Abstract
Purpose
The influence of lateral patellofemoral osteoarthritis (PFOA) in medial unicompartmental knee arthroplasty (UKA) is controversial. Our aim was to identify radiographic factors that may lead to progressive PFOA after implantation of a fixed-bearing medial UKA and their impact on patient-reported outcomes (PROMs).
Methods
A retrospective consecutive cohort of patients undergoing medial UKA with a minimum follow-up of 60 months between September 2011 and January 2017 was identified. All UKAs had a fixed-bearing design with cemented femoral and tibial components. PROMs included documentation of the Oxford Knee Score (OKS). The following radiographic parameters were evaluated on conventional radiographs and computer tomography (CT) scans: patella tilt angle, patella congruence angle, Caton-Deschamps index, medial and lateral patellofemoral degeneration (Kellgren-Lawrence Classification (KL)), mechanical anteroposterior axis, femoral torsion, tibial tuberosity to trochlear groove distance (TTTG), anteroposterior translation of the femoral component. A hierarchical multiple regression analysis and partial Pearson correlation analysis (SPSS) were used to evaluate for predictors of progression of lateral PFOA.
Results
Forty-nine knees allowed PFOA assessment and had an average follow-up of 62 months (range 60–108). Twenty-three patients did not exhibit any progression of lateral PFOA. Twenty-two progressed with 1 stage, whereas four had progressed 2 stages according to the KL classification. TTTG negatively correlated with progressive lateral PFOA (r = − 0.436, p = 0.01). Progression of lateral PFOA did not correlate with OKS at last follow-up (p = 0.613).
Conclusion
A decreased TTGT correlated with radiographic progression of lateral PFOA after medial fixed-bearing cemented UKA. PFOA however did not influence PROMs at a minimum of five years postoperatively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a recognized treatment for medial compartment osteoarthritis (OA) of the knee with promising long-term implant survival rates ranging from 85 to 90% at 15 years [1, 2], as well as functional- and patient reported outcome measures (PROMs) [3]. Nevertheless, there is still debate about the ideal patient selection receiving this kind of joint replacement [4]. The most common reasons for revision are represented by osteoarthritis (OA) progression and aseptic loosening [5]. Up until now, radiologic or clinical evidence of patellofemoral joint osteoarthritis (PFOA) has not been considered an absolute contraindication for UKA, though its role remained controversial [6,7,8]. In fact, evidence exists that PFOA is an underappreciated subgroup of knee OA in respect of clinical symptoms [9, 10].
Due to postoperative aggravation of contralateral PFOA after UKA [11] and inferior clinical results in these population groups [12], the condition of preoperative PFJ degeneration gains even more importance relating to treatment options and indications. Some authors even consider a total knee arthroplasty more suitable in cases of preexisting chondral degeneration in the lateral patellofemoral compartment [12, 13]. As opposed to medial PFOA OA, the lateral PFOA seems to have an impact on PROMs according to Konan and Haddad [12]. The role of topographical location and severity of cartilage damage in the patellofemoral joint needs further clarification, as the decision of undergoing TKA has an impact on patients’ health in terms of hospital stay duration, range of motion, short-term complication and revision rates [14, 15].
It is further hypothesized that an increased femoral antetorsion may lead to patellofemoral degeneration in native knees [16]. Since lateral PFOA can potentially influence outcomes after UKA, and several factors are described in the literature influencing patellofemoral joint stress [16,17,18,19,20], this study aims to identify radiographic factors associated with progression of lateral PFOA after medial fixed-bearing UKA and to evaluate its correlation to the mid-term PROMs and revision rates.
Methods
This retrospective study was approved by the ethics commission board of northwest and central Switzerland and was conducted entirely at the authors’ institution: BASEC Nr 2022–01,280.
Study cohort
Out of the institution’s database that included every unicompartmental or total knee replacement executed between September 2011 and January 2017, all UKA were identified. Patients with a minimum follow-up of five years were reviewed retrospectively. Patients underwent primary UKA (MyKnee UNI®, Medacta International, Castel San Pietro, CH) for symptomatic, medial unicompartmental knee OA stage III–IV according to the Kellgren–Lawrence classification (primary or secondary) [21] with sparing of the lateral tibiofemoral compartment. Preoperative radiological assessment was carried out analyzing weight-bearing anteroposterior, lateral, and Rosenberg views of the knee and an axial view of the patella. Mechanical axis was evaluated preoperatively using a weight bearing full-length anteroposterior radiograph.
Indications included the prerequisites: frontal deformity < 15°; flexion contracture < 15°; functional integrity of the anterior cruciate ligament (ACL), and peripheral ligaments of the knee as well as the absence of an inflammatory arthropathy [22]. UKA implantation for anteromedial OA requires medial bone-on-bone arthritis, a functionally normal ACL, a functionally normal medial collateral ligament, intact full-thickness lateral tibiofemoral cartilage [23].
Surgical technique
The UKAs were performed by two staff surgeons. Minimal invasive incisions of the medial respectively lateral parapatellar approach were utilized. The patella was subluxated but not everted laterally. In all participants, tibial and femoral preparation was performed using patient-specific, 3D-printed cutting blocks made of Polyamid PA12 by Medacta International, which were designed fitting the local anatomy according to the preoperative computed tomography (CT). The data of the preoperatively scans were sent to the company engineers (Medacta International S.A., Castel San Pietro, Switzerland). The position and size of the TKA according to the surgeon’s preferences was planned. In all cases, a neutral mechanical axis [0°; or hip–knee–ankle angle (= HKA) = 180°], a posterior slope of the tibia component between 2° and 4°, a flexion of the femoral component between 0° and 4° aiming best component position without notching or overhang, and an external rotation of the femoral component of 3° or 4° were intended. After assessment and eventual correction, the surgeon confirms the protocol and the patient-specific cutting blocks were manufactured [24]. Implants had fixed-baring design with cemented tibial and femoral component and were produced by MyKnee Solutions of Medacta International® (Strada Regina, 6874 Castel San Pietro, Switzerland). In several cases with small tibial component size (< 2), a full-polyethylene implant may have been used instead of a metal-backed implant [25]. Clinical and radiological assessments were conducted at three months, one year, and five years postoperatively.
Clinical outcome measures
During the postoperative follow-ups, Oxford knee score (OKS) as a representative of the PROMs for the knee has been assessed standardly. Only the OKS at the last consultation was taken into account during the analysis. If patient records reported a radiological assessment and a missing OKS, they were excluded.
Radiographic assessment
The following parameters were evaluated on pre- and postoperative conventional radiographs: Patella tilt angle, patella congruence angle, Caton-Deschamp’s index, medial and lateral patellofemoral degeneration (Kellgren-Lawrence classification), frontal mechanical axis, and anteroposterior translation of the femoral component. Tibial tuberosity to trochlear groove distance (TT-TG) and femoral torsion were assessed on the preoperative three-dimensional CT scan. Measurements were always taken from recordings of the last available follow-up. Conventional radiographs were recorded standardly weight-bearing. CT examination had been performed in supine position with straightened legs and a symmetric pelvis. Imaging was analyzed in a blinded manner on the picture archiving and communication system (PACS) using PACS measurement tools. Calibration was performed using a 25-mm reference ball [26].
Lateral patellofemoral joint degeneration
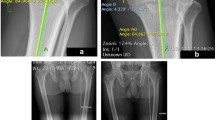
To record pre- and postoperative degenerative changes in the patellofemoral compartment of the knee on standard skyline radiographs of the patella [27], Kellgren-Lawrence (KL) classification system was applied (Fig. 1) [28,29,30]. It classifies radiographs as follows: 0, no findings of osteoarthritis; 1, doubtful joint space narrowing and possible osteophytic lipping; 2, definite osteophytes and possible joint space narrowing; 3, multiple osteophytes, definite joint space narrowing, small pseudocysts, and possible deformity of bone contour; 4, large osteophytes, marked joint space narrowing, severe sclerosis, and definite deformity of bone contour [21]. Disease progression was accounted for any change in the degree of KL PFOA.
Pre- and postoperative contralateral patellofemoral joint degeneration was analyzed on skyline-view radiographs. In order to grade patellofemoral arthrosis, the Kellgren-Lawrence classification system (KL grade 1–4) was applied. This example shows a right patellofemoral joint with grade 2 lateral degeneration (asterisks in picture A) preoperatively and grade 4 lateral degeneration (asterisks in picture B) 60 months postoperatively
TT-TG
Preoperative Tibial tuberosity to trochlear groove distance (TT-TG) measurements were performed, as traditionally described [31], in CT radiographs (Fig. 2). Thus, patellar translation was documented by measuring the transverse distance between the femoral trochlear groove and the tibial tuberosity on axial CT imaging.
TT-TG was measured traditionally in axial CT radiographs: This example pictures a right knee. A rectangular line (CD) relating to a tangent (AB) touching the posterior aspect of the femoral condyles was drawn, bisecting the trochlear groove (TG) of the femur. A second rectangular line (EF) bisecting the anterior spur of the tibial tuberosity (TT) was then applied. Distance between these two lines (D′) was measured and depicted as TT-TG distance
Caton-Deschamp’s index
In order to establish the vertical level of the patella, Caton-Deschamp’s index was calculated [32]. According to the describers, the patellar articular surface length and the length between the anterior angle of the tibia plateau and the most inferior aspect of the patellar articular surface were put in relation. Measurements were conducted in lateral recordings of the knee (Fig. 31).
1 Caton-Deschamps index was measured on lateral x-rays of the knee. In order to calculate the index, the distance between the anterior angle of the tibial plateau and the inferior aspect of the patellar articular surface (red arrow) as well as the patellar articular surface length (green arrow) were measured. 2 Patellar tilt angle was measured as the angle (⍺) between a tangent touching the anterior surface of the femoral condyles (A and B) and a line intersecting the patella on its widest part. 3 Patellar congruence angle measurement: a left patellofemoral joint is depicted in skyline-view. First, the angle between the highest medial (C) and lateral (D) point of the femoral condyles was measured centering over the trochlear sulcus (TS). Then, the lowest point of the articular ridge of the patella (F) was identified. A line was drawn from TS through F. The angle (γ) between the trochlear grove bisectrix and the line crossing TS and F was accepted as patellar congruence angle
Patellar tilt angle
Patellar tilt angle was measured in the Merchant view. In this series, the angle between the intercondylar line and a line drawn through the transverse axis of the patella was adopted [33]. The patellar tilt was expressed as a positive value, when the transverse axis of the patellar body tilted to the lateral side of the knee (Fig. 32) and as a negative value when it tilted medially [34].
Patellar congruence angle
As an index for patellar subluxation, patellar congruence angle was assessed, measuring the angular stretch between the bisecting line of the sulcus angle and a line drawn from the apex of the sulcus angle to the lowest point of the patellar articular ridge [35]. Again, lateral subluxation was defined as a positive value, concluding a negative value for medial subluxation. Measurements were performed in Merchant views of the patella (Fig. 33).
Frontal mechanical axis
Mechanical axis measurements were performed on full-length weight-bearing anteroposterior radiographs. The angle between a line from the centre of rotation of the femoral head, respectively the centre of the medial and lateral malleolar aspect to the centre of the patella, was assessed. Valgus alignment of the knee, where the patellar centre was lying medial to the Mikulicz line, was defined as a negative value. Varus alignment was assigned a positive value.
Femoral component anteroposterior position
Since anteroposterior position of the femoral component seems to influence patellar osteoarthritis after unicompartmental knee arthroplasty, this parameter was captured as well according to the method described by Hernigou and Dechamps [11]. On preoperative radiographs, the distance between the intercondylar roof to a parallel line aiming on the trochleocondylar junction was measured (Fig. 41, 2). On postoperative images, the distance from the intercondylar roof to a parallel line through the anterior aspect of the component was measured. The difference between these two distances displayed the anteroposterior position of the femoral component in relation to the trochleocondylar junction [11].
1 and 2 depict the method used to measure femoral component position. Referring to the method presented by Hernigou and Deschamps, lateral knee x-rays were used. Preoperatively, the distance (H) resulted of the measurement in millimeters between the slope of the intercondylar roof (AB) and a parallel line (CD) crossing the trochleocondylar junction (TCJ). Postoperatively, the distance H′ resulted of the distance between slope of the intercondylar roof (A′B′) and a parallel line (C′D′) crossing the anterior part of the femoral component (AFC)
Femoral torsion
Torsion measurement of the femur was performed according to the method described by Murphy et al. [36, 37]. This method is frequently used and seems to accurately address femoral torsion. Hence, the utilized landmarks in the preoperative CT consisted of the posterior distal femur condyles, femoral head centre, and femoral neck. Thereby, the anterior angulation line was centered between the anterior and posterior femoral neck cortex on the level just superior to the lesser trochanter. The posterior angulation line was drawn tangential on the posterior distal femoral condyles (Fig. 5).
The figure shows the applied measurement technique of the femoral torsion: Here, the angle (⍺) between a tangent touching the posterior aspect of the femoral condyles and a line bisecting the middle of the femoral neck width (FNW) just above the minor trochanter region and subsequently passing through the femoral head rotation centre (RC) was recorded
Statistical analysis
Descriptive analyses of patient characteristics were performed with use of means and standard deviations for continuous variables and with frequencies and percentages for discrete or dichotomous variables. Pearson’s correlation analysis was used to identify correlations between PROMs and radiographic findings.
A hierarchical multiple regression analysis (SPSS) was used to evaluated for independent predictors of progression of OA in the LPF compartment. This was done to first match the population based on the following variables: BMI, age, and gender. An a priori power analysis for a multiple regression revealed a minimum required sample size of 41 for an anticipated effect size (f2) = 0.35 (large effect size) and a desired statistical power of 0.8 (total number of predictors — 7). The multiple regression analysis allowed the inclusion of all covariates (TTTG distance, Caton-Deschamps Index, femoral torsion, postoperative femoral component anteroposterior position, delta mechanical axis, delta patella tilt, and delta patella congruence) in the regression equation for calculation of each risk factor independently. The sample size of the study has achieved these minimal requirements.
All statistical tests were 2-sided, and p value of < 0.05 was considered statistically significant. All analysis was performed with SPSS (version 23.0; IBM SPSS Statistics).
Results
From a total of 69 eligible patients, 57 (83%) were available for follow-up. Out of these, there were 49 patients with available pre- and postoperative Merchant views that allowed PFOA assessment and were selected for further analysis. The last follow-up averaged 62 months (range 60–108). There were 31 males and 18 females with an average age of 69 years (range 47–82). The BMI averaged 28.6 kg/m2 (range 21–39.7). All the medial UKAs had cemented femoral and cemented tibial components, with two knees having received a full-polyethylene cemented tibial implant. Five patients (10%) received previous surgery: four a partial medial meniscectomy and one a previous high tibial osteotomy (HTO). Regarding comorbidities, seven patients (14%) suffered from diabetes mellitus. At the last follow-up, there were no revision surgeries and no conversions to TKA. The OKS score averaged 43.5 at last follow-up (range 22–48).
The pre- and postoperative radiographic parameters along with the PFOA degeneration are emphasized in Table 1. The preoperative mechanical axis averaged 6° (range 0 to 12°), with some postoperative values insinuating overcorrections (range − 2 to 10°). There were no subchondral cysts before surgery with five subchondral retropatellar cysts depicted medially and two knees with both medial and lateral retropatellar subchondral cysts on latest Merchant view radiographs. Twenty-three patients did not exhibit any progression of degeneration in the LPF compartment. Twenty-two progressed with 1 stage OA, whereas four had progressed 2 stages OA according to the KL classification (Table 1).
A hierarchical multiple regression analysis matched on BMI, gender, and age revealed that lower values of TTTG correlated with progressive lateral PFOA (r = − 0.436, p = 0.01). Femoral torsion (p = 0.102), postoperative anteroposterior position of the femoral component (p = 0.410), and the Caton-Deschamps Index (p = 0.860) were not independent predictors for progression of lateral PFOA. Preoperative, postoperative, and delta values of the mechanical axis (p = 0.499), patella congruence angle (p = 0.678) and patella tilt (p = 0.678), did not show statistically significant correlation to lateral PFOA in the regression analysis.
Also, progression of lateral PFOA did not correlate (partial Pearson’s analysis with controlling for age, BMI, and gender) with OKS at last follow-up (p = 0.613).
Discussion
The main finding of this study is represented by the determined correlation of the preoperative TTTG in predicting progression of lateral PFOA after implantation of medial cemented fixed-bearing UKA. Although our initial assumption that an increased femoral antetorsion may lead to lateral PFOA, as it has already been observed in a cohort of native knees [16], did not confirm itself, we found a positive trend during regression analysis (p = 0.102). It is possible that in a bigger cohort with a larger sample size, smaller differences could have been detected, since our regression analysis had sufficient power for only large effect sizes.
An important limitation is the method of evaluation for joint degeneration that was used in our cohort. The KG classification is known to have only a moderate to substantial inter-rater and intrarater reliability [38]. Ideally, magnetic resonance imaging (MRI) with metal artifact-reducing sequences should be used [39]. Although trochlear dysplasia is mainly attributed to patellofemoral instability [40], any changes to the depth of the trochlea or the initial trochlear morphology in UKA could potentially impact the contact pressure in the patellofemoral joint [41]. There is a recent report [42] where the presence of lateral trochlear osteophyte was associated with poor PROMs after medial UKR. Our cohort, however, did not have a significant number of osteophytes, which could not confirm or infirm the results from the study by Carender et al. [42]. Whether the patellar morphology can impact the PFOA is also to be investigated, as it could play a role in patellofemoral instability [43, 44]. A further aspect worth considering is the rotational position of the components in the axial plane. An optimal implant should have between 2° and 6° femoral component external rotation and 1–8° tibial component external rotation in mobile-bearing UKR [45]. In fixed-bearing UKR, the tibial component rotation can be oriented based on the tibial tuberosity, and the other components are implanted for best fit, without evidence of impingement or instability in both flexion and extension [46]. A rotation between 3° of internal to 3° of external rotation should be achieved [47]. Our data lacked a postoperative CT scan, which prevented the assessment of component rotation.
As mentioned above, in our cohort, the OKS score did not correlate with progression of lateral PFOA at the last follow-up. Apart from the imperfection of the OKS for the evaluation of patellofemoral symptoms, it is possible that a certain degree of disease progression is necessary in order to change PROMs [48, 49]. Disease progression with 1 stage according to KL classification may be too little to impact PROMs significantly.
Generally, the TTTG distance is used to evaluate for an overly lateral insertion of the patellar tendon on the tibia in cases with patellar instability [50]. Next to its known contribution to instability, Stephen et al. reported an increased joint contact pressure in their cadaveric study on eight specimens [51]. Also, in a recent cross-sectional study, it was shown that an increased, rather than decreased, TTTG distance may contribute to patellofemoral pain syndrome in native knee joints [52]. Tanaka [53] and Kaplan [54], however, have described negative correlations of decreased sagittal TTTG distances and patellofemoral chondral lesions in native knees. Since these papers were investigating natural knees and UKAs clearly seem to influence patellofemoral biomechanics dependent on femoral component placement (Hernigou and Deschamps, 2002), further investigation needs to be conducted to establish the role in predicting PFOA after UKA. Future prospective studies should clarify the role of TTTG distance on the pathomechanics of the medial UKA on the patellofemoral joint and ultimately the impact on PFOA and PROMs [55].
The main limitation of our study is a lack of a specific PROM measures for the patellofemoral joint. Although the OKS has been already used across multiple studies for evaluation of patient satisfaction and function after medial UKA [56], the need of a more specific PROM measure has been advocated in recent publications [57]. As such, the influence of lateral PFOA on the outcome of medial UKAs needs further investigation. Nevertheless, our study is the first to have investigated radiographic predictors of progression of lateral PFOA after implantation of a fixed-bearing design of a medial UKA. Previous reports which have focused on investigations of Oxford mobile-bearing designs [12, 58] did not investigate the progression of PFOA [35] and did not include the same amount of radiographic parameters as depicted here (these studies lacked assessment of TTTG, femoral torsion, and other) [12, 35].
Conclusion
A decreased TTGT correlated with radiographic progression of lateral PFOA after medial fixed-bearing cemented UKA. PFOA however did not influence PROMs at a minimum of five years postoperatively.
Data availability
All study associated data is stored on a local storage in the institutional database and is password-protected. These data can be accessed and reused; shall the need arise.
References
Rossi SMP, Sangaletti R, Nesta F et al (2022) A well performing medial fixed bearing UKA with promising survivorship at 15 years. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04562-7
Crawford DA, Rutledge-Jukes H, Alexander JS et al (2023) 15-year follow-up of mobile bearing medial unicompartmental knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2023.01.024
Berger RA, Nedeff DD, Barden RM, et al (1999) Unicompartmental knee arthroplasty. Clinical experience at 6- to 10-year followup. Clin Orthop Relat Res 50–60
Pandit H, Jenkins C, Gill HS et al (2011) Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Jt Surg Br 93:622–628. https://doi.org/10.1302/0301-620x.93b5.26214
Ernstbrunner L, Imam MA, Andronic O et al (2018) Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop 42. https://doi.org/10.1007/s00264-017-3662-4
Beard DJ, Pandit H, Gill HS et al (2007) The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Jt Surg Br 89:1597–1601. https://doi.org/10.1302/0301-620x.89b12.19259
Beard DJ, Pandit H, Ostlere S et al (2007) Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Jt Surg Br 89:1602–1607. https://doi.org/10.1302/0301-620x.89b12.19260
Song EK, Park JK, Park CH et al (2016) No difference in anterior knee pain after medial unicompartmental knee arthroplasty in patients with or without patellofemoral osteoarthritis. Knee Surg Sport Traumatol Arthrosc 24:208–213. https://doi.org/10.1007/s00167-014-3367-9
Crossley KM, Hinman RS (2011) The patellofemoral joint: the forgotten joint in knee osteoarthritis. Osteoarthr Cartil 19:765–767. https://doi.org/10.1016/j.joca.2011.05.005
Duncan R, Peat G, Thomas E et al (2008) How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatol 47:1704–1707. https://doi.org/10.1093/rheumatology/ken339
Hernigou P, Deschamps G (2002) Patellar impingement following unicompartmental arthroplasty. J Bone Jt Surg Am 84:1132–1137. https://doi.org/10.2106/00004623-200207000-00006
Konan S, Haddad FS (2016) Does location of patellofemoral chondral lesion influence outcome after Oxford medial compartmental knee arthroplasty? Bone Jt J 98-b:11–15. https://doi.org/10.1302/0301-620x.98b10.Bjj-2016-0403.R1
Stern SH, Becker MW, Insall JN (1993) Unicondylar knee arthroplasty. An evaluation of selection criteria. Clin Orthop Relat Res 143–148
Wilson HA, Middleton R, Abram SGF et al (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ 364:l352. https://doi.org/10.1136/bmj.l352
Siman H, Kamath AF, Carrillo N et al (2017) Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: comparable reoperation, revision, and complication rates. J Arthroplast 32:1792–1797. https://doi.org/10.1016/j.arth.2017.01.020
Flury A, Hoch A, Andronic O et al (2021) Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sport Traumatol Arthrosc 29:1760–1768. https://doi.org/10.1007/s00167-020-06223-x
Cahue S, Dunlop D, Hayes K et al (2004) Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum 50:2184–2190. https://doi.org/10.1002/art.20348
Macri JJ, Khan KK, Crossley KMES (2016) Is tibiofemoral or patellofemoral alignment or trochlear morphology associated with patellofemoral osteoarthritis? A Systematic Review. Arthritis Care Res 68:1453–1470. https://doi.org/10.1002/acr.22842
Kaiser P, Loth F, Attal R et al (2020) Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sport Traumatol Arthrosc 28:952–959. https://doi.org/10.1007/s00167-019-05588-y
Cicuttini F, Wluka A, Wang Y, Stuckey S (2002) The determinants of change in patella cartilage volume in osteoarthritic knees. J Rheumatol 29:2615–2619
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502. https://doi.org/10.1136/ard.16.4.494
Panni AS, Vasso M, Cerciello S, Felici A (2012) Unicompartmental knee replacement provides early clinical and functional improvement stabilizing over time. Knee Surg Sports Traumatol Arthrosc 20:579–585. https://doi.org/10.1007/s00167-011-1613-y
Vasso M, Antoniadis A, Helmy N (2018) Update on unicompartmental knee arthroplasty: current indications and failure modes. EFORT open Rev 3:442–448. https://doi.org/10.1302/2058-5241.3.170060
Koch PP, Müller D, Pisan M, Fucentese SF (2013) Radiographic accuracy in TKA with a CT-based patient-specific cutting block technique. Knee Surgery, Sport Traumatol Arthrosc 21:2200–2205. https://doi.org/10.1007/s00167-013-2625-6
Houdek MT, Wagner ER, Wyles CC et al (2016) All-polyethylene tibial components: an analysis of long-term outcomes and infection. J Arthroplasty 31:1476–1482. https://doi.org/10.1016/j.arth.2015.12.048
Archibeck MJ, Cummins T, Tripuraneni KR et al (2016) Inaccuracies in the use of magnification markers in digital hip radiographs. Clin Orthop Relat Res 474:1812–1817. https://doi.org/10.1007/s11999-016-4704-8
Heng H-YC, Bin AbdRazak HR, Mitra AK (2015) Radiographic grading of the patellofemoral joint is more accurate in skyline compared to lateral views. Ann Transl Med 3:263. https://doi.org/10.3978/j.issn.2305-5839.2015.10.33
Ji X, Li H, Yang S et al (2022) Patellofemoral osteoarthritis does not influence clinical outcomes of fixed-bearing unicompartmental knee arthroplasty. Medicine (Baltimore) 101
Dai Y, Yin H, Xu C et al (2021) Association of patellofemoral morphology and alignment with the radiographic severity of patellofemoral osteoarthritis. J Orthop Surg Res 16:548. https://doi.org/10.1186/s13018-021-02681-2
Horváth G, Koroknai G, Ács B et al (2011) Prevalence of radiographic primary hip and knee osteoarthritis in a representative Central European population. Int Orthop 35:971–975. https://doi.org/10.1007/s00264-010-1069-6
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sport Traumatol Arthrosc 2:19–26. https://doi.org/10.1007/bf01552649
Caton J, Deschamps G, Chambat P et al (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Lewonowski K, Dorr LD, McPherson EJ et al (1997) Medialization of the patella in total knee arthroplasty. J Arthroplast 12:161–167. https://doi.org/10.1016/s0883-5403(97)90062-0
Aglietti P, Insall JN, Cerulli G (1983) Patellar pain and incongruence. I: Measurements of incongruence. Clin Orthop Relat Res 217–224
Burger JA, Kleeblad LJ, Laas N, Pearle AD (2019) The influence of preoperative radiographic patellofemoral degenerative changes and malalignment on patellofemoral-specific outcome scores following fixed-bearing medial unicompartmental knee arthroplasty. J Bone Joint Surg Am 101:1662–1669. https://doi.org/10.2106/JBJS.18.01385
Murphy SB, Simon SR, Kijewski PK et al (1987) Femoral anteversion. J Bone Jt Surg Am 69:1169
Schmaranzer F, Lerch TD, Siebenrock KA et al (2019) Differences in femoral torsion among various measurement methods increase in hips with excessive femoral torsion. Clin Orthop Relat Res 477:1073–1083. https://doi.org/10.1097/corr.0000000000000610
Köse Ö, Acar B, Çay F et al (2018) Inter- and intraobserver reliabilities of four different radiographic grading scales of osteoarthritis of the knee joint. J Knee Surg 31:247–253. https://doi.org/10.1055/s-0037-1602249
Müller GM, Månsson S, Müller MF et al (2014) MR imaging with metal artifact-reducing sequences and gadolinium contrast agent in a case-control study of periprosthetic abnormalities in patients with metal-on-metal hip prostheses. Skeletal Radiol 43:1101–1112. https://doi.org/10.1007/s00256-014-1893-7
Biedert RM, Netzer P, Gal I et al (2011) The lateral condyle index: a new index for assessing the length of the lateral articular trochlea as predisposing factor for patellar instability. Int Orthop 35:1327–1331. https://doi.org/10.1007/s00264-010-1142-1
Kaiser D, Götschi T, Bachmann E et al (2022) Deepening trochleoplasty may dramatically increase retropatellar contact pressures- a pilot study establishing a finite element model. J Exp Orthop 9:76. https://doi.org/10.1186/s40634-022-00512-9
Carender CN, Rand DR, DeMik DE et al (2023) Presence of a lateral trochlear osteophyte predicts medial unicompartmental arthroplasty failure at midterm follow-up. Arthroplast Today 19:101044. https://doi.org/10.1016/j.artd.2022.09.013
Jimenez AE, Levy BJ, Grimm NL et al (2021) Relationship between patellar morphology and known anatomic risk factors for patellofemoral instability. Orthop J Sport Med 9:2325967120988690. https://doi.org/10.1177/2325967120988690
Fucentese SF, von Roll A, Koch PP et al (2006) The patella morphology in trochlear dysplasia–a comparative MRI study. Knee 13:145–150. https://doi.org/10.1016/j.knee.2005.12.005
Ng JP, Fan JCH, Chau WW et al (2020) Does component axial rotational alignment affect clinical outcomes in Oxford unicompartmental knee arthroplasty? Knee 27:1953–1962. https://doi.org/10.1016/j.knee.2020.10.016
Kim TK, Mittal A, Meshram P et al (2021) Evidence-based surgical technique for medial unicompartmental knee arthroplasty. Knee Surg Relat Res 33:2. https://doi.org/10.1186/s43019-020-00084-x
Liow MHL, Tsai T-Y, Dimitriou D et al (2016) Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31:2167–2172. https://doi.org/10.1016/j.arth.2016.03.003
Perrone FL, Baron S, Suero EM et al (2018) Patient-reported outcome measures (PROMs) in patients undergoing patellofemoral arthroplasty and total knee replacement: a comparative study. Technol Heal care Off J Eur Soc Eng Med 26:507–514. https://doi.org/10.3233/THC-181185
Crossley KM, Macri EM, Cowan SM et al (2018) The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br J Sports Med 52:1130–1136. https://doi.org/10.1136/bjsports-2016-096776
Fucentese SF (2018) Patellofemoral instability. Orthopade 47:77–86. https://doi.org/10.1007/s00132-017-3501-8
Stephen JM, Lumpaopong P, Dodds AL et al (2015) The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med 43:186–194. https://doi.org/10.1177/0363546514554553
Carlson VR, Boden BP, Shen A et al (2017) The tibial tubercle-trochlear groove distance is greater in patients with patellofemoral pain: implications for the origin of pain and clinical interventions. Am J Sports Med 45:1110–1116. https://doi.org/10.1177/0363546516681002
Tanaka MJ, D’Amore T, Elias JJ et al (2019) Anteroposterior distance between the tibial tuberosity and trochlear groove in patients with patellar instability. Knee 26:1278–1285. https://doi.org/10.1016/j.knee.2019.08.011
Kaplan DJ, Mojica ES, Ortega PF et al (2022) Posterior tibial tubercle measured by the sagittal TT-TG distance correlates with increased risk for patellofemoral chondral lesions. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06988-3
Cheng J, Feng M, Cao G, Lu S (2020) Efficacy and mid/long-term survivorship of mobile-bearing unicompartmental knee arthroplasty for medial compartment knee osteoarthritis combined patellofemoral joint arthritis: a prospective cohort study protocol. BMJ Open 10:e038448. https://doi.org/10.1136/bmjopen-2020-038448
Harris LK, Troelsen A, Terluin B et al (2022) Interpretation threshold values for the Oxford Knee Score in patients undergoing unicompartmental knee arthroplasty. Acta Orthop 93:634–642. https://doi.org/10.2340/17453674.2022.3909
Green A, Liles C, Rushton A, Kyte DG (2014) Measurement properties of patient-reported outcome measures (PROMS) in patellofemoral pain syndrome: a systematic review. Man Ther 19:517–526. https://doi.org/10.1016/j.math.2014.05.013
Pongcharoen B, Reutiwarangkoon C (2016) The comparison of anterior knee pain in severe and non severe arthritis of the lateral facet of the patella following a mobile bearing unicompartmental knee arthroplasty. Springerplus 5:202. https://doi.org/10.1186/s40064-016-1914-1
Author information
Authors and Affiliations
Contributions
All the authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; (3) final approval of the version to be submitted; (4) being accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethical approval
The presented study was conducted in accordance with Swiss and international law requirements. This retrospective study was approved by the ethics commission board of northwest and central Switzerland and was conducted entirely at the authors’ institution: BASEC Nr 2022–01,280.
Informed consent
All participants have given written consent to participate in the study after being provided with appropriate documentation. Participants also gave consent for publication of the study results.
Competing interests
The authors declare that they have no conflict of interest regarding this study. Prof. Dr. med. Näder Helmy is a medical advisor of Medacta International (Switzerland) and receives royalties from Medacta International (Switzerland). Prof. Helmy reports no conflict of interest in relation to this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andronic, O., Helmy, N., Kellner, C. et al. A decreased tibial tuberosity-trochlear groove distance is associated with lateral patellofemoral joint degeneration after implantation of medial fixed-bearing unicompartmental knee arthroplasty — a minimum five year follow-up. International Orthopaedics (SICOT) 47, 2225–2233 (2023). https://doi.org/10.1007/s00264-023-05812-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05812-y