Abstract
Background
The normal morphological and functional values of orbits vary according to race, sex, and age. We measured the palpebral fissure using the marginal reflex distance (MRD1), marginal limbal distance (MLD), and vertical height of the palpebral fissure (VHPF). Unfortunately, these measurements are all one-dimensional figures that measure the distance between two points; they have limitations when it comes to measuring the three-dimensional ocular surface. Therefore, this study used the area of corneal exposure (ACE), which shows a two-dimensional area, to measure changes between the sizes of eyes according to age.
Materials and Methods
This study was conducted using preoperative photographs of Koreans in Daegu city, Korea, who underwent plastic surgery in our department except for eyelid surgery. We divided the subjects into eight groups, including ten males and ten females in each decade of age, from age 10 to over 80 years. A total of 160 people were recruited who were followed up for photograph analysis using Adobe Photoshop 7.0 software.
Results
In terms of the mean value, the ACEs were 73.3 ± 2% in male subjects and 77.1 ± 2% in female subjects, and values for female subjects were greater than those for male subjects (p < 0.05). Significant differences in ACEs were observed according to age. The peak level of growth in the ACE was reached between 20 and 29 years of age. After the 20 s, a gradual decrease was observed (p < 0.05).
Conclusion
The peak level of growth in the ACE was reached between 20 and 29 years of age. The growth pattern can be classified as continuously decreasing after reaching the peak level. The data from this study are significant in that they can be used as comprehensive data for normal eyelid values according to age.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eyelids show significant differences in morphology and structure according to age and race [1]. Many studies on the anthropometry of African-Americans’ eyelids and articles concerned with measurements for only a specific age group have been reported [2, 3]. However, there are few reports on Asian upper eyelids; in particular, to date, there have been no data published in the literature regarding upper eyelid dimensions in this population. Knowledge of the normal data on upper eyelids is critical for surgeons, as this will allow complications to be avoided and ideal outcomes to be achieved [4]. Moreover, understanding of changes that occur in the location and size of the eyelid and eyebrow will be helpful in cosmetic surgery evaluation [1]. We measured the palpebral fissure in the upper eyelid using the marginal reflex distance (MRD1), marginal limbal distance (MLD), and vertical height of the palpebral fissure (VHPF) [5,6,7]. However, these measurements are all one-dimensional figures that measure the distance between two points; they have limitations when it comes to measuring three-dimensional ocular surfaces. In this study, we introduce the area of corneal exposure area (ACE), which shows a two-dimensional area, for measurement of changes between the sizes of eyes according to age in Koreans.
Materials and Methods
Study Patients
In 2012–2016, a total of 160 patients visited the outpatient department (OPD) in our hospital. During the physical examination, any patients who had undergone corrective surgery because of eyelid abnormalities, including ectropion of the eyelid, or blepharoplasty or ptosis correction were excluded from the current analysis. This study was conducted using preoperative photographs of Koreans in Daegu city, Korea, who underwent surgery other than eyelid surgery in our department. We divided subjects into eight groups according to age, from the 10 to the 80 s, and conducted random sampling of 10 males and 10 females in each group [8]. The mean age of the patients was 46.4 years, and 80 male and 80 female subjects were included.
Anthropometry and Photograph Analysis
For measurements, we instructed each patient to look at the optotype 20/200 of the visual acuity test chart hanging 6 m in front of him or her [5]. For accurate measurements, we took measurements three times at intervals of 3 min and recorded the mean values [4]. A 105-mm camera was used to take a picture from a distance of approximately 1 m away so that both eyes were clearly visible in the picture. We measured the ACE via qualitative analysis using software (Adobe Photoshop 7.0, USA) and a Java-based image processing program (Image J 1.40; National Institutes of Health, Maryland Bethesda, USA). Using the measuring software, two examiners (K.J.B. and C.Y.S.) independently performed ACE measurements. First, the area of the visual iris–pupil and total eyeball area was measured using Adobe Photoshop. Second, the area for quantification was measured using Image J, and the percentage was calculated (Fig. 1).
Preoperative frontal views were taken in all patients using a Nikon D80 digital camera (Nikon Corporation, Tokyo, Japan) with a standardized lens. To acquire the photographs, patients sat 1.0 m away from the camera—representing the standard focal length—with their eyes gazing forward. The preoperative images were measured using the qualitatively analyzed software Adobe Photoshop 7.0.1 (Adobe Inc., San Jose, CA) and Java-based image processing software (Image J 1.40; National Institutes of Health, Maryland Bethesda, USA). With the digital photographs opened in Adobe Photoshop, the visualized corneal area was outlined on one eye, and the total corneal area was outlined on the same eye (Fig. 1). The corneal areas were measured. The same technique was repeated for the opposite eye to obtain an average. The ACE was quantified using Image J (Figs. 2, 3). The measured numerical value is used to calculate the percentage with the following formula (Fig. 4):
Statistical Analysis
The SPSS program and one-way analysis of variance (ANOVA), the paired-samples t test, and the independent-samples t test were used for analysis. The statistical significance level was set at p < 0.05 in relation to the control group.
Results
The average ACE for each gender is listed along with the age groups in Table 1. The ACEs were 75.77 and 79.04% for males and females, respectively, in the 20- to 30-year-old group and decreased to 59.09 and 63.29% in males and females, respectively, in the 80- to 88-year-old group (Table 1). The ACE showed significant differences according to age (p < 0.05; Table 2). In terms of the mean value, the ACE was 69.93 ± 2.39% in all patients (Table 2). Table 2 describes changes between age groups, and the biggest decrease was observed between the 50- to 59-year-old group and 60- and 69-year-old group (p < 0.05).
Values for female subjects were greater than those for male subjects, at 77.1 ± 2% for female subjects and 73.3 ± 2% for male subjects. There was a significant difference according to sex (p < 0.05; Fig. 5).
Figure 6 presents the average numerical ACE value with age. The graph shows the mean ACE value ± the standard error of the mean (SEM) analyzed at each decade as a point. The peak level of growth in the ACE was reached at age 20–29 years. After the 20 s, it showed a gradual decrease (Fig. 6). The correlation between age and ACE value was explained by the following formula: ACE = − 0.1095 × age + 8.962. This gradual linear decrease in the ACE value proves that the ACE decreases according to age. The growth pattern can be classified as continuously decreasing and stationary after the age of 30 years. Figures 7 and 8 illustrate clinical application of ACE in age and sex difference.
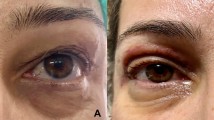
Clinical application for sexual difference. Measurement of ACE according to sex. A 19-year-old female (left) and a 19-year-old male (right) were measured for ACE. The value for the 19-year-old female was 90% on the left side and 89% on the right side; the value for the 19-year-old male was 51% on the left side and 52% on the right side. The value for females was larger than that for males at the same age
Clinical application for age difference. Measurement of ACE according to age. A 19-year-old female (left) and an 80-year-old female (right) were measured for ACE. The value for the 19-year-old female was 90% on the left side and 89% on the right side; the value for the 80-year-old was 51% on the left side and 52% on the right side. The value for younger females was larger than that for older females
Discussion
The ACE was analyzed and documented in different age groups by decade among male and female Korean patients. The ACE was defined as the percentage of visualized corneal area divided by total corneal area. The measurements were compared over the eight different age groups to analyze how much the ACE decreases according to age. A simple measurement using accessible photographic software is important to determine operative outcomes and to obtain average values for each age group. Digital photography of measuring the area of corneal exposure will provide surgeons with a guideline for preoperative blepharoplasty planning.
With greater frequency of plastic surgery, a plastic surgeon constantly strives to reduce complications and improve outcome satisfaction. Accurate measurement is necessary to accomplish this. The palpebral fissure is a common parameter to be measured during the performance of upper blepharoplasty [11]. The palpebral fissure shows significant differences in morphology and structure according to age and race, and it has a significant effect on appearance. Therefore, many individuals have undergone measurement of the palpebral fissure on the upper eyelid using the MRD1, MLD, and VPH [6, 7]. However, measurement using a paper ruler can be highly inaccurate, especially when the measurement is taken by inexperienced clinicians [8].
Multiple techniques for eyelid measurement have been evaluated in an attempt to carry out more objective assessment of the eyelid. Lee [8] sought to analyze the upper eyelid contour using a software program that measures multiple radial midpupil lid distances. Moreover, Rayisa reported that three-dimensional cameras can help in better assessing the spherical area of the globe [9]. However, these methods either require a learning curve or expensive equipment. In our study, we used a simple approach to measure the percentage of the ACE, which represents a two-dimensional area, using a digital photographic technique. This appears to be a substantially more convenient and accurate method of eyelid measurement.
In our study, we obtained the following results: In terms of the mean value, the ACE was 75.4 ± 2% in all patients. Female subjects exhibited greater values than male subjects. The peak level of growth in the ACE was reached at the age of 20–29 years in males and females. After this decade, it showed a gradual decrease. The ACE showed significant differences according to age.
Our study showed contradictory results to those of prior research on eyelid measurement with age. Van den Bosch et al. [10] reported no decrease or statistical significance with age for MRD1. Hong and Hee [12] showed a slight decrease with age, but this did not reach statistical significance. Our findings indicated a slow, almost linear decrease in the ACE, and there were statistically significant differences with age. Thus, we found that age is a major factor in decreasing ACE. Because globe size does not change in adulthood [13], the main reason for the decreasing size with age must have to do with the eyelid. Lateral brow descent and sub-brow soft tissue redundancy are fundamental factors in making the eye smaller. Moreover, an increasing amount of lower lid laxity with age makes the lower eyelid cover more of scleral show, which is a factor in decreased eye size. Moreover, the loss of upper sulcus fat weakens the levator palpebrae, which leads to ptosis [14]. In addition, orbital volume expands with age because of bone resorption, most markedly in the superomedial and inferolateral regions, thereby leading to enophthalmos [15]. We think that lower lid laxity, ptosis, and enophthalmos contribute to the smaller eye size with age, and these facts are consistent with the ACE decreasing according to age, as illustrated in this study.
We found a gradual and almost linear decrease in the ACE by decade. The greatest decrease was observed between the ages of 50–59 and 60–69 years. This is consistent with the appearance of more advanced age in the eyelid’s appearance in the 60- to 69-year-old group; moreover, it supports the American Society for Aesthetic Plastic Surgery’s (ASAPS’s) 2015 cosmetic surgery statistics, which showed that most blepharoplasty operations were performed in individuals aged 51–64 years. This finding offers numerical values to understand the aging process better.
In Jung and Hong’s study, mean VHPF values of 8.2 and 8.5 mm were found for Korean adult males and females, respectively [16]. Moreover, Baek et al. [17] reported results of 7.6 mm in adult males and 7.8 mm in adult females, which was not statistically significantly different. Cho et al. [18] reported values of 8.0 and 8.2 mm in males and females. These studies showed there is no significant difference according to sex for VHPF. Although contradictory reports have emerged concerning statistical differences in the VHPF between male and female subjects, our study revealed that the mean ACE values were greater than in females, and the difference was statistically significant (p < 0.05).
Our method had some limitations. First, although it is generally acknowledged that not all patients have perfectly round pupils, it would appear that the most common shape of the human pupil is a slightly vertical oval [19]. Second, the patient number per age group was relatively small. More patients could be recruited to demonstrate the numerical average ACE value per age group. Also, the groups seem to be somewhat irrational to represent a true example of the population as they are based on patients who came to the clinic. Third, the ACE calculation method did not take into consideration the nature of the curve of the cornea. Assessment of this factor could be more complicated and hard to measure. This makes the ACE value less precise. In addition, serial “forward gaze” photographs of a patient will surely vary slightly in angulation between the subject and camera, and this can affect the measured area of the cornea visible on the photographs.
Conclusion
We introduced the ACE, which is a two-dimensional area, for measurement of the change between the sizes of eyes according to age in Koreans. The peak level of growth in the ACE was reached at the age of 20–29 years. The growth pattern can be classified as continuously decreasing and stationary after reaching the peak level. In this study, our data have significant applicability for use as comprehensive data on normal eyelid values according to age, and they can provide objective measurement for clinical applications.
References
Park DH, Choi WS, Yoon SH et al (2008) Anthropometry of Asian eyelids by age. Plast Reconstr Surg 121:1405–1413
Farkas LG, Forrest CR, Litsas L (2000) Revision of neoclassical facial canons in young adult Afro-Americans. Aesthet Plast Surg 24:179–184
Barretto RL, Mathog RH (1999) Orbital measurement in black and white populations. Laryngoscope 109:1051–1054
Price KM (2009) Eyebrow and eyelid dimensions: an anthropometric analysis of African Americans and Caucasians. Plast Reconstr Surg 124:615–623
Baek SW (2000) Anthropometric analysis of palpebral fissure. J Korean Soc Aesthet Plast Surg 1:221
Morris CL, Morris WR, Fleming JC (2011) A histological analysis of the Mullerectomy: redefining its mechanism in ptosis repair. Plast Reconstr Surg 127:2333–2341
Park DH, Jung JM, Song CH (2008) Anthropometric analysis of levator muscle function. Plast Reconstr Surg 121:1181–1187
Lee H, Lee JS, Chang MW et al (2014) Analysis of lid contour change with aging in Asians by measuring midpupil lid distance. Plast Reconstr Surg 134:521e–529e
Hontscharuk R, Fialkov JA, Binhammer PA et al (2012) Primary orbital fracture repair: development and validation of tools for morphologic and functional analysis. J Craniofac Surg 23:1044–1049
van den Bosch WA, Leenders I, Mulder P (1999) Topographic anatomy of the eyelids, and the effects of sex and age. Br J Ophthalmol 83:347–352
Tsai PY (2012) Ocular surface area changes after double eyelidplasty. J Plast Reconstr Aesthet Surg 65:141e–145e
Hong RS, Hee BA (2009) Morphological changes of the eyelid according to age. J Korean Ophthalmol Soc 50:1461–1467
Duke-Elder S, Wybar KC (1961) The anatomy of the visual system. In: Duke-Elder S (ed) System of ophthalmology, vol II. Mosby, St. Louis
Lambros V (2007) Observations on periorbital and midface aging. Plast Reconstr Surg 120:1367–1376
Kahn DM, Shaw RB (2008) Aging of the bony orbit. A three-dimensional computed tomographic study. Aesthet Surg J 28:258–264
Jung TM, Hong SK (1974) The exophthalmometry, extraorbital width and height of lid fissure of Koreans. J Korean Ophthalmol Soc 15:4
Baek SW, Kim JH, Park SH et al (1995) Anthropometric analysis of palpebral fissure. J Korean Soc Aesthet Plast Surg 1:221
Cho JH, Han KH, Kang JS (1993) Normal anthropometric values and standardized templates of Korean face and head. Korean Soc Aesthet Plast Surg 20:995–1005
Arshad M, Khanani MD, Steven M et al (2004) Horizontal versus vertical dark-adapted pupil diameters in normal individuals. J Cataract Refract Surg 30:2557–2558
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, K., Guo, Z. & Park, D.H. Measurement of the Area of Corneal Exposure Using Digital Image and Its Application During Assessment for Blepharoplasty. Aesth Plast Surg 42, 208–214 (2018). https://doi.org/10.1007/s00266-017-0980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-017-0980-2