Abstract
Background
Gynecomastia is a benign, excessive development of the male breast that occurs at an overall incidence of 32–36 %. The authors effectively removed peripheral fat tissues with power-assisted liposuction (PAL) and periareolar glandular tissues with a cartilage shaver in a series of patients. The small periareolar incisions were not easily recognized.
Methods
Between February 2010 and April 2012, the charts of 15 patients (28 breasts) treated with PAL and a cartilage shaver were retrospectively reviewed.
Results
The mean volume of fat tissue removed with liposuction was 319 mL, and the mean volume of glandular tissue removed with the cartilage shaver was 70 mL. The mean follow-up period was 11.2 months. No infection, nipple–areola complex necrosis, nipple retraction, or saucer deformity was encountered in this series. Intraoperative bleeding occurred in one patient. Mild asymmetries developed in three patients.
Conclusions
Use of PAL and a cartilage shaver for the treatment of gynecomastia allows for effective removal of both the fat and the glandular tissue of the breast through a minimal periareolar incision. This technique can achieve excellent aesthetic results with inconspicuous scarring.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gynecomastia is a benign, excessive development of the male breast caused by proliferation of the ductular element and adipose tissue [1]. The overall incidence of gynecomastia is 32–36 % [2, 3], and 65 % of cases involve adolescent boys [4].
In the International Society of Aesthetic and Plastic Surgery international survey on aesthetic and cosmetic procedures performed in 2010, correction of gynecomastia ranked as the 10th most commonly performed surgical procedure by plastic surgeons worldwide [5].
There are three types of gynecomastia: glandular, fatty glandular, and fatty [6, 7]. The glandular and fatty glandular types are frequently observed, especially in puberty [4]. In longstanding gynecomastia, fibrosis, and hyalinization of loose periductal tissue occur, causing a glandular hypertrophy that does not regress [8]. Therefore, surgical resection of the periareolar glandular tissue is essential in the treatment of these cases.
Many patients with gynecomastia tend to feel shame because of the feminine breast shape. This leads to a posture characterized by shrinking of the back and shoulders in efforts to disguise the prominent breast. As a result, these patients usually have lower self-esteem.
Most cases of gynecomastia do not influence the lifespan of the affected patients, so treatment most strongly affects quality of life and self-confidence. With treatment, it is very important not only to restore the breast contour but also to leave minimal scars.
The authors effectively removed peripheral fat tissues with power-assisted liposuction (PAL) and periareolar glandular tissues with a cartilage shaver. The small periareolar incisions were not easily recognized. This study aimed to introduce a surgical correction of gynecomastia with minimal scarring and the outcome of this technique.
Materials and Methods
Between February 2010 and April 2012, the charts of 15 patients (28 breasts) for whom we used the PAL and the cartilage shaver were retrospectively reviewed. The study was approved by our Institutional Review Board. The patients ranged in age from 13 to 55 years (average, 21.5 years). The duration of gynecomastia was 1.5–10 years (average, 4.9 years). Patients with gynecomastia sustained less than 1 year who could experience spontaneous regression were not treated.
We examined the preoperative hormonal status, including the levels of luteinizing hormone (LH)/follicle-stimulating hormone (FSH), testosterone, estradiol, and human chorionic gonadotropin (HCG), for every patient. One of our patients took a selective estrogen receptor modulator (Tamoxifen; Kwang Dong Pharmaceutical Co., Seoul, Korea). This patient’s breast fat tissues were reduced during administration of the drug, but no glandular tissues showed signs of reduction.
The authors checked every patient for chest wall deformities during the preoperative physical examinations. Mammographies also were performed. The extent of periareolar glandular tissues and their distributions were analyzed with manual palpation and mammographies. The breast fat tissues were removed by PAL (Lipomatic 3; Euromi S.A., Verviers, Belgium) using 4-mm Mercedes cannulas. The periareolar glandular tissues then were removed with cartilage shavers (Linvatec Corporation, Largo, FL, USA).
The cartilage shaver is a powered, rotary shaving device with continuous suction. The blades of this device comprise two concentric cannulas (Fig. 1). The outer cannula has an opening with a sharp margin, and the inner cannula rotates in oscillation mode (see Video, Supplemental Digital Content 1, which demonstrates the shaving for removal of periareolar glandular tissues).
Surgical Technique
The areas of fat and glandular tissue and a concentric topographic map were marked preoperatively with the patient in a standing position. All the patients were administered a general anesthesia. Each patient was placed in the supine position with the arms abducted at 90°. A 6-mm incision for the insertion of protectors with a diameter of 5 mm was made at the inferior areolar margin (Fig. 2). The incision was made just on the outer edge of the areolar pigmentation.
Before liposuction, a tumescent solution containing 1 L of 0.9 % NaCl, 1 mL of 1:1,000 epinephrine, and 20 mL of 2 % lidocaine was infiltrated into the enlarged breast tissue. Protectors to prevent skin injury due to vibrations of the liposuction device were inserted through the inferior periareolar incision. The PAL was always performed first and proceeded along the mappings drawn preoperatively, with consideration for the natural convexity of the breasts.
After the liposuction, cartilage shavers were selectively applied to remove the remaining glandular tissues around the periareolar areas (Fig. 3). The glandular tissue was severed and suctioned by the cartilage shaver at low speed (1,500 rpm). Regularity of the breast was checked with the roll test. Symmetry also was checked. No breast skin excisions were performed.
After periareolar glandular tissue had been shaved, cold saline irrigation and fibrin sealant (Tisseel; Baxter International Inc., Deerfield, IL, USA) were applied to prevent bleeding. Hemovac drains (100 mL) were inserted through an infraareolar incision in the breasts and removed on postoperative day 1 or 2. Compressive dressings also were applied postoperatively.
We recommended that the patients reduce their activities for at least 1 week postoperatively. The stitches were removed on postoperative day 7. The patients wore compression garments for the following 4 weeks.
Results
No hormonal imbalances or abnormalities were shown in the preoperative examinations. Two patients had minor chest wall deformities, and both deformities were left-side prominent. Therefore, the correction of gynecomastia was limited. The risk of residual breast asymmetry because of preoperative chest wall deformities was explained to every patient.
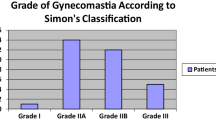
The mean volume of fat tissue removed with liposuction was 319 mL (range, 50–720 mL), and the mean volume of glandular tissue removed with the cartilage shaver was 70 mL (range, 20–130 mL). The mean follow-up period was 11.2 months. The numbers of Rohrich grades [9] 1A, 1B, 2A, and 2B patients were 3, 5, 6, and 1, respectively. Every patient was satisfied with the result (Figs. 4, 5, 6). The scars on the inferior areolar margin were barely recognizable (Fig. 7).
No infection, nipple–areola complex necrosis, nipple retraction, or saucer deformity was encountered in this series. Intraoperative bleeding occurred in one patient. Mild asymmetries developed in three patients. One patient with a chest wall deformity had mild remaining asymmetry. However, no patients in this study underwent reoperation.
Discussion
Many surgical trials have been performed to correct gynecomastia [6, 7, 9–16]. Subcutaneous mastectomy results in the longest scar [10]. With this procedure, two parallel incisions are made from the lateral margin on the pectoralis major to the medial end of the inframammary crease [10]. This method is a very good option for correcting gynecomastia when skin redundancy is present, but it is not applicable to patients with minimal to moderate gynecomastia.
Many surgical procedures have been performed in an attempt to remove the periareolar glandular tissues effectively with minimal scarring [11, 12]. However, semicircular areolar incisions or circumareolar incisions leave longer scars than the current surgical techniques.
Recently, suction-assisted lipectomy and ultrasound-assisted liposuction have been used for primary treatment of gynecomastia [9]. These procedures can be performed with small incisions no larger than the cannula. However, they have limitations in terms of removing the periareolar glandular tissues [9, 13].
Several studies have explored new surgical options that involve the use of a cartilage shaver either alone or with liposuction [13–16]. However, Prado and Castillo [14], Benito-Ruiz et al. [13], and Song et al. [15] left additional scars in the inframammary folds. In addition, Goh et al. [16] left scars on the anterior axillary lines. These procedures showed excellent aesthetic results, but the additional scars were easily recognizable in the figures of the articles.
In the current study, minimization of scarring was intended, with small incisions on the areolar margins. An obvious bleeding risk was associated solely with application of the cartilage shaver because of its tendency to make sharp dissections. Therefore, we selectively used only the residual periareolar glandular tissues after PAL.
One of our patients had bleeding at the pocket in the breast after shaving. We irrigated this area with copious amounts of cold saline, but the bleeding continued. It was controlled after 20 min of compression around the bleeding focus and application of absorbable hemostats (Surgicel; Ethicon Inc., Somerville, MA, USA).
The procedure used in this study removes the breast tissues with only a small incision. Thus, it is very difficult to find the bleeding focus when bleeding occurs. Accordingly, cartilage shavers should be used only on periareolar glandular tissues. They should not be used in areas with large vessels, such as the axilla. We performed many procedures to reduce the risk for the development of bleeding including cold saline irrigations, Hemovac drain insertion, Tisseel application, compressive dressing application, and postoperative ice packing.
Another advantage of using a cartilage shaver with a minimal periareolar incision is the ability to remove glandular tissues in every direction through a simple wrist rotation. Cartilage shavers can remove periareolar glandular tissue without a pull-through or pull-out technique.
Nipple–areolar complex retractions occurred in two cases between postoperative weeks 1 and 2. However, the patients in both cases recovered with only areolar massage. No revision was necessary. Subcutaneous sutures should be placed in every case to prevent retraction or dimpling of the nipple–areolar complex. The superior aesthetic results of our study can be attributed to the conservative approach to removal of the tissues just beneath the nipple.
Conclusion
With the use of PAL and a cartilage shaver in the treatment of gynecomastia, both the fat and glandular tissue of the breast can be effectively removed through a minimal periareolar incision. This technique can achieve excellent aesthetic results with an inconspicuous scar.
References
Mathes SJ, Seyfer AE, Miranda EP (2006) Congenital anomalies of the chest wall. In: Mathes SJ (ed) Plastic surgery, 2nd edn. Saunders Elsevier, Philadelphia, pp 457–537
Carlson HE (1980) Gynecomastia. N Engl J Med 303:795–799
Nuttall FQ (1979) Gynecomastia as a physical finding in normal men. J Clin Endocrinol Metab 48:338–340
Nydick M, Bustos J, Dale JH, Rawson RW (1961) Gynecomastia in adolescent boys. JAMA 178:449–454
International Society of Aesthetic and Plastic Surgery international survey on aesthetic and cosmetic procedures performed in 2010 (2010). http://www.isaps.org/isaps-global-statistics.html. Accessed August 2012
Morselli PG (1996) “Pull-through”: a new technique for breast reduction in gynecomastia. Plast Recontr Surg 97:450–454
Bracaglia R, Fortunato R, Gentileschi S, Seccia A, Farallo E (2004) Our experience with the so-called pull-through technique combined with liposuction for management of gynecomastia. Ann Plast Surg 53:22–26
Karsner HT (1946) Gynecomastia. Am J Pathol 22:235–315
Rohrich RJ, Ha RY, Kenkel JM, Adams WP Jr (2003) Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Recontr Surg 111:909–923
Wray RC Jr, Hoopes JE, Davis GM (1974) Correction of extreme gynaecomastia. Br J Plast Surg 27:39–41
Webster JP (1990) Mastectomy for gynecomastia through a semicircular intraareolar incision. Ann Surg 12:557–575
Huang TT, Hidalgo JE, Lewis SR (1982) A circumareolar approach in surgical management of gynecomastia. Plast Reconstr Surg 69:35–40
Benito-Ruiz J, Raigosa M, Manzano M, Salvador L (2009) Assessment of a suction-assisted cartilage shaver plus liposuction for the treatment of gynecomastia. Aesthet Surg J 29:302–309
Prado AC, Castillo PF (2005) Minimal surgical access to treat gynecomastia with the use of a power-assisted arthroscopic-endoscopic cartilage shaver. Plast Recontr Surg 115:939–942
Song JY, Han BK, Kim CH (2009) The treatment of gynecomastia using XPS microresector (shaver). J Korean Soc Plast Reconstr Surg 36:806–810
Goh T, Tan BK, Song C (2010) Use of the microdebrider for treatment of fibrous gynecomastia. J Plast Reconstr Aesthet Surg 63:506–510
Acknowledgments
The authors thank illustrator Hye-Seong Park. This research was supported by Yeungnam University grants in 2012.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (WMV 4130 kb)
Rights and permissions
About this article
Cite this article
Lee, JH., Kim, IK., Kim, TG. et al. Surgical Correction of Gynecomastia with Minimal Scarring. Aesth Plast Surg 36, 1302–1306 (2012). https://doi.org/10.1007/s00266-012-9970-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-012-9970-6