Abstract
Capsular contracture is the most unpredictable complication after mammary augmentation. It presents an uncertain evolution, and is one of the most difficulty complications to treat. Evaluation of this condition usually was relegated to the surgeon’s judgment, but currently there are three methods for measuring capsular contracture: palpation, applanation tonometry, and measure of mammary compliance. A prospective study was conducted to evaluate the different methods for managing capsular contracture. Particular attention was paid to the measure mammary compliance with a new device: the Anton Paar Mammacompliance system. This study found a good match between clinical and objective measurements, and also between the measure of applanation tonometry and the measure of mammary compliance. The Anton Paar Mammacompliance system seems to be effective in eliminating the descriptive part and keeping to the measurements and objective data. It is easily reproducible in the various check ups. It permits objective assessment for the measure of capsular contracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In recent years augmentation mammaplasty has been one of the most common surgical procedures performed by plastic and reconstructive surgeons. An estimated 10 to 12 million women in the world have had breast implants, attesting to the pervasiveness of societal attitudes favoring the use of these devices for breast enlargement [5].
Unfortunately agumentation mammaplasty is not free of complications, and capsular contracture, the most unpredictable complication, presents an uncertain evolution and is the most difficult to treat after mammary augmentation. The literature to date is extremely variable, and reported rates of capsular contracture range from 0.5% to 20% [1, 6]. The variability of the reported rate for capsular contracture certainly depends on many factors, but it is particularly related to the time from the surgery, the percentage of the patients monitored, and the type of implant used. More than this, the evaluation of capsular contracture is related to surgeon’s judgment, breast condition, and other numerous factors. Evaluation of the capsular contracture rate can be very important not only for scientific purposes, but also for its medicolegal implications. For this reason, methods for standardizing the procedure have been described. The current methods described to measure capsular contracture are basically three: palpation, applanation tonometry and measurement of mammary compliance [2, 3, 4, 7, 8, 9, 10, 11, 12, 13, 14].
Palpation is a clinical evaluation that divides the clinical cases in four groups. The first group consists of the patients who present with normal inspection and palpation result. The consistency is the same as with a breast that has had no surgery. For the second group, the breast examination results are normal, but the palpation is not normal. The implant is palpable, but it is not visible, and the consistency of the breast is increased. For the third group, both the examination and the palpation are abnormal. The breast is hard, and the prosthesis is easily palpable and visible. The fourth group consists of patients who report mammary tension and mastalgia. The implant and overlying skin are evident [2, 3].
Applanation tonometry measures the intramammary pressure. This technique, derived from the Goldman’s technique for the measurement of intraocular pressure, was described by Moree in 1979 [12]. It is based on the application of a force (F) to the breast, measurement of the contact area (A), and subsequent calculation of the intramammary pressure according to the following formula:
The tonometer is made up of a transparent disc with a diameter of 20.3cm and a weight of 213 g. Applied to the breast it exerts a force that squashes the breast. The breast, over which a normal-colored ecograph gel has been applied, leaves an imprint on the tonometer. This imprint is transferred to a sheet of filter paper, from which the contact area is calculated. The force applied is attributable to the weigh of the tonometer and the acceleration of gravity (9.8 m/sec2). The area, which may be circular or ellipsoidal, is calculated by measuring the zone of contact with the filter paper according to a comparison of paper and millimeter markings. When the applied force and the area of contact are known, it is possible to obtain the intramammary pressure. Because a pressure of 98.1 is required to elevate a column of water (H2O) by 1 cm, the intramammary pressure can be expressed as cm H2O [7, 8, 12].
Mammary compliance, developed from the caliber of Burkhardt et al. [4], measures mammary compressibility. The instrument is placed at a level between the areola and the inframammary fold to measure the maximum diameter. Then a compression is performed to obtain the minimum diameter. The measure of the compressibility is obtained by calculating the difference between the two measurement. The system has been improved by Hoflehner [11], who measured the distance between the two sensors when a known force, was applied, obtaining a measurement according the following formula:
where DX represents the applied force, and the mammary diameter is that measured on the detector’s point of contact [10, 11, 14].
We conducted a prospective study to evaluate capsular contracture in a series of patients who underwent mammary augmentation over the last 2 years. We assessed the grade of capsular contracture with the different methods, particularly measuring mammary compliance with a new device: the Antoon Paar Mammacompliance system.
Materials and Methods
From January 2000 until this writing, we considered 120 implants applied to 60 patients in the Department of Plastic Surgery at the University of Rome La Sapienza. The indications for the surgery included augmentation mastoplasty for 34 patients, and mammary asymmetry for the other 26 patients. The age of the patients ranged from 20 to 42 years (mean, 33 years and 8 months; median, 30 years).
In 60 cases, the implanted device was anatomic and filled with cohesive silicone gel, and in the other 60 cases, round double-lumen implants filled with silicone gel and saline solution were used. All the implants had a textured shell, and the size ranged from 165 to 390 g for the anatomic implants and from 200 to 400 ml for the round double-lumen implants. For all the cases, the inframammary approach was used and the implant was inserted into a retromammary pocket.
Follow-up visits were scheduled at 1, 4, and 12 months after the surgical procedure. Capsular contracture was evaluated using palpation, applanation tonometry, and measurement of mammary compliance with the Antoon Paar Mammacompliance system. Clinical evaluation was performed by three different operators, and all the cases with discrepancies in the staging were recorded.
The Antoon Paar Mammacompliance system measures the distance between two sensors of the instrument when a known force is applied. A sedentary patient is subjected to breast constriction, which then is measured with the appropriate instrument. The measurement is started when a base value of 0.5 is achieved and ended when a value of exceeding 15 N is obtained. The diameter of the breast is measured when a forces of 0.5 N and 15 N are applied. Such measurements are used to calculate the mammary compliance according to the following formula:
where d15 is the mammary compliance and d15 and d0 represent the mammary diameter measured in millimeters with respective forces of 15 and 0.5 N.
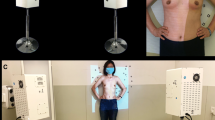
The measurement is performed for each breast in eight positions, and the arithmetic mean of the various measurements is calculated. All the work is done by computer, which can indicate the compliance value as a numeric value or as a diagram of the compliance showing the softness of the breast (Figs. 1 and 2).
Results
We have found a good match between clinical and objective measurements and also between the measures of applanation tonometry and mammary compliance.
According Baker’s method of palpation at the 4-month follow-up visit, capsular contracture was grade 1 in 45 cases (37.5%). In these cases, the mean value of mammary compliance was 38.7, and the mean value of mammary pressure, as measured with applanation tonometry, was 5.3 cm of H2O. In 54 cases, (45%) we observed a grade 2 capsular contracture. In these cases, the mean value of mammary compliance was 48.1, and the mean value of mammary pressure, as measured with applanation tonometry, was 6.7 cm of H2O. In 21 cases (17.5%) we observed a grade 3 capsular contracture. In these cases, the mean value of mammary compliance was 56.1, and the mean value of mammary pressure, as measured with applanation tonometry, was 8.1 cm of H2O.
At the 1 year follow-up visit, capsular contracture was grade 1 in 40 cases (33.3 %). In these cases, the mean value of mammary compliance was 38.9, and the mean value of mammary pressure, as measured with applanation tonometry, was 5.2 cm of H2O. In 52 cases (43.3%), we observed grade 2 capsular contracture. In these cases, the mean value of mammary compliance was 48.4, and the mean value of mammary pressure, as measured with applanation tonometry, was 6.8 cm of H2O. In 19 cases (15.8%), we observed a grade 3 capsular contracture. In these cases, the mean value of mammary compliance was 57.3, and the mean value of mammary pressure, as measured with applanation tonometry, was 8.3 cm of H2O. In 9 cases (7.6%), we observed a grade 4 capsular contracture. In these cases, the mean value of mammary compliance was 64.5, and the mean value of mammary pressure, as measured with applanation tonometry was 10.2 cm of H2O.
From our data, we observed that the value of mammary compliance was from 29.2 to 44.1 (mean, 38.8) in the cases with grade 1 capsular contracture, as determined according Baker’s method of palpation. In the cases with grade 2 capsular contracture, the value of mammary compliance ranged from 40.1 to 52.2 (mean, 48.2). In the cases with grade 3 capsular contracture, the value of mammary compliance ranged from 48.6 to 61.9 (mean, 56.7). In the cases with grade 4 capsular contracture, the value of mammary compliance ranged from 55.3 to 75.8 (mean, 65.4)
Interestingly, 18 cases (15%) were clinically difficult to score, and they showed a borderline measure of capsular contracture according Baker’s classification.
Discussion
Although the system we used to measure of capsular contracture, and mammary compliance is in a preliminary phase, it seems to give reliable results. This type of system seems to be effective in its attempt to eliminate the descriptive part and keep to measurements and objective data. It is easily reproducible in the various checkups.
The data from our series show that is possible to find a good match between the values for mammary compliance and applanation tonometry and that for clinical evaluation such as Baker’s method of palpation.
The measurement of capsular contracture by palpation according to Baker’s method uses a system that is largely dependent on the experience and sensitivity of the operator. If only skin with little adipose and glandular tissue cover the implant, the capsule may be visible even though the breast may show no evidence of firmness. Such a case would be classified as Baker 1 because it is completely soft or Baker 3 because the capsule is visible. Similar difficulties arise when a thick layer of soft tissue covers the implant. The capsule may be very firm and still look absolutely natural. A different assessment also may result if a different position is assumed by the patient. If the arms are raised over the head, the capsule seems to be more contracted than when the arms are pending. When the patient bends forward from the waist, the tensile forces exerted on the breast may show the capsule in the lateral section even if the breast shows no signs of firmness [11].
A further disadvantage of Baker’s classification is that the result can neither be reproduced nor documented. On the contrary, applanation tonometry and especially the measurement of mammary compliance are easy to perform and dependent only to a limited extent on the operator. They therefore are easily reproducible [10, 11].
Applanation tonometry is based on the same principle as the method developed by Goldman [12] to measure internal eye pressure. Larger contact areas indicate a soft breast, whereas smaller contact areas point to a firm breast. To date, however, the use of this technique has not become widespread because the contact area also is influenced to a larger extent by the size of the breast and lateral slipping depends on the thickness and firmness of the subcutaneous tissue and the shape of the thorax [7, 8].
The method of Burkhardt et al. [4] is well suited to excluding possible sources of error and permitting objective and recordable measurements. Because the sensors are small, only slight pressure is necessary to impress the soft tissue. The thickness of the soft tissue layer that covers the implants is thus negligible [4, 10, 11].
The Anton Paar Mammacompliance system evolved from the Burkhardt method. It is simple to use, and its graphs are easy to understand. All the work is done by the computer. The results may be either recorded or stored directly into a computer by an analog data acquisition interface. In either case, it is possible to evaluate the graphs and store them for subsequent comparisons. Because of their great sensitivity, compliance measurement is suited to long-term follow-up studies and close monitoring of therapeutic concepts. Great importance is attributed to the graphs because they may show the severity of the capsular contracture. The graph with a curvilinear aspect shows a mild capsular contracture, whereas the graph with a rectilinear aspect shows a severe capsular contracture (Figs. 1 and 2).
As the current data shows, this method is influenced by the type of the mammary prostheses used. In fact, the mammary compliance in this study appeared higher in the patients who had a cohesive gel-filled anatomic implant than in the patients who had a round double-lumen implant filled with silicone gel and saline solution.
Compliance measurement is an objective method for measuring and classifying capsular contracture. The measurements can be reproduced and documented. The refer, the measurement of mammary compliance can be very important for scientific purposes and also for its medico-legal implications.
References
C Alfano M Costantini M Mazzocchi (1999) ArticleTitleClinical examination and follow-up of mammary implants Eur Plast, Surg Rev 4 4–8
Baker JL: Classification of spherical contractures. Read at the Aesthetic Breast Symposium, Scottsdale, Arizona
JL Baker (1978) Augmentation mammoplasty JQ Owsley R Peterson (Eds) Symposium on aesthetic surgery of the breast Mosby St Louis 125–152
B.R Burkhardt PL Schhnur JJ Tofield PD Dempsey (1982) ArticleTitleAn objective clinical assessment of fibrosus capsular contracture Plast Reconstr Surg 69 794–799 Occurrence Handle1:STN:280:Bi2C2svpvFI%3D Occurrence Handle7071224
MA Codner AT Cohen TR Hester (2001) ArticleTitleComplication in breast augmentation: prevention and correction Clin Plast Surg 28 587–596 Occurrence Handle1:STN:280:DC%2BD38%2FitlKmsw%3D%3D Occurrence Handle11471964
M Eisenmann-Klein (1999) ArticleTitleBreast implants: the past, the present, the future Eur. Plast Surg Rev 3 33–43
LO Gylbert (1989) ArticleTitleApplanation tonometry for the evaluation of breast compressibility Scand J Plast Reconstr Surg Hand Surg 23 223–229 Occurrence Handle1:STN:280:By%2BC2c%2FlslI%3D Occurrence Handle2617224
LO Gylbert (1989) ArticleTitleConstant compression caliper for objective measurement of breast capsular contracture Scand J Plast Reconstr Surg Hand Surg 23 137–142 Occurrence Handle1:STN:280:By%2BD2cbgtFY%3D Occurrence Handle2814382
H Hayes SuffixJr P McLeod (1979) ArticleTitleIndentation tonometry of the breasts Plast Reconstr Surg 63 13–21 Occurrence Handle432321
H Hoflehner G Pierer (1994) ArticleTitleSubjective and objective assessment of capsular contracture Eur J Plast Surg 17 69–74
H. Hoflehner G. Pierer P Rehak (1993) ArticleTitleMammary compliance, an objective technique for measuring capsular fibrosis Plast Reconstr Surg 80 1078–1084
JR Moore (1979) ArticleTitleApplanation tonometry of breasts Plast Reconstr Surg 63 9–12 Occurrence Handle1:STN:280:CSaC2MfltVU%3D Occurrence Handle432328
JW Mulder JPA Nicolai (1990) ArticleTitleBreast tonometry: a practical device for accurate measurement of capsule formation Eur J Plast Surg 13 274–282
PH Rehak H Glanzer (1994) ArticleTitle“Mammary compliance transmitter,” a novel instrument for the objective measurement of the degree of capsular fibrosis following breast prosthesis implantation Phy Med Biol 39a IssueIDpart 2 574–581
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alfano, C., Mazzocchi, M. & Scuderi, N. Mammary Compliance: An Objective Measurement of Capsular Contracture. Aesth. Plast. Surg. 28, 75–79 (2004). https://doi.org/10.1007/s00266-004-4005-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-004-4005-6