Abstract
Background
Conventional treatment for nasal augmentation utilizes autologous grafts, allografts, or synthetic implants such as silicon implants. Silicon implants could protrude/expose or induce nasal bone resorption. Autologous grafts are usually associated with donor site morbidity and the volume of harvested tissue is limited. We had developed a new method for nasal augmentation using cultured autologous chondrocytes (CAC). The current report presents the results of a study using that method with a larger number of patients and an improved graft technique for the nasal tip.
Methods
Approximately 1 cm2 of cartilage was harvested from the auricular concha and treated with collagenase, and then chondrocytes were obtained. In our multilayer culture system the chondrocytes formed immature cartilaginous tissues with a gelatinous chondroid matrix. They were injection-grafted into the subcutaneous pocket of the nasal dorsum.
Results
The chondrocytes with a gelatinous chondroid matrix change from a soft gel to hard neocartilage tissue within 2 to 3 weeks and then stabilize. The authors have used this procedure over a 6-year period on 75 cases: 58 secondary augmentation rhinoplasties following silicon implantation and 17 primary augmentation cases. The results have been satisfactory and long-lasting.
Conclusion
Grafting of CAC is an optional method for nasal augmentation and could be used for a wide range of facial augmentation cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Augmentation rhinoplasty of the nasal dorsum has been achieved by the grafting of various autologous tissues such as bone, cartilage, and fascia; synthetic materials such as silicone and polymeric materials; and allografts [1–14]. Autologous cartilage is the most commonly used material and the preferred choice in augmentation rhinoplasty. However, the collection of autologous tissues as a graft material is associated with donor site morbidity, and the harvested volume of the tissues is limited. Various studies have been conducted to find solutions for these drawbacks. We developed a new method using biotechnology, in which a portion of a patient’s tissue is harvested, the obtained cells are cultured into a large volume and developed into a tissue block similar to auricular chondrocytes, and the result is grafted into the patient [15–19]. The most significant improvements of our method over existing methods are the minimal morbidity of the donor site and the flexible supply of graft material through the culture of preserved chondrocytes. Our method can always provide a sufficient volume of graft material.
We used these cultured autologous chondrocytes (CAC) for nasal augmentation. The cultured chondrocytes are in a soft gel form because they produce a gelatinous chondroid matrix, and they are highly flexible. Therefore, the chondrocytes can be injection-grafted into a subcutaneous pocket created by dissection. The gel-like tissue turns solid 2 to 3 weeks after grafting and forms a matured cartilage.
We also improved our grafting method for patients who had silicon implantation and whose skin on the nasal tip had become thin and had a concave deformity. Treatment of such patients requires filling of cartilaginous tissues and soft tissues. We invented a combined grafting technique that uses both the CAC and the temporal fascia. We consider that CAC might be a new option for nasal augmentation.
Materials and Methods
The Institutional Review Board of the Ethical Committee of Osaka City General Medical Center approved this study. Each patient received a full explanation of the purpose of the study and the results of previous animal and clinical studies and submitted a written informed consent.
There were 75 subject patients, including 58 cases of secondary augmentation rhinoplasty after silicon implantation and 17 cases of primary augmentation rhinoplasty. Before culturing, all patients tested negative for human immunodeficiency virus, hepatitis B, hepatitis C, human T-cell leukemia virus-1, and syphilis. Autologous serum was obtained from each patient at the time of surgical collection of the auricular cartilage.
Multilayer Chondrocyte Culture System
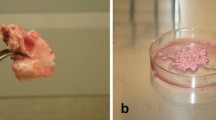
The harvested concha cartilage (approximately 2 × 1 cm, Fig. 1) was sterilized, treated in 0.3% collagenase (Worthington Biochemical, Freehold, NJ)/PBS (–) at 4°C, spun with a stirrer for 4 h at 37°C, and filtered through a BD FalconTM cell strainer of 100-μm pore size (BD Biosciences, San Jose, CA); then the chondrocytes were isolated. The obtained chondrocytes were seeded at a cell density of 1 × 103–104 cells/cm2 in a 75-cm2 culture flask, primary cultured, and then subcultured. At the third passage, cell counts were approximately 1000 times greater than the primary culture. The cells at the second or third passage were used for grafting. The culture medium was a DMEM medium supplemented with 10% autoserum, FGF-2 (5 ng/ml, FIBRAST®, Kaken Pharmaceuticals, Tokyo, Japan), and antibiotics [penicillin G (400 unit/ml, Meiji Seika Kaisha, Ltd., Tokyo, Japan), streptomycin sulfate (1 mg/ml, Meiji Seika Kaisha), and amphotericin B (2.5 μg/ml, Invitrogen, Carlsbad, CA)]. FGF-2 is clinically approved and used as a wound-healing agent in Japan. Finally, the chondrocytes obtained from the subculture were seeded at a density of 1 × 104 cells/cm2 three to four times over the previously seeded cells as described elsewhere [17, 18]. The chondrocytes cultured in this medium proliferated at a dedifferentiation state, and then the redifferentiated chondrocytes with the gelatinous chondroid matrix in a multilayer culture were obtained (Fig. 1). The cultured chondrocytes were washed once with PBS, collected, drawn into a syringe, and grafted. It was approximately 4 weeks from the primary culture to the grafting.
Scheme of the culture methods. The auricular chondrocytes were harvested from the auricular concha. The chondrocytes were cultured and proliferated at a dedifferentiation state, and then the redifferentiated chondrocytes with a gelatinous chondroid matrix in a multilayer culture were obtained. They were then aspirated into a syringe and prepared for injection-grafting
The number of chondrocytes in 1 cc of gel was 0.5–1 × 107 cells. The final volume of gelatinous-formed cells was 10–50 cc with a total of 0.5–5 × 108 cells. Before grafting the culture medium was checked for bacteria and microplasma to confirm it was free of contamination. Chondrocytes cultured in this manner were also cryopreserved for possible future use.
Surgical Procedure
The grafting is performed under local anesthesia and sedation in our office operating suite or other outpatient facility. The patient receives cefazolin 2 g before grafting and then takes oral penicillin 750 mg per day for 5 days. The nasal vestibule is prepared in the usual manner with 5% povidone-iodine solution.
CAC are aspirated into a 10-cc syringe, and then a 16-gauge indwelling needle (Terumo, Co., Tokyo, Japan) is attached. In the case of secondary augmentation rhinoplasty, the silicon implant located in the nasal dorsum is removed through a marginal incision that extends into the superior half of the columella in the case of L-shaped silicone implantation. Both edges of the capsule that is created around the implant are cut, and the base capsule is rasped. This is necessary to make the chondrocytes adhere to the base, to make a precise subcutaneous midline, and to create enough space. Next, the CAC are injection-grafted into the subcutaneous pocket. If the silicon implant is displaced or the capsule is calcified, the capsule is torn and removed and a cavity of an appropriate size is created. In the case of primary augmentation rhinoplasty, the external extent of the pocket is precisely marked with a marking pen. The exact dissection of the subcutaneous midline pocket is then done via an internal approach on the perichondrium and on the periosteum, and then the CAC are injection-grafted into the subcutaneous pocket. The volume of grafted cells is 20% more than the target volume because water content in the cultured chondrocytes is high and their volume decreases after grafting.
In the cases in which the skin had become thin and there was a concave deformity of the nasal tip, a grafting technique that uses both the CAC and the temporal fascia was used. The temporal fascia (approximately 2 × 4 cm, almost double the size of the nose tip) is harvested from the temporoparietal lesion. The fascia is prepared in a single layer or folded into a double layer depending on the skin thickness and grafted, and then the CAC are injection-grafted beneath the fascia.
After grafting CAC, we model the nasal dorsum using external digital maneuvers and the wound is tightly sutured with a 5-0 nylon thread. External fixation is very important and the aesthetic shape can be adjusted at this time. We apply a hydrocolloid sheet and micropore strips and always keep the form of the nasal dorsum and root. Finally, a cast is applied for 1 week. After 7 full days of fixation, the patient is instructed to apply the hydrocolloid sheet and micropore strips carefully for 3 weeks at night.
Results
The CAC achieved very good results with graft pliability upon digital pressure during the first 2 weeks. Approximately 3–4 weeks after grafting the CAC became solid cartilage. The results in our 75 patients are summarized in Table 1. The ages of the 75 patients ranged between 16 and 67 years old (average = 37.5 years). The number of grafted CAC with gelatinous chondroid matrix was 0.5–1 × 107cell/cc and the implantation volume was 0.5–10 cc (average = 2.9 cc). The follow-up period ranged from 6 months to 6 years 11 months (average = 3 years 8 months). No total absorption has been detected in any patient (Table 2).
In patients in whom there was excessive augmentation in a part of the nose, the excess tissue was resected after obtaining permission from the patient and the obtained tissue was histologically examined (Figs. 2 and 3). With toluidine blue staining, metachromasie was depicted and the presence of aglycan (a cartilage-specific differentiation marker) was confirmed (Fig. 3). With immunohistochemistry, cartilage-specific type II collagen was stained and showed the formation of human cartilage (Fig. 3). With EVG staining, the presence of elastic fibers that are specific to elastic cartilage was seen (Fig. 3). In radiograms, silicon implants are clearly depicted because of their low X-ray permeability, whereas CAC are not depicted because of their high X-ray permeability.
Histological findings of the grafted chondrocytes. Left Toluidine blue staining of the neocartilage 6 months after grafting depicted metachromasie. Center Immunochemistry 6 months after grafting depicted human type II collagen and showed the formation of human cartilage. Right EVG staining 6 months after grafting showed elastic cartilage that originated from auricular cartilage
Case Reports
Case 1
The results of this case were reported earlier [15]. A 23-year-old woman had abnormal skin color of the nasal tip and the silicone implant on the right side was drifting on the nasal dorsum. Four years earlier she had undergone a silicone nasal/chin augmentation. The skin on the nasal dorsum had become thin and reddish and indicated the possibility of implant exposure. After removing the L-shaped silicone implant, CAC 3.5 cc (120% after overcorrection) was injection-grafted into the subcutaneous pocket through a marginal incision (Fig. 4). Six years later the patient showed very good aesthetic results. Figures 5 and 6 show the clinical course of this patient.
Case 1: Upper left Preoperative view showing abnormal skin color and implant malposition. Upper right Abnormal skin color and implant malposition are seen. Lower left The skin on the nasal dorsum became thin (double arrows), and indicated the possibility of implant exposure. Lower right After removing the implant, CAC were injection-grafted into the subcutaneous pocket
Clinical course of case 1, left lateral views and radiographs. Upper left Preoperative view at 23 years old. Lower left Arrow shows silicone implant shadow on radiograph. Center Two years after CAC grafting (25 years old). Upper right Six years after CAC grafting (29 years old). Good nasal shape has been maintained. Lower right Silicone implant was not depicted on radiograph
Case No. 2
A 66-year-old woman had undergone silicone implant nasal augmentation 40 years earlier. She had a history that indicated episodes of nasal trauma in her childhood. After removing the I-shaped silicone implant surrounded by marked calcification, she had a severe saddle nose, a severely depressed radix, and resorption of the nasal bone. CAC 6 cc (120% after overcorrection) was injection-grafted into the subcutaneous pocket through a marginal incision. The patient showed acceptable results 1 year later (Figs. 7 and 8).
Case 2: Left Preoperative frontal view shows a steplike deformity and implant malposition. Center Operative findings show severe saddle nose, depressed radix, resorption of nasal bone and cartilage, and marked calcification around the removed implant. Right Postoperative view 1 year after CAC grafting. The radix and nasal projection were acceptable
Lateral views of case 2. Left Preoperative frontal view shows remarkable steplike deformity (single arrow). Center left Silicone implant surrounded by marked calcification (double arrow) and nasal bone resorption is shown on the radiograph. Center right Operative findings show severe saddle nose and depressed radix after removing the implant. Right Postoperative view 1 year after CAC grafting. The radix and nasal projection were acceptable
Case No. 3
A 63-year-old woman had undergone silicone implant nasal augmentation 15 years earlier. After removing the L-shaped silicone implant, she had abnormal skin color, depression of the nasal dorsum, and a concave deformity of the nasal tip. She underwent a combined grafting technique that uses both the CAC and the temporal fascia. The patient showed a good aesthetic result 1 year later (Figs. 9, 10, 11).
Case 3: Left Preoperative frontal view showing abnormal skin color and implant malposition. Center Operative findings after silicone removal showed that the nasal tip had marked concave deformity and the skin was thin. Right Postoperative view 1 year after the combination grafting using CAC and temporal fascia. The nasal contour was markedly aesthetically improved
Lateral views of case 3. Left Preoperative frontal view shows abnormal skin color and turned-up nose. Center Operative findings after silicone removal showed that the nasal tip had a marked concave deformity. Right One year after the combination grafting. The nasal contour was markedly aesthetically improved
Discussion
There are a variety of autologous materials available for nasal augmentation. Most surgeons have preferred autologous grafts because of their advantages, as published in the medical literature [1–9]. In the past, bone grafts (iliac bone and calvarial bone [2, 3]), cartilage grafts (e.g., nasal septal cartilage, auricular cartilage, and costal cartilage), and temporoparietal fascia [4–9] were used for dorsal nasal augmentation. These autologous materials have considerable advantages over synthetic materials, but at the same time they are associated with drawbacks such as significant donor site morbidity and limitations on the harvested tissue volume. Because of these reasons, synthetic materials such as silicone implants [10, 11] Gore-Tex [12], alloimplants [13], and AlloDerm® (LifeCell Corp., Branchburg, NJ) [14] are often used. We have invented a novel treatment method that uses autologous tissues and requires minimal donor site sacrifice. We succeeded in developing a new culture method in which sufficiently large amounts of CAC are developed from only 1 cm2 of auricular cartilage of the patient. This method has been clinically applied to our patients [15–19].
We used our cultured autologous chondrocyte grafting technique to treat 75 patients. Biopsy of the grafted cells of some patients histologically demonstrated the formation of auricular cartilage originated from the donor tissue. The patients have been followed up from 6 months to 6 years after grafting (Table 1), and total absorption has not occurred (Table 2). In 17 primary augmentation cases, 2 patients who had tight skin had partial absorption on the nasal tip. Among the 58 secondary augmentation cases, 5 patients had partial absorption on the nasal dorsum or tip.
Improvement was also made in our grafting technique for patients whose nasal tip became thin because of a silicone implant that had been placed much earlier. Several reports proposed the use of free temporoparietal deep fascia combined with cartilage for dorsal augmentation [7–9]. We thought that the subcutaneous tissues of such patients would become thinner when filled only with cartilaginous tissue (hard tissue). Therefore, we used grafting of temporal fascia as a soft tissue filling in combination with the grafting of CAC.
Our CAC method has many advantages over other augmentation methods: (1) A large volume of autologous graft material can be produced with minimal damage to the donor site. (1) The graft volume is taken well. (3) Patients do not feel the presence of a foreign body. (4) The shape and volume of the graft is easily adjustable because cultured chondrocytes are injection-grafted. (5) The cells can be cryopreserved for future cultures when additional grafting is needed. However, there are disadvantages: (1) The treatment period becomes longer, as long as the culture period. (2) Cost of treatment increases because of the cell culture equipment and technology. (3) Small adjustments in the millimeter range are difficult because chondrocytes are in a gelatinous form and not in a shaped block. (4) The cultured cells are not suited for cosmetic surgery of the external nose or the wing of the nose because of the above-mentioned reasons. (5) The cultured cells are susceptible to infections so have to be managed with strict hygiene control and administration of antibiotics. (6) This grafting method is still not fully free from the risk of cartilage absorption after grafting.
A longer study is needed to examine absorption of the grafted chondrocytes. However, in this grafting method, minor absorption is not a problem because chondrocytes are cryopreserved for future additional grafting. This method using cultured chondrocytes would be very useful and beneficial as a novel nasal augmentation technique and could be used for various treatments including facial augmentation.
References
Maas CS, Monhian N, Shah SB (1997) Implants in rhinoplasty. Facial Plast Surg 13:279–290
Wheeler ES, Kawamoto HK, Zarem HA (1982) Bone grafts for nasal reconstruction. Plast Reconstr Surg 69:9–18
Jackson IT, Choi HY, Clay R, Bevilacqua R, TerKonda S, Celik M, Smith AW (1998) Long-term follow-up of cranial bone graft in dorsal nasal augmentation. Plast Reconstr Surg 102:1869–1873
Gurley JM, Pilgram T, Perlyn CA, Marsh JL (2001) Long-term outcome of autogenous rib graft nasal reconstruction. Plast Reconstr Surg 108:1895–1905
Cardenas-Camarena L, Guerrero MT (1999) Use of cartilaginous autografts in nasal surgery: 8 years of experience. Plast Reconstr Surg 103:1003–1014
Çelik M, Haliloglu T, Bayçin N (2004) Bone chips and diced cartilage: an anatomically adopted graft for the nasal dorsum. Aesth Plast Surg 28:8–12
Erol OO (2000) The Turkish delight: a pliable graft for rhinoplasty. Plast Reconstr Surg 105:2229–2241
Guerrerosantos J, Trabanino C, Guerrerosantos F (2006) Multifragmented cartilage wrapped with fascia in augmentation rhinoplasty. Plast Reconstr Surg 117:804–812
Guerrerosantos J (1984) Temporoparietal free fascia grafts in rhinoplasty. Plast Reconstr Surg 74:465–475
McCurdy JA Jr (2002) The Asian nose: augmentation rhinoplasty with L-shaped silicone implants. Facial Plast Surg 18:245–252
Zeng Y, Wu W, Yu H, Yang J, Chen G (2002) Silicone implants in augmentation rhinoplasty. Aesthetic Plast Surg 26:85–88
Owsley TG, Tayler CO (1994) The use of Gore-Tex for nasal augmentation: a retrospective analysis of 106 patients. Plast Reconstr Surg 94:241–248
Romo T 3rd, Sclafani AP, Sabini P (1998) Reconstruction of the major saddle nose deformity using composite allo-implants. Facial Plast Surg 14:151–157
Gryskiewicz JM, Rohrich RJ, Reagan BJ, Schwartz BM (2001) The use of AlloDerm for the correction of nasal contour deformities. Plast Reconstr Surg 107:571
Yanaga H, Koga M, Imai K, Yanaga K (2004) Clinical application of biotechnically cultured autologous chondrocytes as novel graft material for nasal augmentation. Aesthetic Plast Surg 28:212–221
Yanaga H, Yanaga K, Imai K, Koga M, Soejima C, Ohmori K (2006) Clinical application of cultured autologous human auricular chondrocytes with autologous serum for craniofacial or nasal augmentation and repair. Plast Reconstr Surg 117:2019–2030
Yanaga H, Imai K, Yanaga K (2007) Clinical application of cultured autologous human auricular chondrocytes to cranio-facial, nasal and/or ear reconstruction: overall results in basic studies and 60 patients. Plast Reconstr Surg Suppl 120:73–74 (abstract)
Yanaga H, Imai K, Yanaga K (2008) Clinical application of cultured autologous human auricular chondrocytes for nasal augmentation. 19th Congress of the International Society of Aesthetic Plastic Surgery, Melbourne, Australia 10–13 February 2008, pp 49–50
Yanaga H, Imai K, Fujimoto T, Yanaga K (2009) Generating ears from cultured autologous auricular chondrocytes by using two-stage implantation in microtia treatment. Plast Reconstr Surg (in press)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yanaga, H., Imai, K. & Yanaga, K. Generative Surgery of Cultured Autologous Auricular Chondrocytes for Nasal Augmentation. Aesth Plast Surg 33, 795–802 (2009). https://doi.org/10.1007/s00266-009-9399-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-009-9399-8