Abstract
Among the reasons for reoperation after augmentation mammaplasty is the malpositioned implant, especially a lowered inframammary fold or symmastia, which is difficult to repair. The peri-implant capsule, a physiologic response to a foreign body, is naturally formed and suitable for use as a flap because of its high vascularity. In addition, it is sufficiently tough for suspension of the implant. The authors introduce the idea that the capsular flap is very useful for the correction of symmastia or a lowered inframammary fold. In such situations, the capsular flaps are used to prevent migration of the implant after raising of the inframammary fold or defining of the midline with capsulorrhaphy. This technique successfully corrected the malpositioned implants in this study, and all the patients were satisfied. There was no recurrence of a lowered inframammary fold or symmastia. These findings suggest that the capsular flap should be considered a safe and effective option for the management of malpositioned implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast augmentation is a popular cosmetic surgical procedure. The development of surgical methods and breast implants has been associated with reduced risk for complications of breast augmentation. However, a recent cohort study reported the overall risk for reoperation to be 12.5% among augmentation patients [1]. The causes for reoperation were capsular contracture, implant rupture, palpable implant, exposed implant, implant malposition, and infection [1–3].
Although implant malposition is a common cause of reoperation among breast augmentation surgeries, the medical literature has little information about this complication. Methods such as capsulorrhaphy, capsular flaps, AlloDerm (LifeCell Corp, Branchburg, NJ), explantation with delayed reimplantation, and changing of the pocket have been used to correct implant malposition [4–8], but correction, especially for a lowered inframammary fold or symmastia, is difficult to achieve.
We present a novel procedure involving internal pocket plication reinforced with the flap from the capsule physiologically formed around the implant after breast augmentation. This method proved to be safe and effective for the correction of implant malposition in secondary breast augmentation procedures. The capsular flap is thin but strong enough to withstand the weight of the implant and to maintain its original postoperative position for long periods.
Surgical Technique
Preoperatively, the patient is marked in the standing position. The ideal location for the implant and the dissection area is accurately marked, and the area of thin skin of the palpable implant or rippling area is marked if present. General anesthesia is provided.
The areolar “omega” zigzag incision (transareolar-perinipple incision) usually is preferred because of its imperceptible operation scar. However, if the diameter of the areola is less than 2.7 cm, an inframammary incision is used, and if a previous periareolar operation scar exists, the approach is through the previous incision line.
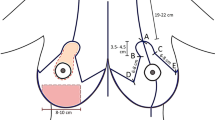
Through the areolar “omega” zigzag incision, the dissection between the breast tissue and subcutaneous fatty layer is performed to the capsule. The anterior capsule is dissected, with the implant kept in place except for the area that will be the base of the capsular flap. The implant then is removed through the incision on the capsule. Incisions for the capsulorrhaphy are made on the anterior capsule along the preoperatively designed line and corresponding opposite posterior capsules. In addition, several scoring incisions are made on the anterior and posterior capsules of the area to be closed, and a counter capsulotomy is performed if needed (Fig. 1a).
Placement of the capsular flap on the capsulorrhaphy area. a The lowered inframammary fold and lower positioned implant. b The lowered inframammary fold is elevated by permanent capsulorrhaphy suture, and the capsular flap is raised. c The capsular flap (gray-colored area) is turned down on the capsulorrhaphy site. 1 (planned capsular flap), 2 (incision on the anterior capsule for capsulorrhaphy), 3 (scoring for adhesion), 4 (countercapsulotomy if needed), 5 (incision on the posterior capsule for capsulorrhaphy), 6 (raised capsular flap), 7 (capsulorrhaphy with nonabsorbable sutures), 8 (capsular flap for reinforcement of capsulorrhaphy), 9 (absorbable sutures for fixation of the flap), 10 (remaining posterior capsule), 11 (remaining anterior capsule)
The capsulorrhaphy is performed with interrupted sutures and continuous double sutures using 2-0 Prolene. The capsular flap from the anterior capsule is turned down to the area of the capsulorrhaphy for reinforcement of the pocket plication and fixed with 4-0 Vicryl sutures in the stretching position. A new implant is inserted into the newly made space after careful hemostasis is achieved, and the wound is closed (Fig. 1b, c).
Case Reports
Case 1
A 27-year-old woman had undergone transumbilical breast augmentation (TUBA) with a 175-ml saline implant 5 years previously. She reported a symmastia-like appearance, asymmetric breasts with an uncomfortable feeling of the implant on the lower medial region of the right breast, and a contracted umbilical scar. There was no capsular contracture, and the implants were palpated at the lower medial quadrant of the right breast. Both implants were located too medially, especially the right implant, which was more medially located (Fig. 2a–d).
Case 1. A 27-year-old woman who reported an undesirable breast shape and palpation of the implant on the right medial portion of her breast. a, b Preoperative view. c Preoperative findings and design. The palpable implant is marked (blue shaded area). The implants are located too medially, especially on the right side. d The woman had symmastia. e, f View 6 months after the revised breast augmentation with capsulorrhaphy and capsular flap in the medial pocket and counter capsulotomy in the lateral pocket
Through an areolar “omega” zigzag incision, the implant was removed. For correction of the implant palpation, the capsular flaps were turned down under the thinned area. To define the medial border of the breast, a medial pocket plication was performed with interrupted and continuous double-layer sutures using 2-0 Prolene after several scorings on the anterior and posterior capsule. Another capsular flap covered the medial capsulorrhaphy area to reinforce the pocket plication. After completion of the capsulotomy on the lateral pocket and more subfascial dissection laterally for widening of the pocket, a 265-ml smooth cohesive silicone gel implant was inserted, and the wound was closed.
The patient was very satisfied with the outcome of the procedure 6 months after the operation. There was no evidence of symmastia recurrence, and the implant could no longer be palpated (Fig. 2e, f).
Case 2
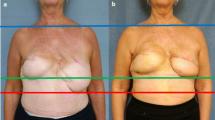
A 36-year-old woman had undergone two prior submuscular breast augmentation procedures via the axillary approach with saline implants 5 years previously. She reported asymmetric breasts and an uncomfortable feeling of the implant. The implants were palpated at the lateral and inferior sides of both breasts, and no capsular contracture was detected. The right inframammary fold was lower than the left one (Fig. 3a–d).
Case 2. A 36-year-old woman who reported asymmetric breasts and unpleasant feeling of the implant. a, b Preoperative view. c, d Preoperative findings and design. The right inframammary fold was lower than the left one. The implants were palpated at the lateral and inferior side of both breasts (red shaded area), and there was no capsular contracture. e, f View 1 week after revised breast augmentation with capsulorrhaphy and capsular flap in the inferior pocket
Through an areolar “omega” zigzag incision, the implant was removed. For correction of the implant palpation, the capsular flaps were turned down under the thinned area on both breasts. To correct the lowered inframammary fold, an inferior pocket plication was performed with interrupted and continuous double-layer sutures using 2-0 Prolene after several scorings on the anterior and posterior capsule. The capsular flap covered the sutured inferior area to reinforce the pocket plication of the right breast. After completion of the subpectoral pocket, 234 ml of smooth cohesive silicone gel was inserted, and the wound was closed.
The right lowered inframammary fold was corrected, and the patient was very satisfied with the outcome of the procedure 1 week after the operation (Fig. 3e, f). The patient reported no evidence of recurrence of right lowered inframammary fold, and the implant could not be palpated any longer 3 months after the operation.
Discussion
Breast augmentation is a common cosmetic surgical procedure. Although breast augmentation surgery generally is successful, some cases require revision. The Mentor core study on silicone breast implants published in 2007 reported an overall reoperation rate of 15.4% among patients with primary breast augmentation. Allergan, Inc., reported a 12.5% reoperation rate [1, 3].
The most common reasons for revision breast surgery are style or size change (4.7%) followed by implant malposition (2.6%) and capsular contracture (1.9%) [1]. Implant malposition is a common reason for patient dissatisfaction with breast augmentation. This complication occurs when the implant is not centered behind the nipple. For a patient with a high-riding implant, a simple open capsulotomy is sufficient to lower the implant. Malposition of the implant in the inferior, lateral, or medial direction can be corrected relatively simply with capsulorrhaphy and mirror-image selective capsulotomy to remove tension from the line of plication of the capsulorrhaphy [4, 7].
Although acellular dermal matrix materials also have been used to treat malposition of implants [8], capsulorrhaphy has remained the mainstay of the repair. However, capsulorrhaphy may have somewhat inconsistent results because the implant may fall against the suture line, moving across it and disrupting the repair. Then the action of the pectoralis major muscle may pull the repair apart in either the submuscular or subglandular positions [6]. Therefore, we reinforced the plicated site with a capsular flap raised from the capsule.
The capsule is thin, highly vascularized, and physiologically formed around the implants used for breast augmentation [9]. The capsule may persist for 17 years after implant removal, although in most cases, the capsule is reabsorbed after the implant is removed [10]. The capsule, comprising multiple layers of collagen fibers and a thin vascular layer near the inner surface [9], can be raised on a small pedicle and used as a flap [11].
We used a capsular flap to create a sling. This resulted in a vascularized reinforced repair that protected the capsulorrhaphy line from the maximum weight of the implants.
An implant is in contact with the raw surface because the capsular flap is folded down on the capsulorrhaphy area. The reinforcing effect of the capsular flap is duplicated by newly formed capsule around the implant. Although the persistence of the capsular flap is questionable because it is controversial for the capsule to be resorbed after implant removal, the capsular flap plays its role with its persistence because it has the conditions to survive with circulation in itself.
Conclusion
A capsular flap on capsulorrhaphy is a powerful technique that is safe and effective for repairing breast implant malposition and improving the results of reoperative breast surgery.
References
Bengtson BP, Van Natta BW, Murphy DK, Slicton A, Maxwell GP (2007) Style 410 highly cohesive silicone breast implant core study results at 3 years. Plast Reconstr Surg 120:40S–48S
Araco A, Gravante G, Araco F, Delogu D, Cervelli V, Walgenbach K (2007) A retrospective analysis of 3,000 primary aesthetic breast augmentations: postoperative complications and associated factors. Aesth Plast Surg 31:532–539
Cunningham B (2007) The mentor core study on silicone MemoryGel breast implants. Plast Reconstr Surg 120:19S–29S
Spear SL, Little JW (1988) Breast capsulorrhaphy. Plast Reconstr Surg 81:274–279
Parsa FD (1990) Breast capsulopexy for capsular ptosis after augmentation mammaplasty. Plast Reconstr Surg 85:809–812
Voice SD, Carlsen LN (2001) Using a capsular flap to correct breast implant malposition. Aesth Surg J 21:441–444
Chasan PE (2005) Breast capsulorrhaphy revisited: a simple technique for complex problems. Plast Reconstr Surg 115:296–301
Baxter RA (2003) Intracapsular allogenic dermal grafts for breast implant-related problems. Plast Reconstr Surg 112:1692–1696
Rubino C, Mazzarello V, Farace F, D’Andrea F, Montella A, Fenu G, Campus GV (2001) Ultrastructural anatomy of contracted capsules around textured implants in augmented breasts. Ann Plast Surg 46:95–102
Rockwell WB, Casey HD, Cheng CA (1998) Breast capsule persistence after breast implant removal. Plast Reconstr Surg 101:1085–1088
Imran D, Javaid M, Lewis D, Attar KH (2005) Capsular flap for correction of contour deformities of the breast. Ann Plast Surg 54:662–663
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoo, G., Lee, PK. Capsular Flaps for the Management of Malpositioned Implants After Augmentation Mammoplasty. Aesth Plast Surg 34, 111–115 (2010). https://doi.org/10.1007/s00266-009-9456-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-009-9456-3