Abstract
Background
Recent studies have provided diverging results regarding the factors that may affect sensibility after primary breast augmentation. Implant volume is believed to be an important factor, but the relation of implant size to breast volume has not been adequately addressed. In addition, the literature shows that a conflict exists when the periareolar and inframammary approaches are compared. This study aimed to refine the volumetric analysis comparing the implant and final breast size as well as the intrinsic association of these two factors with postoperative sensory alteration of the breast.
Methods
A prospective study investigated patients who underwent aesthetic breast augmentation between June 2004 and October 2005 (i.e., a 16-month period) at the Ivo Pitanguy Institute. The sensibility in nine regions of the breast was tested before and after surgery using Semmes-Weinstein monofilaments. Breast sizers were used to compare the pre- and postoperative breast volumes. Statistical analysis of the data took into consideration the relative volume of the implant, the surgical approach, the presence of minor complications, the breast-feeding history, and the subjective evaluation of sensory changes in the patients.
Results
A total of 37 patients who underwent breast augmentation were examined preoperatively. The relative volume of the implant was found to be associated with sensibility alterations. No difference was found between the periareolar and inframammary incision approaches. Other factors such as previous breast-feeding, minor complications, and subjective alterations were not associated with sensory alterations.
Conclusions
The study findings suggest that larger implants and smaller breasts show an increased association with postoperative sensory alterations of the breast. Plastic surgeons and their patients should be aware of this possibility. Implant volume should be considered together with breast size to avoid sensory complications, and this is summarized in the concept of relative volume.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast augmentation is one of the most common cosmetic plastic surgery procedures performed worldwide, with more than 290,000 surgeries performed during 2005 in the United States alone [1]. Over the years, evolutions in operative technique (incision selection, different planes of dissection) and improvements in implant variables (volume, shape, surface texture, and filler type) have led to excellent results with minimal complications.
Despite the increasing popularity of breast augmentation, some patients experience sensory changes after the procedure, with the incidence estimated to be as high as 41% [2]. Alterations in breast sensibility seem to be the second most common patient complaint after breast augmentation, after capsular contracture [3].
Earlier studies performed to evaluate postoperative sensory changes used imprecise measurements such as light finger touch or pinprick [4]. The sensibility level could not be precisely quantified using these crude methods. Recent studies evaluating sensibility changes use the Semmes-Weinstein monofilament test to assess the pressure threshold [5,6]. Other methods, such as measuring static and moving two-point discrimination, have proved to be unreliable and inconsistent [7]. Although some newer studies use a pressure-specified sensory device [8,9], the clinical relevance of such methods is still unclear [10].
The use of the Semmes-Weinstein monofilaments remains a simple, clinically applicable, and objective method [10,11]. The perception of monofilaments involves an expression of touch, pressure, and pain [10], which makes the monofilaments suitable for our purpose.
The anatomy of the female breast innervation has been well described. The breast receives sensory fibers from the second to the sixth intercostal nerves, with the upper breast skin innervated by supraclavicular nerves from the third and fourth branches of the cervical plexus. Each intercostal nerve divides itself into an anterior cutaneous branch (supplying the medial aspect of the breast) and a lateral cutaneous branch (innervating the lateral aspect of the breast). Most authors agree that the sensory innervation of the nipple–areola complex (NAC) is provided primarily by the fourth intercostal nerve, but that the third and fifth intercostal nerves participate as well [10,11], and even the second [10] in some cases. These various nerve branches converge into the NAC, providing breast skin sensation.
The implants all were placed through the following incisional approachs: the periareolar approach, the inframammary approach, and the transareolar (or Pitanguy incision) approach.
This study aimed to investigate the factors that affect the sensation of breast skin after subglandular implant placement. The analyzed variables included the relative volume of the implant, the surgical approach (inframammary, periareolar, or transareolar incision), the previous lactation, the role of minor complications, and the patients’ subjective perception of sensibility alterations.
Patients and Methods
A prospective study investigated patients who underwent aesthetic breast augmentation between June 2004 and October 2005 at the 38th Ward of the Santa Casa General Hospital of Rio de Janeiro (the Ivo Pitanguy Institute). Breast sensibility was tested before and after surgery using Semmes-Weinstein monofilaments. Breast sizers 10 was used to compare the pre- and postoperative breast volumes. No financial or other compensation was provided for the patients enrolled in the study.
The exclusion criteria specified medical conditions that could affect sensory functions (neurologic, endocrine, nutritional, metabolic, or hematologic abnormalities; collagen or autoimmune diseases), previous breast surgery (including biopsy), and altered mammography or breast sonography images. Patients scheduled to receive submuscular implants also were excluded from this protocol.
Sensory Testing
Skin sensation was tested preoperatively using Semmes-Weinstein monofilaments, which consist of nylon filaments applied perpendicularly to the breast skin. With the patient seated comfortably in a room temperature environment, each monofilament was tested over nine points on each breast while the patient kept her eyes closed. The locations of these nine points were established as in previous sensibility studies [5,6]: one on the nipple, one on each of the four areola quadrants, and one on each of the four breast skin quadrants. The tactile thresholds were defined as the minimal bending force of the thinnest filament sensed by the patient. After three attempts, one single affirmative response determined a positive result for each of the nine points.
The kit of six monofilaments was labeled from 1.69 to 5.47. These values represent the logarithm of 10 in the base of the force in milligrams required to bend the nylon monofilament. The same test performed preoperatively was repeated 6 months postoperatively. As shown in previous sensibility studies [5,9], sensory losses tend to stabilize after this period and normally show no significant improvement after 6 months.
Breast Volume Assessment
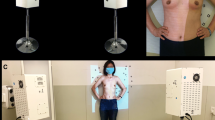
Breast volume was measured preoperatively and 6 months after surgery using a set of seven breast sizers [17] (transparent plastic molds used under the bra to simulate the breast size after breast augmentation, intended to help in planning of the implant size). These breast sizers have volumes measuring from 120 to 660 ml. Each sizer is held by the patient so as to fit exactly the breast surface.
The sizers were applied over the breast with the patient seated in an upright position (Fig. 1). The patient chose the one mold that best simulated the final breast volume she desired.
Other Examined Factors
In a postoperative patient questionnaire, symptoms such as pain, tenderness, and paresthesis were recorded for each breast. Patients were asked about their subjective perception of sensibility changes. Local complications (seroma, hematoma, or partial wound dehiscence) also were registered for each breast.
Statistical Analysis
The results of the sensory testing were classified in a qualitative fashion in two groups: group 1 (patients with unaltered postoperative sensibility) and group 2 (patients with altered postoperative sensibility). To verify the association among the variables of interest, statistical analysis was performed using a chi-square test at a significance level (α) of 0.05. The analyzed variables included the relative volume of the implant (i.e., an index defined by the quotient resulting from the implant volume divided by the preoperative breast size), the incision approach (transareolar, periareolar, or inframammary), the presence of minor complications, the breast-feeding history, and the subjective perception of sensibility alterations.
Results
A total of 37 healthy women scheduled for elective aesthetic breast augmentation agreed to participate in this study. All the patients were examined before surgery and scheduled to be reexamined 6 months after the operation. Eight patients did not return for medical consultation in the 6th month after surgery. Our final sample therefore consisted of 29 patients (58 breasts) with mean age of 33 years. Two of these patients had undergone previous unilateral biopsies, thus excluding 2 breasts from our study, for a final sample of 56 breasts. The features of our population sample are summarized in Table 1. Of the 56 breasts, 40 (71%) had previously been submitted to breast-feeding.
All the breasts received silicone gel-filled implants. The periareolar approach was used for 31 breasts (55.3%), the inframammary approach for 17 breasts (30.3%), and the transareolar approach for 8 breasts (14.3%). Nine breasts (16%) presented minor complications: partial wound dehiscence in 6 breasts, seromas in 5 breasts, dehiscence with seroma drainage in 1 breasts, and hematoma in 1 breast. None of the breasts showed capsular contracture by the time of reexamination.
Subjective Perception
Subjective complaints were reported for 21 breasts (37.5%). Among these, the main complaint was paresthesia (14 breasts, 66.6%), followed by allodynia (3 breasts, 14.2%). For the remaining four breasts (19%), the patients complained of sensory alterations but could not specify their symptoms based on our questionnaire. No patient reported spontaneous pain after 6 months of follow-up evaluation.
Objective Alterations
Objective alterations were observed for 18 breasts (32.1%), with sensibility loss demonstrated by higher postoperative tactile thresholds in examination with the Semmes-Weinstein monofilaments. In this subset of breasts, the most affected region was the NAC. Objective alterations in the inferior region of the areola were observed with all 18 breasts (100%). Among the four regions of the breast skin, the lower (i.e., the “6 o’clock” point) also was the most affected (Table 2).
Variables Associated with Sensibility Alterations
With regard to the different surgical approaches, no difference could be found between the periareolar and the inframammary incisions. The number of breasts with a transareolar incision (n = 8) was too small to allow a valid statistical comparison.
The relative volume of the implant was found to have a positive association with sensibility alterations. Higher values of this index (i.e., larger implants or smaller breasts) were associated with higher postoperative sensibility thresholds (p < 0.05). No association between the presence of minor complications and sensibility alterations was found. The patient breast-feeding history showed no statistical relation with sensory changes. Patients who claimed to have subjective alterations were not associated with a higher incidence of objective alterations than patients who had no subjective complaints (Table 3).
Discussion
After augmentation mammaplasty, many factors are involved in sensory alterations. Endogenous conditions such as previous breast-feeding cannot be altered by the surgeon, but our findings suggest that this plays a minor role in sensory changes. Complications may appear, as with any other surgical procedure, but such events (seroma, partial wound dehiscence, or hematomas) are not likely to interfere with sensory outcomes, as the results of this study demonstrate.
The information gathered in our study suggests that subjective perception of sensibility changes is not associated with objective alterations, although the former is more frequent. The patient’s subjective perception is undoubtedly an important factor to be considered, but this evaluation is beyond the scope of this study. After all, for the majority of patients, the satisfaction with improvement in body contour and self-image greatly outweighs the experienced sensory alterations [2,3,18].
In practical terms, the surgeon must limit the possible factors for sensory alteration to the technical aspects of the surgical procedure: incision selection, choice of plane for implant placement, and size of the implant to be used. These are the variables that can be modified by the surgeon in accordance with the desires, expectations, and possibilities of the patient.
Distinct surgical approaches to avoid sensory loss are advocated by different authors. On the basis of anatomic studies, Farina et al. [15] state that the fourth intercostal nerve reaches the left mammary gland at the 4 o’clock position and the right gland at the 8 o’clock position, thus supporting a medialized periareolar incision. This approach also was defended by Spear [19].
On the other hand, Schlenz et al. [14] report that medialized periareolar incisions increase the risk of nerve damage. After extensive anatomic dissections, Schlenz concluded that the main source of innervation for the NAC, the nerve fibers of the anterior cutaneous branch, presents a more superficial course within the subcutaneous tissue to reach the medial areolar edge. Accordingly, these nerves are best protected if incisions on the medial border of the areola are avoided.
Pitanguy [20] advocates the transareolar incision. Because the innervation shows a constant centripetal pattern, this approach would lower the risk of nerve lesions. Jaspars et al. [16], describing the lack of a consistent anatomic nerve distribution, suggest that a vertical approach (from a cranial or caudal direction) to the NAC would minimize the chance of nerve injury. More recently, Okwueze et al. [8] concluded that the periareolar incision produces less sensory loss than the inframammary incision.
Our study compared the periareolar approach with the inframammary approach and found no difference in terms of objective sensibility alterations. These findings agree with those presented by the pioneer work of Courtiss and Goldwyn [4], and more recently with those published in the study of Mofid et al. [9], which showed no difference in sensory outcomes among different incision approaches. This valuable information can help plastic surgeons and their patients in deciding whether a periareolar or inframammary approach would be more suitable.
As for the plane choice, submuscular placement is thought to minimize nerve damage [18,19], although some authors claim that there is no reason to presume that implant position, either subglandular or submuscular, should affect sensory innervation [9,18]. Notwithstanding this controversy, all the patients included in our study had their implants placed in a subglandular plane. Dissection was performed under direct vision (with the use of fiberoptic-assisted illumination) using both scalpel and blunt dissection. The pocket of undermining was large enough to accommodate the implants well without risk of creating creases and contour irregularities.
Based on the information provided in our study, implant size seems to play an important role in determining sensory changes. This was first pointed out by the studies mentioned earlier [4,9]. Because the implant volume determines the size of the pocket to be undermined, the risk of nerve lesion is greater with more extensive dissections, especially those in the lower quadrants of the breast [5]. The same size pocket undermined in a medium-sized breast with no final sensory alteration can presumably produce a permanent sensory impairment in a small-sized breast, caused by nerve section (neurotmesis) during the undermining.
In addition, sensory alterations may be caused by neurapraxis of the nerve fibers, due to excessive tension, if the implant is placed under a relatively small breast [9]. Other factors, such as the alleged higher innervation density of small breasts [6], may contribute to more noticeable sensory alterations in patients with smaller breasts.
In the view of the cited authors, the relative volume (implant volume divided by preoperative breast size) adequately corrects this analytical distortion. Higher values of this index are associated with an increased postoperative sensibility threshold, suggesting greater sensibility loss. For statistical inference purposes, however, our sample was not large enough to establish a maximum security limit for such an index (i.e., a value above which the procedure would be associated with prohibitive rates of sensory losses).
The concept of relative volume should not be regarded merely as a mathematical finding. Rather, it emphasizes the implications of choosing larger implants, especially for small-breasted women. The possible sensory complications that may arise from this choice should always be explained to the patient and discussed before surgery. The information provided in our study suggests that larger implants or smaller breasts show an increased association with postoperative sensory alterations, and plastic surgeons and their patients should be aware of this possibility.
References
Information provided in the official ASPS site, this information from the American Society of Plastic Surgeons is currently available at the same electronic address online. Retrieved May 12, 2006 at http://www.plasticsurgery.org/public_education/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=17890. American Society of Plastic Surgery
Fiala TGS, Lee WPA, May JW: Augmentation mammaplasty: Results of a patient survey. Ann Plast Surg 30:503, 1993
Hetter GP: Satisfactions and dissatisfactions of patients with augmentation mammaplasty. Plast Reconstr Surg 64:151, 1979
Courtiss EH, Goldwyn RM: Breast sensation before and after plastic surgery. Plast Reconstr Surg 58:1, 1976
Schlenz I, Rigel S, Schemper ME, Kuzbari R: Alteration of nipple and areola sensitivity by reduction mammaplasty: A prospective comparison of five techniques. Plast Reconstr Surg 115:743, 2005
Mofid M, Dellon L, Elias J, Nahabedian M: Quantification of breast sensibility following reduction mammaplasty: A comparison of inferior and medial pedicle techniques. Plast Reconstr Surg 109:2283, 2002
Terzis JK, Vincent MP, Wilkins LM, Rutledge K, Deane LM: Breast sensibility: A neurophysiological appraisal in the normal breast. Ann Plast Surg 19:318, 1987
Okwueze MI, Spear ME, Zwyghuizen AM, Braun SA, Ajmal N, Nanney LB, Hagan KF, Wolfort SF, Shack RB: Effect of augmentation mammaplasty on breast sensation. Plast Reconstr Surg 117:73, 2006
Mofid M, MD, Klatsky S, MD, Singh N, Nahabedian M, MD: Nipple–areola complex sensitivity after primary breast augmentation: A comparison of periareolar and inframammary incision approaches. Plast Reconstr Surg117:1694, 2006
Nahabedian MY: Effect of augmentation mammaplasty on breast sensation: Discussion. Plast Reconstr Surg 117:84, 2006
Tairych GV, Kuzbari R, Rigel S, Todoroff BP, Schneider B, Deutinger M: Normal cutaneous sensibility of the breast. Plast Reconstr Surg 102:701, 1998
Gonzalez F, Brown F, Gold M, Walton R, Shafer B: Preoperative and postoperative nipple–areola sensibility in patients undergoing reduction mammaplasty. Plast Reconstr Surg 92:809, 1993
Benediktsson KP, Perbeck L, Geigant E, Solders G: Touch sensibility in the breast after subcutaneous and immediate reconstruction with a prosthesis. Br J Plast Surg 50:443, 1997
Schlenz I, Kuzbari R, Gruber H, Holle J: The sensitivity of the nipple–areola complex: An anatomic study. Plast Reconstr Surg 105:905, 2000
Farina MA, Newby BG, Alani HM: Innervation of the nipple–areola complex. Plast Reconstr Surg 66:497, 1980
Jaspars J, Posma A, Van Immerseel A, Gittenberger-de-Groot A: The cutaneous innervation of the female breast and nipple–areola complex: Implications for surgery. Br J Plast Surg 50:249, 1997
França AL, Scevola MC, Fachin SD, França PF, França NC: Mamasize: A new auxiliary instrument in the planning of enlargement mammaplasty (Mamasize: um novo instrumento auxiliar no planejamento das mamoplastias). Rev Soc Bras Cir Plas 20:204, 2005
Young VL, Nemecek JR, Nemecek DA: The efficacy of breast augmentation: Breast size increase, patient satisfaction, and psychological effects. Plast Reconstr Surg 94:958, 1994
Spear SL, Matsuba H, Little J III: The medial periareolar approach to submuscular augmentation mammaplasty under local anesthesia. Plast Reconstr Surg 84:599, 1989
Pitanguy I: Transareolar incision for augmentation mammaplasty. Aesth Plast Surg 2:363, 1978
Tebbets JB: Transaxillary subpectoral augmentation mammaplasty: Long-term follow-up and refinements. Plast Reconstr Surg 74:497, 1980
Banbury J, Yetman R, Lucas A, et al. Prospective analysis of the outcome of subpectoral breast augmentation: Sensory changes, muscle function, and body image. Plast Reconstr Surg 113:701, 2004
Sarhadi N, Dunn J, Lee F, Soutar D: An anatomical study of the nerve supply of the breast, including the nipple and areola. Br J Plast Surg 49:156, 1996
Acknowledgment
The authors express their gratitude to Mr. Clayton Amaral Domingues, PhD., for his expertise in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pitanguy, I., Vaena, M., Radwanski, H.N. et al. Relative Implant Volume and Sensibility Alterations After Breast Augmentation. Aesth Plast Surg 31, 238–243 (2007). https://doi.org/10.1007/s00266-006-0173-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-006-0173-x