were significantly associated with fatal outcome in the univariate analysis (Table 4); anemia and hypoalbuminemia appeared to be associated with mortality, although statistical significance was not reached. The multivariate analysis identified three variables (high Child-Pugh score, duration of operation, and general complications) that were independently associated with mortality within 30 days after surgery (Table 5).
Discussion
A number of studies have been carried out to assess morbidity and mortality in patients with cirrhosis undergoing nonhepatic surgery [7, 9, 12, 13], but there is a large variability in the results obtained. This variability may be explained in large part by factors attributable to differences in the patients’ surgical diagnoses and by timing of the operation in relation to liver function status [14]. In most of the studies [2, 3, 4, 7, 8, 9, 12, 13, 15], control groups are lacking, whereas comparative studies in which a group of noncirrhotic patients has been included provide information on the mortality and morbidity rates for certain surgical procedures, such as cholecystectomy [14], umbilical herniorrhaphy [16], open-heart surgery [17], peptic ulcer surgery [15], or laparoscopic cholecystectomy [5, 18]. It has been shown that laparoscopic cholecystectomy offers several advantages over open cholecystectomy in patients with cirrhosis, including lower morbidity, shorter operative time, less need for transfusions, and fewer incision-related complications [19, 20, 21].
In the present study, like others [7, 8, 9, 12, 13] patients undergoing different surgical interventions were included; in addition, patients matched by age and sex with similar preoperative diagnoses and operated on during the same study period than patients with cirrhosis served as controls. It should be noted, however, that the present study was not designed for inclusion of an independent evaluation of subgroups of surgical procedures (the number of patients should be larger to analyze preoperative diagnoses separately). The list of procedures given in Table 1 shows baseline data regarding emergency surgery, preoperative diagnoses, and indications for surgery between cirrhotics and controls, but these variables were not selected a priori in the study protocol to be analyzed with respect to outcome. The control group consisted of fewer cases than the group of cirrhotics, because patients in whom clinical, analytical, or liver ultrasound studies were not available to exclude unequivocally the diagnosis of cirrhosis were not eligible. In the selection of cirrhotic patients, all patients with preoperative or intraoperative documented liver cirrhosis undergoing nonhepatic surgery during the study period were included. Eight surgical candidates with Child class C who died at the hospital while awaiting surgery were excluded. The comparison between the study group and the control group revealed more intraoperative transfusion needs and prolonged hospital stay in patients with cirrhosis. These data have not been documented in other studies on morbidity in cirrhotic patients undergoing different nonderivative procedures because a control group was lacking. In the study of Jan and Chen [18] in which safety of laparoscopic cholecystectomy in cirrhotic patients compared to noncirrhotic patients was evaluated, the hospital stay in both groups was similar.
The significantly higher overall rate of complications among patients with cirrhosis was most commonly associated with cirrhosis-related complications—i.e., decompensation of liver function status—given that the rate of surgical wound complications and general complications in patients with cirrhosis and controls was similar. When the analysis of complication was limited to the group of patients with cirrhosis, 50.4% of our patients developed one or more postoperative complications. This percentage is higher than the perioperative complication rate of 30.1% reported by Ziser et al. [9], and it may be explained by the low surgical severity score of many procedures included in their study (e.g., operations on eye, ear, nose, mouth, pharynx, tracheostomy, laryngoscopy, chest tube placement, thoracentesis, bronchoscopy, vein stripping, pacemaker insertion, gastrointestinal endoscopy, excision of skin lesions, and the like). In contrast, 37 general and surgical complications were observed after major abdominal surgery in 34 cirrhotics in the study of Jakab et al. [12]. This high rate of complications may be related to the high proportion of patients with Child class B and C (65%) and the surgical severity of the operations performed.
In our series of patients with cirrhosis, duration of operation, prolonged hospitalization, anemia, and Child-Pugh score were significantly associated with wound-related complications, whereas duration of operation was identified in the univariate analysis as being associated with the occurrence of general complications. In agreement with other studies [8, 9, 12], 20% of patients developed some decompensation of liver cirrhosis that was not present prior to operation. Univariate analysis identified transfusion requirement, decreased platelet count, prothrombin time, and high Child-Pugh score as being associated with decompensation of liver disease, whereas multivariate analysis identified high Child-Pugh score, and number of units of blood transfused as independent risk factors for the occurrence of cirrhosis-related complications.
The present findings confirm that nonhepatic procedures in patients with cirrhosis are associated with a significant death rate, i.e., 16.3% as compared with 3.5% in controls. This difference was found only for patients with Child-Pugh score B and C (31.7% and 54.5%, respectively) given that mortality rates in patients with class A and controls were similar. Differences in the mortality rate between cirrhotics and noncirrhotics have been also reported by other authors, such as 25% versus 1.1% for cholecystectomy and common bile duct exploration in the study of Aranha et al. [14], or 8.3% versus 1.8% for umbilical herniorrhaphy in the study of Leonetti et al. [16]. In our group of 135 patients with cirrhosis, the perioperative mortality rate (within 30 days of surgery) was 16.3%, which is similar to results obtained in other studies, with mortality rates ranging between 11.6% and 28% [7, 8, 9, 12, 13]. Multivariate analysis identified high Child-Pugh score, duration of operation, and general complications as being independently associated with mortality within 30 days after surgery. Child-Pugh score has been found prognostically helpful in all series except the study reported by Rice et al. [8]. These authors, however, showed a statistically significant association between mortality risk and encephalopathy, hyperbilirubinemia, international normalization ratio > 1.6, and hypoalbuminemia, four of the five variables considered by the Child-Pugh scoring system. In addition, the effect of general complications on the outcome of patients with cirrhosis has been indirectly noted in other studies, in which COPD, congestive heart failure, and infection were significantly associated with an increased mortality rate [8, 9].
In summary, patients with cirrhosis and noncirrhotics showed similar rates of wound complications and general complications after nonhepatic surgery, but 20% of cirrhotics developed decompensation of cirrhosis postoperatively. Patients with cirrhosis had a significantly higher mortality rate than controls, but mortality in patients with Child-Pugh class A and controls was similar. Multivariate analysis identified preoperative Child-Pugh score, duration of operation, and general complications as being independently associated with mortality within 30 days after surgery.
Résumé.
La cirrhose du foie apparaît comme un pronostic défavorable pour la chirurgie. Le but de cette étude a été de déterminer les facteurs de morbidité et de mortalité chez les patients cirrhotiques ayant eu une chirurgie non hépatique. Nous avons étudié 135 patients porteurs de cirrhose du foie, opérés d’un procédé non hépatique et 86 patients contrôles, appariés pour l’âge, le sexe, et le diagnostic préopératoire. Les variables pré-, per- et postopératoires en rapport avec la morbidité et al., mortalité à 30 jours ont été étudiés par analyze uni- et multi-variée. Les patients ayant une cirrhose ont eu besoin de plus de transfusions sanguines, ont eu une durée de séjour plus longue, et ont eu un nombre plus élevé de complications que ceux dans le groupe contrôle. Le taux de mortalité a été de 16.3% chez les patients cirrhotiques et de 3.5% dans le groupe de contrôle. Par une analyze univariée, on a trouvé que le besoin en transfusions, un taux de prothrombine, et le score de Child-Pugh étaient significativement associés à la décompensation hépatique postopératoire, alors que la durée de l’acte chirurgical, le temps de prothrombine, le score de Child-Pugh, les complications en rapport avec la cirrhose ont été statistiquement significativement associés à la mortalité. En analyze multivariée, le score de Child-Pugh (rapport de côte (RC): 24.4, interval de confiance de 95% [IC] 5.5 à 106); la durée de chirurgie (RC 5, 95% IC 1.2 à 15.6) et les complications postopératoires générales (RC 3.7, IC 95% 3.4 à 6.4) étaient des facteurs prédicteurs indépendants de mortalité. Les patients cirrhotiques opérés pour autre chose que leur foie ont un risque important de complications périopératoires, pouvant être mortelles Les variables indépendantes associées à une mortalité élevée sont le score préopératoire de Child-Pugh, la durée de chirurgie et la présence de complications générales postopératoires.
Resumen.
La cirrosis hepática constituye un factor pronóstico desfavorable en el paciente quirúrgico. El objetivo del presente estudio fue determinar los factores de riesgo de morbilidad y mortalidad en pacientes con cirrosis sometidos a cirugía no hepática. La población de estudio estaba formada por 135 pacientes con cirrosis hepática en los que se efectuaron diferentes procedimientos quirúrgicos no hepáticos y 86 controles emparejados por edad, sexo y diagnóstico preoperatorio. Las variables preoperatorias, peroperatorias y postoperatorias asociadas con la morbilidad y mortalidad a los 30 días se evaluaron mediante análisis univariado y multivariado. Los pacientes con cirrosis mostraron mayores requerimientos transfusionales y duración de la estancia hospitalaria, así como un mayor número de complicaciones que los controles. La tasa de mortalidad fue del 16.3% en los cirróticos y del 3.5% en los controles. En el análisis univariado, los requerimientos transfusionales, tiempo de protrombina y el grado de Child-Pugh presentaron una asociación estadísticamente significativa con la descompensación hepática postoperatoria, mientras que la duración del acto quirúrgico, el tiempo de protrombina, el grado de Child-Pugh, las complicaciones relacionadas con la cirrosis y las complicaciones generales se asociaron signìficativamente con la mortalidad. En el análisis multivariado, el grado de Child-Pugh (odds ratio [OR] 24.4, intervalo de confianza (IC) del 95% 5.5 a 106); duración de la cirugía (OR 5, IC 95% 1.2 a 15.6) y las complicaciones generales postoperatorias (OR 3.7, IC 95% 3.4 a 6.4) fueron predictores independientes de mortalidad. Los pacientes con cirrosis sometidos a operaciones no hepáticas presentan un riesgo significativo de complicaciones perioperatorias que pueden conducir a un fatal desenlace. Las variables independientes asociadas con la mortalidad perioperatoria incluyen el grado de Child-Pugh, la duración de la cirugía y la presencia de complicaciones generales durante el postoperatorio.
References
SI Schwartz (1981) ArticleTitleBiliary tract surgery and cirrhosis: a critical combination Surgery 90 577–583
RC Doberneck WA Sterling SuffixJr DC Allison (1983) ArticleTitleMorbidity and mortality after operation in nonbleeding cirrhotic patients Am. J. Surg. 146 306–309 Occurrence Handle1:STN:280:BiyA3cnjtVQ%3D Occurrence Handle6604465
RN Garrison HM Cryer DA Howard et al. (1984) ArticleTitleClarification of risk factors for abdominal operations in patients with hepatic cirrhosis Ann. Surg. 199 648–655 Occurrence Handle1:STN:280:BiuB3s%2FisVA%3D Occurrence Handle6732310
GV Aranha HB Greenlee (1986) ArticleTitleIntra-abdominal surgery in patients with advanced cirrhosis Arch. Surg. 121 275–277 Occurrence Handle1:STN:280:BimC38bosF0%3D Occurrence Handle3947226
NF Fernandes WH Schwesinger SG Hilsenbeck et al. (2000) ArticleTitleLaparoscopic cholecystectomy and cirrhosis: a case-control study of outcomes Liver Transpl. 6 340–344 Occurrence Handle1:STN:280:DC%2BD3c3oslyqtQ%3D%3D Occurrence Handle10827236
SB Lausten TM Ibrahim T El-Sefi et al. (1999) ArticleTitleSystemic and cell-mediated immune response after laparoscopic and open cholecystectomy in patients with chronic liver disease. A randomized, prospective study Dig. Surg. 16 471–477 Occurrence Handle10.1159/000018772 Occurrence Handle1:STN:280:DC%2BD3c3mtlaqtA%3D%3D Occurrence Handle10805546
A Mansour W Watson V Shayani et al. (1997) ArticleTitleAbdominal operations in patients with cirrhosis: still a major surgical challenge Surgery 122 730–736 Occurrence Handle1:STN:280:DyaK1c%2FgslGguw%3D%3D Occurrence Handle9347849
HE Rice GE O’Keefe WS Helton et al. (1997) ArticleTitleMorbid prognostic features in patients with chronic liver failure undergoing nonhepatic surgery Arch. Surg. 132 880–884 Occurrence Handle1:STN:280:ByiH3M3mt1U%3D Occurrence Handle9267273
A Ziser DJ Plevak RH Wiesner et al. (1999) ArticleTitleMorbidity and mortality in cirrhotic patients undergoing anesthesia and surgery Anesthesiology 90 42–53 Occurrence Handle1:STN:280:DyaK1M7ht1GitQ%3D%3D Occurrence Handle9915311
RN Pugh IM Murray-Lyon JL Dawson et al. (1973) ArticleTitleTransection of the oesophagus for bleeding oesophageal varices Br. J. Surg. 60 646–649 Occurrence Handle1:STN:280:CSyB3svhvFU%3D Occurrence Handle4541913
ME Charlson P Pompei KL Ales et al. (1987) ArticleTitleA new method of classifying prognostic comorbidity in longitudinal studies: development and validation J. Chronic Dis. 40 373–383 Occurrence Handle1:STN:280:BiiC28nlsVc%3D Occurrence Handle3558716
F Jakab Z Rath I Sugar et al. (1993) ArticleTitleComplications following major abdominal surgery in cirrhotic patients Hepatogastroenterology 40 176–179 Occurrence Handle1:STN:280:ByyB1crmtVA%3D Occurrence Handle8509051
J Carbo J Garcia-Samaniego G Castellano et al. (1998) ArticleTitleLiver cirrhosis and mortality by abdominal surgery. A study of risk factors Rev. Esp. Enferm. Dig. 90 105–112 Occurrence Handle1:STN:280:DyaK1c3ivFSmtg%3D%3D Occurrence Handle9580437
GV Aranha SJ Sontag HB Greenlee (1982) ArticleTitleCholecystectomy in cirrhotic patients: a formidable operation Am. J. Surg. 143 55–60 Occurrence Handle1:STN:280:Bi2D1cbgtlw%3D Occurrence Handle7053656
T Lehnert C Herfarth (1993) ArticleTitlePeptic ulcer surgery in patients with liver cirrhosis Ann. Surg. 217 338–346 Occurrence Handle1:STN:280:ByyB387isFE%3D Occurrence Handle8466308
JP Leonetti GV Aranha WA Wilkinson et al. (1984) ArticleTitleUmbilical herniorrhaphy in cirrhotic patients Arch. Surg. 119 442–445 Occurrence Handle1:STN:280:BiuC2MzivF0%3D Occurrence Handle6703901
JD Klemperer W Ko KH Krieger et al. (1998) ArticleTitleCardiac operations in patients with cirrhosis Ann. Thorac. Surg. 65 85–87 Occurrence Handle10.1016/S0003-4975(97)00931-4 Occurrence Handle1:STN:280:DyaK1c7hsFKgtw%3D%3D Occurrence Handle9456100
YY Jan MF Chen (1997) ArticleTitleLaparoscopic cholecystectomy in cirrhotic patients Hepatogastroenterology 44 1584–1587 Occurrence Handle1:STN:280:DyaK1c%2FovVCltA%3D%3D Occurrence Handle9427027
MA Yerdel C Koksoy N Aras et al. (1997) ArticleTitleLaparoscopic versus open cholecystectomy in cirrhotic patients: a prospective study Surg. Laparosc. Endosc. 7 483–486 Occurrence Handle10.1097/00019509-199712000-00011 Occurrence Handle1:STN:280:DyaK1c%2FpvFCksg%3D%3D Occurrence Handle9438632
H Saeki D Korenaga H Yamaga et al. (1997) ArticleTitleA comparison of open and laparoscopic cholecystectomy for patients with cirrhosis Surg. Today 27 411–413 Occurrence Handle1:STN:280:ByiB2snlvV0%3D Occurrence Handle9130342
JL Poggio CM Rowland GJ Gores et al. (2000) ArticleTitleA comparison of laparoscopic and open cholecystectomy in patients with compensated cirrhosis and symptomatic gallstone disease Surgery 127 405–411 Occurrence Handle10.1067/msy.2000.104114 Occurrence Handle1:STN:280:DC%2BD3c3jvVOgsw%3D%3D Occurrence Handle10776431
Acknowledgments.
We thank Marta Pulido, M.D., for reading the manuscript and providing editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
del Olmo, J., Flor-Lorente, B., Flor-Civera, B. et al. Risk Factors for Nonhepatic Surgery in Patients with Cirrhosis. World J. Surg. 27, 647–652 (2003). https://doi.org/10.1007/s00268-003-6794-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-6794-1