Abstract
In men, the development of feminized breasts may cause significant emotional distress and embarrassment, particularly in young men and adolescents. Unfortunately, gynecomastia responds poorly to diet and exercise, and conventional corrective surgery may produce large stigmatizing areolar or chest scars and a flattened or concave chest. In 2004, board-certified plastic surgeons performed 16,275 corrective procedures, and in 2005 there was a 17% increase, according to The American Society of Plastic Surgeons (ASPS) procedural statistics. This report describes a surgical approach for removal of both glandular and adipose tissue using a small 3-mm areolar stab wound incision and a piecemeal glandular resection to correct gynecomastia with minimal and imperceptible external scarring. Pectoral etching of the chest and suction lipectomy are performed simultaneously to enhance and define the thoracic musculature and further virilize the upper thorax. Excellent results have been obtained with minimal complications. The authors present their experience with more than 200 consecutive cases over the past 4 years. They are very optimistic with these results because they have obtained a high degree of patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An estimated 32% to 65% of males are affected by gynecomastia, [1–4] an increase in breast tissue, which varies in severity from overt chest feminization to modest excess [6,9]. The condition may develop at puberty as a result of obesity, cancer, or consumption of estrogens, anabolic steroids, or H2 blockers such as cimetidine [2,12]. In addition, gynecomastia is reported to be a side effect of several prescription and over-the-counter drugs, medications, and supplements including Effexor, Motrin, Pepcid, and digitalis purpurea, also known as foxglove. Heavy marihuana use also has been linked to gynecomastia.
Gynecomastia induced by pubertal hormone fluctuations often resolves spontaneously. Defective androgen receptors or altered breast sensitivity to estrogen will functionally emulate a distorted estrogen-to-androgen hormonal ratio [2,8].
Bodybuilders who use steroids or supplements such as Prohormone, an-over-the-counter substance designed to convert into active hormones, are prime candidates for gynecomastia. Prohormone can increase the amount of estrogen in the body, which in males would cause the breast gland to become overactive, thus increasing a man’s breast size.
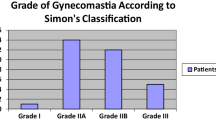
The three terms typically used to categorize gynecomastia are true gynecomastia, referring specifically to glandular enlargement; pseudogynecomastia, referring to chest lipodystrophy; and mixed gynecomastia, which describes a breast with both fatty deposits and glandular hypertrophy [15]. Severity may be assessed using the Simon, Hoffman, and Kahn scale [12]. Because a benign or malignant breast tumor may resemble gynecomastia, samples of excised tissue should be sent to pathology postoperatively, particularly in cases of glandular asymmetry.
Ideally, surgery will masculinize chest contours while protecting areolar anatomy and position. Tumescent liposuction is an effective remedy for chest lipodystrophy [3]. However, the removal of breast glands necessitates additional consideration because conventional surgical methods of extraction typically create prominent scars. Liposuction alone usually will not fully correct a significant proportion of gynecomastia cases. In addition, the recurrence rate may be higher when the breast gland is not resected.
Subareolar glandular pedicle or periareolar methods of gland excision use a circumareolar incision [1,9,12–15], which commonly results in conspicuous scarring, permanent pigment changes, and mismatched breasts or nipples [4]. The “pull-through” approach described by Morselli [8] is similar to our method in its aim to remove glandular tissue through small incisions. However, the Morselli technique differs most sharply in its reliance on the liposuction cannula for tissue undermining.
A pitfall in the surgical correction of gynecomastia is overzealous tissue removal, which may produce a flat, plane-like thorax with the potential for irregularity and concavity. The extent and placement of postoperative scarring is an important consideration.
We describe a modified technique for removal of glands through small 3-mm puncture incisions, with optional suction-assisted lipectomy to improve contouring through an axillary puncture incision.
Materials and Methods
More than 200 male patients ranging in age from 13 to 78 years (average, 22 years) underwent surgery with a single puncture excision of their enlarged breasts. The procedure was complemented with suction-assisted lipectomy (etching) of the pectoral musculature and chest [5,6]. The procedure was performed in a fully accredited facility with the patients under general endotracheal anesthesia. The postoperative follow-up period ranged from 3 to 60 months.
Marking and Preparation
In a supine position, the chest is firmly palpated, with particular attention given to assessing and marking the perimeter of individual mammary glands. While standing, the patient flexes his trunk muscles to aid in outlining of the sternum and the pectoral muscle at its lateral, inferior, and medial borders. Tumescent Klein solution with 1 ml of triamcinolone 10 mg (for resolution of edema and diminution of postoperative bruising) is used for infiltration.
True gynecomastia requires only one puncture incision at the 6 o’clock position of the inferior areolar margin for manual removal of the patient’s hypertrophied gland. Glandular hypertrophy may present as a single or a bilateral deformity. Mixed gynecomastia requires two incision sites, marked bilaterally at the anterior axillary fold and at the 6 o’clock position in the inferior areolar margin for gland removal (Fig. 1).
Liposuction through axillary and areolar incisions (upper left). Superficial subareolar dissection and transection of ductal components (upper right). Subglandular dissection and skeletization of glandular structures (lower left). Excision of glandular components in strips and their removal through an areolar incision (lower right).
Surgical Technique
Liposuction and gland removal flatten the chest. To eliminate the rounded, feminized appearance of gynecomastia, chest adipose tissue is suctioned with a 3-mm cannula at the lateral, medial, and inferior borders of the pectoralis major (Fig. 2). This pectoral-contouring approach (etching) accentuates a muscular, masculine appearance [6]. Typically, 50 to 500 ml of aspirate are removed. Intraoperative results correlate closely with the final result. Patients are instructed to wear a vest compression garment for 4 weeks. Oral antibiotics and pain medications are given during the first week after surgery.
Puncture incisions are made with a #15 blade for liposuction and gland excision. To extract the mammary gland, subareolar dissection is performed through the areolar puncture at the 6 o’clock position with blunt-tipped scissors. The mammary ducts connecting the nipple to the gland are thus transected at the level of the lactiferous sinus. Using the scissors to dissect the superior and posterior aspect of the gland, the ligamentous connecting fibers are cut, resulting in a detached and nearly free-floating gland. The gland then is transected along its length, and individual pieces are removed with forceps. One 4-0 catgut suture is placed to close the dermis.
For some patients, postoperative subareolar fullness develops as a result of scar deposition. To prevent furrowing of the nipple, 0.3 ml of triamcinolone 10 mg may be injected under the nipple into the deeper scar tissue to smooth excess collagen formation.
Results
From January 2004 to January 2007, we operated on more than 200 men and young adolescents ranging in age from 13 to 78 years (Figs. 3–6).
Possible complications from this procedure may include undercorrection, unevenness, infection, bruising, sensation changes, skin redundancy, areolar wrinkling, overcorrection, and hematoma. Our total complication rate was 2.5%.
Redundant areolar skin occurred after gland removal for 1 (0.5%) of the 200 patients who underwent this technique, requiring a minor in-office revision to remove an ellipse of areolar skin. In two patients (1.0%), a small hematoma developed, which required evacuation at the clinic. No other significant complications or gynecomastia recurrences were encountered. Two patients (1.0%) required secondary suctioning because of undercorrection. No patient experienced unevenness, permanent sensation changes, or infection.
Discussion
Imperceptible 3-mm incisions are of particular value to younger gynecomastia patients, for whom prominent nipple scars might become a new source of shame and self-consciousness. Our method refines and improves upon existing traditional techniques, offering a less outwardly invasive approach, with a highly gratifying result. The removal of hypertrophic or enlarged breast glands with excessive fat tissue produces an improved appearance and projection of the male torso. The ability to extract these glands with a minimal incision that creates an inconspicuous scar is a significant improvement over the established surgical techniques.
The described procedure removes the stigma that results from a man having a physical appearance normally found in women. Correction of gynecomastia translates to greater confidence and self-esteem. It does more than fix a physical problem. It can make a profound impact on the patient’s emotional and psychological life.
References
Celebioglu S, Ertas NM, Ozdil K, Oktem F: Gynecomastia treatment with subareolar glandular pedicle. Aesth Plast Surg 28:281–286, 2004
Delle Fave GE, Tamburrano G, DeMagistris L: Gynaecomastia with cimetidine. Lancet i:1319, 1977
Matarasso SL: Liposuction of the chest and back. Dermatol Clin 17:799–804, 1999
McGrath MH, Mukerji S: Plastic surgery and the teenage patient. J Pediatr Adolesc Gynecol 13:105–118, 2000
Mentz H, Gilliland M, Patrovella C, Abdominal Etching: Differential liposuction to detail abdominal musculature. Aesth Plast Surg 17:287–290, 1993
Mentz HA, Ruiz-Razura A, Newall G, Patronella CK: For men only: Body contouring for the athlete. Plast Surg Products, pp. 26–32, December 2004
Mentz HA, Ruiz-Razura A, Newall G, Patronella CK: Pectoral etching: A method for augmentation, delineation, and contouring the thoracic musculature in men. In Press. Accepted for publication in Plast Reconstr Surg July 18, 2006
Morselli S: Pull-through: A new technique for breast reduction in gynecomastia. Plast Reconstr Surg 97:450–454, 1996
Prezioso D, Piccirillo G, Galasso R, Altieri V, Mirone V, Lotti T: Gynecomastia due to hormone therapy for advanced prostate cancer: A report of ten surgically treated cases and a review of treatment options. Tumori 90:410–415, 2004
Ruiz-Razura A, Mentz H, Patronella C, Newall G: Gynecomastia: Breast tissue removal through a single puncture incision. Poster presentation. Aesthetic Meeting 2004, ASAPS/ASERF, Vancouver, Canada, April 15–21, 2004
Saad MN, Kay S: The circumareolar incision: A useful incision for gynaecomastia. Ann R Coll Surg Engl 66:121–122, 1984
Simon BE, Hoffman S, Kahn S: Classification and surgical correction of gynaecomastia. Plast Reconstr Surg 51:48, 1973
Spence RW, Celestein LR: Gynaecomastia associated with cimetidine. Gut 20:154–157, 1979
Tashkandi M, Al-Qattan MM, Hassanain JM, Hawary MB, Sultan M: The surgical management of high-grade gynecomastia. Ann Plast Surg 53:17–20, discussion 21, 2004
Wallace AM: Gynecomastia. In: Evans GRD (ed) Operative plastic surgery. McGraw-Hill: New York, pp. 686–697, 2000
Acknowledgment.
None of the authors had any financial interest or received any grants or outside funding for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a scientific poster at the Annual Meeting of the American Society of Aesthetic Plastic Surgery, The Aesthetic Meeting 2004, ASAPS/ASERF, Vancouver, Canada, 15–21 April 2004.
Rights and permissions
About this article
Cite this article
Mentz, H.A., Ruiz-Razura, A., Newall, G. et al. Correction of Gynecomastia Through a Single Puncture Incision. Aesth Plast Surg 31, 244–249 (2007). https://doi.org/10.1007/s00266-006-0180-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-006-0180-y