Abstract
Background
In 2005 we reported a study on the efficacy of the preoperative use of the selective COX-2 inhibitor celecoxib (Celebrex) for reducing both postoperative pain and opioid requirements in patients undergoing bilateral subpectoral breast augmentation. Our findings showed that patients who received 400 mg of celecoxib 30 min before surgery required significantly less postoperative opioid analgesics compared with those given a placebo. Gabapentin (Neurontin) is an agent commonly used to control neuropathic pain. Here we describe a prospective study assessing the efficacy of preoperative gabapentin in combination with celecoxib for reducing postoperative pain and opioid requirements in elective subpectoral breast augmentation.
Methods
One hundred eighteen patients were given 1200 mg of gabapentin and 400 mg of celecoxib 30–60 min before surgery. From the day of surgery until postoperative day 5, patients documented any use of analgesics and recorded their degree of pain. Results were then compared with those of our previous study in which only celecoxib was used.
Results
The combination of gabapentin and celecoxib was found to be significantly superior (p < 0.001) in reducing postoperative pain and opioid requirements than celecoxib alone in the management of postoperative pain and opioid requirements.
Conclusion
To decrease postoperative opioid requirements, we recommend 400 mg of celecoxib and 1200 mg of gabapentin taken 30–60 min before surgery by patients undergoing subpectoral breast augmentation or a comparable plastic surgery procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative pain control is an essential part of elective breast augmentation and is inveterately managed with opioid-containing compounds such as oxycodone/acetaminophen (Percocet), hydrocodone/acetaminophen (Vicodin), and meperidine. Unfortunately, these agents are notorious for both their analgesic inadequacy and objectionable side effects of nausea, vomiting, constipation, somnolence, dizziness, and a clouded sensorium [1–3]. Effective alternatives to opioids have included celecoxib, a COX-2 inhibitor believed to affect analgesia by inhibition of cyclooxygenase, an enzyme involved in the conversion of plasma membrane-derived arachidonic acid into proinflammatory and hyperalgesic prostaglandins and thromboxanes [4]; and gabapentin, an anticonvulsant/antihyperalgesic thought to reduce the hyperexcitability of dorsal horn neurons following tissue damage [5]. When used to control postoperative pain, both celecoxib and gabapentin have been shown to have a significant opioid-sparing efficacy [6–16].
In a 2005 report published in this journal, we described a prospective study in which patients who received a single 400 mg oral dose of celecoxib 30 min before subpectoral breast augmentation required significantly less postoperative opioids [14]. To further diminish opioid use, we undertook the present prospective study to assess the efficacy of preoperative celecoxib in combination with gabapentin. Using the study population from our 2005 study as a control group (hereafter referred to as control group), we compared the use of celecoxib plus gabapentin (combination group) to the use of celecoxib alone for reducing postoperative pain and opioid use.
Materials and Methods
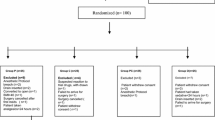
Between 2005 and 2008, women undergoing elective bilateral subpectoral breast augmentation for diagnosed breast hypoplasia were asked to volunteer for this study. All patients were women with no prior history of breast surgery, and neither mastopexy nor any other concurrent procedures were performed. Patients were excluded from this study if they had used any opioid analgesics for longer than 30 days in the 5 years prior to surgery. Patients with an allergy to COX-2 inhibitors, gabapentin, acetaminophen, or hydrcodone were excluded from the study. All women received Inamed-McGhan textured saline implants inserted submuscularly by the same surgeon (FDP) under intravenous sedation (propofol, diazepam, and ketamine) and local anesthesia (0.25% lidocaine with 1:400,000 epinephrine) on an outpatient basis. No opioids, including morphine, meperidine, or sublimase, were administered during the procedure. The incidence of nausea and vomiting in the PACU was recorded.
A total of 118 patients qualified for the study. Patient ages ranged from 23 to 62 years, with a mean of 31.2 years. The patients were 73.4% Asian or of a mixed Asian ancestry. The remaining identified themselves as Caucasian, Filipino, part-Hawaiian, or “other.” All patients were given an oral dose of 1200 mg of gabapentin and 400 mg of celecoxib with a sip of water 30–60 min before surgery. These doses were recommended previously by other clinical studies [3, 7, 10, 17]. All patients had access to acetaminophen (1000 mg every 6 h as needed) as well as 5 tablets of Vicodin (5 mg hydrocodone/500 mg acetaminophen per tablet) in the event that acetaminophen was insufficient. The rationale for the administration of celecoxib and gabapentin was explained to the patients by the operating surgeon during their preoperative visit, which occurred approximately 2 weeks before surgery, and was reiterated on the day of the procedure.
The mechanism of pain and the importance of endorphines were explained to all patients and they were provided the form shown in Fig. 1 to read carefully prior to surgery and to return to the office on their postoperative visit. They were also asked to answer the questions at the end of the form.
Beginning on the day of surgery and ending on the fifth postoperative day, patients experiencing pain requiring the use of analgesics were asked to record the date, time, type of medication (either Tylenol or Vicodin), and the intensity of their pain on a provided form. Pain intensity was quantified by the following scale: 0 for nil; 1 for mild pain (annoying, nagging); 2 for discomforting (troublesome, nauseating, grueling, numbing); 3 for distressing (miserable, agonizing gnawing); 4 for intense (dreadful, horrible, vicious, cramping); and 5 for excruciating pain (unbearable, torturing, crushing, tearing) as shown in Fig. 2.
Statistical analyses were conducted using Fisher’s exact test with mid-p, two-sided values of p < 0.05 considered significant. These results were compared to previous data in which only celecoxib had been utilized, the control group [14].
Results
Patient cooperation was 100%. No patient refused to take the 400 mg of celecoxib and the 1200 mg of gabapentin preoperatively, and all 118 patients complied with the use of their questionnaires. No allergic reactions were noted either before or after the procedures and no patient developed nausea and/or vomiting as a result of preoperative ingestion of celecoxib and gabapentin.
In response to questions 1 and 2 in Fig. 1, 109 patients (92.4%) found the preoperative explanations of the rationale for the use of celecoxib and gabapentin and their education regarding endorphins very clear and very understandable. The remaining 9 patients (7.6%) found the explanations somewhat clear and somewhat understandable.
In the combination group, 113 patients (95.8%) took only acetaminophen or no analgesics at all after surgery compared with 19.9% of patients in the control group [14]; this was found to be a significant difference (p < 0.001). With regard to opioid use, five patients (4.2%) in the combination group required supplemental Vicodin (a total of 18 Vicodin tablets were consumed) in contrast to 18.2% in the control group [14]; this also was found to be significant (p < 0.01).
In the combination group, nil (score of 0) or mild (score of 1) pain was reported by 14 patients (11.9%), with a mean pain score of 0.78. The average age of these 14 patients was 44.8 years. Intense pain (score of 4 or 5) was reported by 9 patients (7.6%) on at least one occasion, with a mean score of 4.4. The mean age in this group was 37.1 years. However, five of the nine patients who rated their pain as intense also had a history of smoking compared with none of the 14 who rated their pain as nil or mild. All had been asked to stop smoking for 6 weeks before and after surgery. The difference in pain scores between smokers and nonsmokers was significant (p < 0.005), which was in accordance with our previous study [14]. The remaining 95 patients (80.5%) experienced a mean pain intensity rating of 1.84, or pain ranging from mild to discomforting.
Thirty-eight patients (32.2%) decided not to fill their Vicodin prescriptions either before or after the operation, stating they did not believe it was warranted in light of the preoperative education they had received. When interviewed at their postoperative follow-up, all of these patients believed this decision was justified. These 38 patients also had the lowest pain intensity score, ranging from 0 to 2 and with a mean of 0.67. The mean age in this patient subgroup was 40.3 years.
Discussion
In a previous report, we showed a significant benefit of the preoperative oral administration of 400 mg of celecoxib for reducing both postoperative pain and opioid requirements [14]. Several other studies have demonstrated the opioid-sparing efficacy of preoperatively administered selective COX-2 inhibitors in reducing postoperative pain after dental surgery [13], bunionectomy [7], spinal fusion surgery [16], thyroid surgery [11], and abdominal hysterectomy [12]. This current study was undertaken in an attempt to further improve postoperative pain management by adding gabapentin to the celecoxib regimen. Hurley et al. [18] reported on the synergistic effects of combining the nonselective naproxen with gabapentin and pregabalin. In 2006, after we had begun our study, Reuben et al. [19] found the beneficial effect of combining celecoxib with pregabalin for spinal fusion surgery. In the same year, Turan et al. [20] demonstrated the efficacy of combining gabapentin with rofecoxib in reducing postoperative pain and opioid use following abdominal hysterectomy. In that study, patients were administered a regimen of either a placebo, 50 mg of rofecoxib alone, 1200 mg of gabapentin alone, or the combination of rofecoxib and gabapentin on the morning of surgery and every subsequent morning through postoperative day 2 [20]. Patients were also administered IV fentanyl 3-5 min before the initial skin incision and had access to patient-controlled morphine postoperatively. A report by Gilron et al. [21] demonstrated the efficacy of rofecoxib and gabapentin in reducing movement-related pain after abdominal hysterectomy, although it similarly allowed for the administration of both pre- and perioperative opioids and patients had access to a bolus-only morphine PCA postoperatively. We found no trials in the literature that combined celecoxib and gabapentin or combined any selective COX-2 inhibitor with gabapentin on an outpatient basis and that completely avoided pre-, peri-, or postoperative IV opioid use.
Selective COX-2 inhibitors were originally developed as chronic pain medications that offered the pain-relieving benefits of nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) with fewer adverse gastrointestinal effects. Their demonstrated efficacy in treating postsurgical and acute medical pain has expanded their use. The theory behind the preoperative administration of selective COX-2 inhibitors is that inhibition of COX-2-mediated prostaglandin synthesis reduces nociceptive pain and prevents inflammatory-induced hyperalgesia [4, 14]. It has been shown that the administration of 400 mg of celecoxib before surgery is as effective as when it is administered postoperatively in major plastic surgery cases [17].
Although the precise mechanism by which gabapentin produces analgesia is unknown, the compound has been shown to bind to the α-2-τ subunit of presynaptic voltage-gated calcium channels, thus reducing calcium influx and inhibiting the release of excitatory amino acids [22–24]. These channels are upregulated in the dorsal root ganglia and spinal cord after surgical trauma. In animal models, gabapentin has been shown to prevent allodynia and hyperalgesia [10, 25] and pain-related responses in several models of neuropathic pain [26, 27]. Other theories about the analgesic effects of gabapentin relate to its inhibitory effect on dorsal horn N-methyl-D-aspartic acid (NMDA) receptors [5, 6, 28, 29]. Gabapentin is generally well tolerated by patients and the most common adverse effects reported in clinical trials of neuropathic pain are somnolence, dizziness, ataxia, and fatigue [19, 30–32].
It has been demonstrated that the administration of morphine downregulates μ-opioid receptor synthesis and pro-opiomelanocortin (POMC)—the precursor of β-endorphins—mRNA expression in an animal model [33, 34]. Both endogenous β-endorphins and exogenous opioids act on these receptors to decrease the release of substance P and, consequently, pain. Endogenous opioids such as β-endorphin (β-EP) and methionine-enkephalin (M-EK) play an important role in the modification of pain perception, and studies have suggested that higher preoperative cerebrospinal fluid concentrations of these endogenous opioids are associated with longer periods of analgesia and less postoperative morphine requirements [35]. The interplay of exogenous and endogenous opioids continues to be an area of active clinical investigation, particularly as it relates to postoperative pain. β-EP levels appear to be increased under surgical stress, and it appears that this response can be effectively blunted using a spinal or systemic delivery of narcotics [36]. However, clinical observations also suggest that intraoperative narcotics can induce postoperative hyperalgesia, possibly via inhibition of endogenous opioids [37]. Therefore, investigations into non-narcotic options for the management of postoperative pain continue to be actively pursued.
It is possible that pain experienced by patients in this study in the immediate postoperative period may be the necessary trigger for the implementation of these endogenous pain relief mechanisms. Our current preoperative regimen of celecoxib and gabapentin administered 30–60 min before surgery may create an ephemeral period of immediate postoperative pain, although we have found that patients tolerate this discomfort if properly educated about the value of endorphins in long-term recovery. Whether or not a placebo effect is operational is beyond the scope of this report. Future researchers may investigate this question. However, if a placebo effect has contributed to our results, we would certainly welcome and laud its consistent and beneficial role.
We have found that older patients, with an average age of 40.3 years and nonsmokers, reported the lowest pain intensity and no postoperative Vicodin use. Although age-related discrepancies have been reported both in the perception and reporting of pain [38, 39], our study can neither verify nor disqualify these conclusions.
This report demonstrates the significant advantage of combined preoperative administration of gabapentin and celecoxib over celecoxib alone in patients undergoing subpectoral breast augmentation. We find that patient education about the mechanism of action of analgesics and the importance of preserving the endogenous endorphins very important and must be communicated to all patients on their preoperative visits. We ensure proper patient education 2 weeks before surgery and reiterate any salient points on the morning of surgery. We have extended our current preoperative celecoxib/gabapentin regimen to other patients undergoing different aesthetic procedures such as breast reduction, mastopexy, abdominoplasty, liposuction, face lift, blepharoplastyand endoscopic brow lift with similar favorable outcomes.
Conclusion
The preoperative administration of 400 mg of celecoxib combined with 1200 mg of gabapentin 30-60 min before subpectoral breast augmentation significantly reduces postoperative pain and opioid requirements. This effect is significantly superior to the administration of celecoxib alone. Therefore, we recommend that a combination of celecoxib and gabapentin be administered to all patients undergoing elective subpectoral breast augmentation. Other procedures of similar intensity may also benefit from this regimen. Preoperative education so as to ensure that patients have a basic understanding of analgesic drugs, pain pathways, and the production of endogenous endorphins appears paramount to success.
References
Bekker A, Cooper PR, Frempong-Boadu A, Babu R, Errico T, Lebovits A (2002) Evaluation of preoperative administration of the cyclooxygenase-2 inhibitor rofecoxib for the treatment of postoperative pain after lumbar disc surgery. Neurosurgery 50:1053–1057
Glasson JC, Sawyer WT, Lindley CM, Ginsberg B (2002) Patient-specific factors affecting patient-controlled analgesia dosing. J Pain Palliat Care Pharmacother 16:5–21
Sinclair DR, Chung F, Mezei G (1999) Can postoperative nausea and vomiting be predicted? Anesthesiology 91:109–118
Needleman P, Isakson PC (1997) The discovery and function of COX-2. J Rheumatol Suppl 49:6–8
Johnson S, Johnson FN, Johnson RD, Armer ML et al (2001) Gabapentin in neuropathic pain. In: Johnson S, Johnson FN, Johnson RD, Armer ML (eds) Reviews in contemporary pharmacotherapy. Marius Press, Carnforth, UK, pp 125–211
Dahl JB, Mathiesen O, Møiniche S (2004) ‘Protective premedication’: an option with gabapentin and related drugs? A review of gabapentin and pregabalin in the treatment of post-operative pain. Acta Anaesthesiol Scand 48:1130–1136
Desjardins PJ, Shu VS, Recker DP, Verburg KM, Woolf CJ (2002) A single preoperative oral dose of valdecoxib, a new cyclooxygenase-2 specific inhibitor, relieves post-oral surgery or bunionectomy pain. Anesthesiology 97:565–573
Dirks J, Fredensborg BB, Christensen D, Fomsgaard JS, Flyger H, Dahl JB (2002) A randomized study of the effects of single-dose gabapentin versus placebo on postoperative pain and morphine consumption after mastectomy. Anesthesiology 97:560–564
Fassoulaki A, Patris K, Sarantopoulos C, Hogan Q (2002) The analgesic effect of gabapentin and mexiletine after breast surgery for cancer. Anesth Analg 95:985–991
Field MJ, Holloman EF, McCleary S, Hughes J, Singh L (1997) Evaluation of gabapentin and S-(+)-3-isobutylgaba in a rat model of postoperative pain. J Pharmacol Exp Ther 282:1242–1246
Karamanlioğlu B, Turan A, Memiş D, Türe M (2004) Preoperative oral rofecoxib reduces postoperative pain and tramadol consumption in patients after abdominal hysterectomy. Anesth Analg 98:1039–1043
Koppert W, Angst M, Alsheimer M, Sittl R, Albrecht S, Schüttler J, Schmelz M (2003) Naloxone provokes similar pain facilitation as observed after short-term infusion of remifentanil in humans. Pain 106:91–99
Malmstrom K, Daniels S, Kotey P, Seidenberg BC, Desjardins PJ (1999) Comparison of rofecoxib and celecoxib, two cyclooxygenase-2 inhibitors, in postoperative dental pain: a randomized, placebo- and active-comparator-controlled clinical trial. Clin Ther 21:1653–1663
Parsa AA, Soon CWM, Parsa FD (2005) The use of celecoxib for reduction of pain after subpectoral breast augmentation. Aesth Plast Surg 29:441–444
Recart A, Issioui T, White PF, Klein K, Watcha MF, Stool L, Shah M (2003) The efficacy of celecoxib premedication on postoperative pain and recovery times after ambulatory surgery: a dose-ranging study. Anesth Analg 96:1631–1635
Rønnekleiv OK, Bosch MA, Cunningham MJ, Wagner EJ, Grandy DK, Kelly MJ (1996) Downregulation of mu-opioid receptor mRNA in the mediobasal hypothalamus of the female guinea pig following morphine treatment. Neurosci Lett 216:129–132
Sun T, Sacan O, White PF, Coleman J, Rohrich RJ, Kenkel JM (2008) Perioperative versus postoperative celecoxib on patient outcomes after major plastic surgery procedures. Anesth Analg 106:950–958
Hurley RW, Chatterjea D, Rose Feng M, Taylor CP, Hammond DL (2002) Gabapentin and pregabalin can interact synergistically with naproxen to produce antihyperalgesia. Anesthesiology 97:1263–1267
Reuben SS, Connelly NR (2000) Postoperative analgesic effects of celecoxib or rofecoxib after spinal fusion surgery. Anesth Analg 91:1221–1225
Turan A, White PF, Karamanlioglu B, Memis D, Tasdogan M, Pamukçu Z, Yavuz E (2006) Gabapentin: an alternative to the cyclooxygenase-2 inhibitors for perioperative pain management. Anesth Analg 102:175–181
Gilron I, Orr E, Tu D, O’Neill JP, Zamora JE, Bell AC (2005) A placebo-controlled randomized clinical trial of perioperative administration of gabapentin, rofecoxib and their combination for spontaneous and movement-evoked pain after abdominal hysterectomy. Pain 113:191–200
Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN (1996) The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha-2-delta subunit of a calcium channel. J Biol Chem 271:5768–5776
Maneuf YP, Hughes J, McKnight AT (2001) Gabapentin inhibits the substance P-facilitated K(+)-evoked release of [(3)H]glutamate from rat caudial trigeminal nucleus slices. Pain 93:191–196
Matejec R, Ruwoldt R, Bödeker RH, Hempelmann G, Teschemacher H (2003) Release of beta-endorphin immunoreactive material under perioperative conditions into blood or cerebrospinal fluid: significance for postoperative pain? Anesth Analg 96:481–486
Whiteside GT, Harrison J, Boulet J, Mark L, Pearson M, Gottshall S, Walker K (2004) Pharmacological characterisation of a rat model of incisional pain. Br J Pharmacol 141:85–91
Woolf CJ, Salter MW (2000) Neuronal plasticity: increasing the gain in pain. Science 288:1765–1769
Woolf CJ, Max MB (2001) Mechanism-based pain diagnosis: issues for analgesic drug development. Anesthesiology 95:241–249
Taylor CP, Gee NS, Su TZ, Kocsis JD, Welty DF, Brown JP, Dooley DJ, Boden P, Singh L (1998) A summary of mechanistic hypotheses of gabapentin pharmacology. Epilepsy Res 29:233–249
Scholz J, Woolf CJ (2002) Can we conquer pain? Nat Neurosci 5(Suppl):1062–1067
Bone M, Critchley P, Buggy DJ (2002) Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med 27:481–486
Serpell MG, Neuropathic pain study group (2002) Gabapentin in neuropathic pain syndromes: a randomised, double-blind, placebo-controlled trial. Pain 99:557–566
Turan A, Karamanlioğlu B, Memiş D, Hamamcioglu MK, Tükenmez B, Pamukçu Z, Kurt I (2004) Analgesic effects of gabapentin after spinal surgery. Anesthesiology 100:935–938
Fang Y, Kelly MJ, Rønnekleiv OK (1998) Proopiomelanocortin (POMC) mRNA expression: distribution and region-specific down-regulation by chronic morphine in female guinea pig hypothalamus. Brain Res Mol Brain Res 55:1–8
Rice AS, Maton S (2001) Gabapentin in postherpetic neuralgia: a randomised, double blind, placebo controlled study. Pain 94:215–224
Nader-Djalal N, de Leon-Casasola OA, Peer GL, Vladutiu AO, Lema MJ (1995) The influence of preoperative concentrations of beta-endorphin and met-enkephalin on the duration of analgesia after transurethral resection of prostate. Anesth Analg 81:591–595
Marais E, Klugbauer N, Hofmann F (2001) Calcium channel alpha(2)delta subunits—structure and gabapentin binding. Mol Pharmacol 59:1243–1248
Karamanlioğlu B, Arar C, Alagöl A, Colak A, Gemlik I, Süt N (2003) Preoperative oral celecoxib versus preoperative oral rofecoxib for pain relief after thyroid surgery. Eur J Anaesthesiol 20:490–495
Gagliese L, Katz J (2003) Age differences in postoperative pain are scale dependent: a comparison of measures of pain intensity and quality in younger and older surgical patients. Pain 103:11–20
Gagliese L, Katz J, Melzack R (1999) Pain in the elderly. In: Wall PD, Melzack R (eds) Textbook of pain. Churchill Livingstone, Edinburgh, pp 991–1006
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parsa, A.A., Sprouse-Blum, A.S., Jackowe, D.J. et al. Combined Preoperative Use of Celecoxib and Gabapentin in the Management of Postoperative Pain. Aesth Plast Surg 33, 98–103 (2009). https://doi.org/10.1007/s00266-008-9230-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-008-9230-y