Abstract
Among concerned nasal appearances, a deformity with supero-lateral displacement of the nostril rim, called retracted nostril rim or elevated nostril rim is commonly seen and is considered one of the most difficult types of cases to treat aesthetically. A new surgical method for treating retracted nostril rim was performed in 10 patients, using the combination of auricular composite graft, internal fixation with a retainer, and external continuing suspension with anchoring sutures. The procedure was successful in maintaining the grafted cartilage in the ideal position and in avoiding recurrence of retraction or elevation of the constructed alar rim. The presented method merits consideration as a standard operative approach for correction of retracted nostril rim.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The shape of the nostril rim is a sensitive topic, especially among women. Retracted or elevated (supero-lateral displacement) nostril rim occurs congenitally, or iatrogenically due to scar contracture after various kinds of rhinoplasty. Gunter et al. [1] previously suggested a definition of retracted ala as a deformity characterized by an alar rim to nostril long axis distance of more than 2 mm. Retracted alar rims make the nostrils appear too big, and nasal hair be seen from oblique and lateral views. As for the unilateral cases, the most common complaint is a marked difference in the size and shape of the nostril rim. Morphologically, retracted nostril rims can be classified into two types: Type I includes those cases where the nostril rim is completely displaced supero-laterally, and the nasal cavity can be seen from the frontal view. Type II includes those cases where part of the nostril rim is supero-laterally displaced and appears to be notched. Type I occurs congenitally and is usually bilateral, whereas type II occurs both congenitally and iatrogenically, and iatrogenic cases involve usually only one side.
Although retracted nostril rims are seen frequently, and there have been several surgical techniques and modifications for it, it is still considered one of the most difficult nasal deformities to treat. Meyer and Kesselring [2] introduced a method for lowering the alar rim with a graft of alar cartilage strip, and Ellenbogen [3] modified the method as a combined technique with a local skin flap and a cartilage graft (septal, lower lateral, or auricular). Ellenbogen’s method, however, left a raw surface on the internal mucosa, which could lead to postoperative complications such as distortion, retraction, and protrusion of the grafted cartilage. Guyuron [4] used an internal V-to-Y advancement with or without a cartilage graft for the severe alar retraction, and Rohrich et al. [5] utilized alar contour grafting with septal cartilage. Constantian [6] used Sheen and Sheen’s method [7] with minor modifications and showed relatively successful results by using skin and cartilage composite grafts harvested mainly from the auricle for secondary or tertiary rhinoplasty. Based on our experiences, insufficient improvements or postoperative retractions can be seen, especially in severe cases of retracted alar rim deformity or in the cases with scarring.
The authors modified the previously mentioned methods to avoid postoperative retraction of the nostril rim by combining auricular composite grafts and postoperative anchoring suspension.
Subjects
A total of 10 patients, including nine females and one male, were treated with the present method. The age of the patients ranged from 21 to 44 years (mean ± SD: 32.2 ± 7.0). All six bilateral cases did not have any history of rhinoplasty, whereas four unilateral cases were composed of two congenital cases and two iatrogenic cases. Eight congenital cases were composed of five Type I cases and three Type II cases, whereas two iatrogenic cases showed Type II deformity. The follow-up periods ranged from 5 to 20 months. The summarized data are shown in Table 1.
Surgical Technique
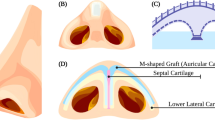
First, an auricular cartilage and its adherent anterior skin is harvested from the posterior conchal wall as a composite graft (Fig. 1A). For bilateral cases, the combined skin and cartilage grafts are harvested from the anterior surface of both auricles, whereas for the unilateral cases it is harvested from a single side. The skin defect is closed with 7-0-nylon, and the cartilage defect is left as it is.
Surgical procedure. (A) The donor site of the auricular composite graft. Two 7-0 nylon sutures for anchoring suspension were passed through the lateral end of the cartilage. (B--D) Cross-sectional views of the nasal ala. (E) The composite graft was sutured to the recipient site and the anchoring sutures were passed out through the nostril rim skin. (F) The reconstructed ala was fixed with an internal retainer and an external cast on which the anchoring sutures were fixed with taping.
The combined skin and cartilage graft is trimmed and fabricated to match the preoperative design of the recipient site. The cartilage is shaved to about one-half its original thickness to avoid postoperative bulky appearance of nasal ala. After completion of the fabrication, two 7-0-nylon sutures for anchoring suspension are passed through the end of the cartilage on the side placed to the alar margin (Fig. 1A).
A little cephalic from the hair-bearing margin of the vestibular skin, a rim incision is made, followed by undermining in the caudal direction to form a skin pocket and unfurl the alar margin caudally (Fig. 1B, 1C). The free ends of the two 7-0-nylon anchoring sutures are passed out through the nostril rim skin for proper positioning and postoperative suspension of the auricular composite graft. Once positioned in the skin pocket, the composite graft is fixed with sutures followed by skin closure (Fig. 1E). In order to stabilize the graft, a nasal retainer is inserted into the nasal cavity followed by an external fixation with a plastic cast (Aquaplast® A962-54, Smith & Nephew Inc., Germantown, Wisconsin, USA). The final procedure is to fix the free ends of the 7-0 nylon sutures to the cast with tape (Micropore®, 3M, Minnesota, USA) to avoid cephalic displacement of the graft (Fig. 1D, 1F). The internal retainer and the external cast, as well as the anchoring sutures, are removed 1 week after surgery.
Cases
Case1
A 36-year old female patient presented with bilateral retracted nostril rim classified as Type I. The patient’s chief complaint was that the nasal cavity can be seen from the front (Fig. 2A). A combined skin and free composite cartilage graft was harvested from the anterior surface of both auricles with the dimension of 18 × 4 mm. The graft stabilized without any postoperative complications or problems. At 7 months, a natural configuration of the nostril rim was attained with symmetry and the patient was satisfied with the result. The nasal cavity was relatively concealed from the frontal view (Fig. 2B).
Case 2
A 21-year old female patient presented with bilateral retracted nostril rim classified as Type II. The preoperative frontal appearance revealed a notch-like configuration in the superior region of the nostril rim (Fig. 3A). The postoperative appearance at 5 months showed that the notch-like configuration had been sufficiently corrected and that a natural-looking configuration of the nostril rim had been attained (Fig. 3B).
Case 3
A 28-year old female patient presented with right unilateral retracted nostril rim classified as Type II. The preoperative frontal view showed asymmetry of the nostril rim, especially the notch-like configuration located in the superior region of the right nostril rim (Fig. 4A). A combined skin and free composite cartilage graft was harvested from the anterior surface of the right auricle. The right nostril rim was successfully corrected without any postoperative complications, and a natural-looking configuration of the right nostril rim and symmetry had been maintained at 15 months (Fig. 4B).
Results
In all 10 cases, improvement of the retraction and patient satisfaction were obtained with minimal variation. Postoperative recurrence of the deformity was not clearly detected during the follow-up periods ranging from 5 to 20 months. Bulkiness of the ala was seen in one case in which the auricular cartilage was not thinned. In two cases, localized focal necrosis of the skin cover of the cartilage graft was seen at 1 week after surgery, and yet the necrosis left no postoperative alar deformity.
Discussion
The nasal ala has a freed margin, and this is one of the reasons for difficulty in correcting alar deformity, suggesting the importance of postoperative fixation of the reconstructed ala during the healing period. The authors combined the auricular composite graft to the internal fixation with a nasal retainer and the external continuing suspension with anchoring sutures. For cast fixation, we used cast plastic with heat, but other materials, such as Denver Splint® (Shippert Medical Technologies, Eaglewood, Colorado, USA), can be used. Continuing suspension of the grafted cartilage greatly helps it to be maintained in the ideal position of the nasal ala. It also should be noted that the skin pocket of the recipient site is undermined in the caudal direction to construct a deep pocket, to obtain a tensility of the skin cover, and to allow for easy unfurling of the vestibular skin.
In our procedure, the composite graft was harvested from the anterior aspect of the auricle. This is because of the fact that the volume of the skin cover and subcutaneous soft tissue of the posterior surface is thicker in comparison to that of the anterior. If the composite graft taken from the posterior surface is used for the nostril rim, a bulky appearance is unavoidable. For the same purpose, the harvested cartilage is to be shaved to about one-half the original thickness. If the harvested cartilage is used in its original form, the cartilage is thick and hard, and it can be visible or felt at the external skin surface. In addition, when harvesting the composite graft, it is important to select an area of the auricle that closely resembles the curved configuration of the nostril rim, and thus we use the posterior wall of the concha.
Some of congenital bilateral type I cases are partly caused by the short nose, as suggested by Case 1. Although the present method does not improve the short nose, it can correct the large-looking appearance of the nostril frequently accompanying it.
Although further accumulation of cases is necessary, we believe that the presented method merits consideration as a standard operative approach for correction of retracted nostril rim.
References
JP Gunter RJ Rohrich RM Friedman (1996) ArticleTitleClassification and correction of alar-columellar discrepancies in rhinoplasty. Plast Reconstr Surg 97 643 Occurrence Handle10.1097/00006534-199603000-00026 Occurrence Handle1:STN:280:BymC2svpvVU%3D Occurrence Handle8596800
R Meyer UK Kesselring (1977) ArticleTitleSculpturing and reconstructive procedures in aesthetic and functional rhinoplasty. Clin Plast Surg 4 15 Occurrence Handle1:STN:280:CSiC28%2FovVM%3D Occurrence Handle852214
R Ellenbogen (1987) ArticleTitleAlar rim lowering. Plast Reconstr Surg 79 50 Occurrence Handle1:STN:280:BiiD1M3nsFI%3D Occurrence Handle3797517
B Guyuron (2001) ArticleTitleAlar rim deformities. Plast Reconstr Surg 107 856 Occurrence Handle10.1097/00006534-200103000-00032 Occurrence Handle1:STN:280:DC%2BD3M3jsFamtA%3D%3D Occurrence Handle11304615
RJ Rohrich J Raniere RY Ha (2002) ArticleTitleThe alar contour graft: correction and prevention of alar rim deformities in rhinoplasty. Plast Reconstr Surg 109 2495 Occurrence Handle10.1097/00006534-200206000-00050 Occurrence Handle12045582
MB Constantian (2002) ArticleTitleIndications and use of composite grafts in 100 consecutive secondary and tertiary rhinoplasty patients: introduction of the axial orientation. Plast Reconstr Surg 110 1116
JH Sheen AP Sheen (1987) Aesthetic Rhinoplasty, 2nd Ed. Mosby St. Louis 372–382
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirohi, T., Yoshimura, K. Surgical Correction of Retracted Nostril Rim with Auricular Composite Grafts and Anchoring Suspention . Aesth. Plast. Surg. 27, 418–422 (2003). https://doi.org/10.1007/s00266-003-3091-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-003-3091-1