Abstract
Objective
The purpose of this prospective study was to compare the double reverse traction repositor (DRTR) and manual traction in retrograde intramedullary nailing (RE-IMN) for femoral shaft fractures.
Patients and methods
Seventy-seven patients with femur shaft fractures were randomized to undergo surgery with either DRTR or manual traction (MT) to facilitate RE-IMN between January 2018 and January 2019. Demographics, fracture characteristics, surgical data, post-operative complications, and functional outcomes were assessed. Data from 72 patients completing the final follow-up (12 months) were analysed in this study.
Results
The average number of intra-operative perspectives in the DRTR group was 27.7, which was significantly reduced compared with that in the MT group (31.3, p < 0.001). Fewer assistants were required in the DRTR group compared with the MT group (1.1 vs 1.9, p < 0.001). Fewer patients with open reduction were discovered in the DRTR group compared with the MT group (2.8 vs 19.4, p=0.024). Demographics, fracture characteristics, other surgical data, and prognostic parameters were comparative between the two groups.
Conclusions
The DRTR can be effectively and safely used to treat femur shaft fractures with RE-IMN. The DRTR achieves similar results as MT and is also superior to MT in terms of intra-operative perspectives, the number of assistants, and the open reduction rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral shaft fracture is a common condition in adults and represents 4.6% of all adult fractures [1]. The choice of treatment for femur shaft fractures has been updated in reference to the intramedullary nailing (IMN) technique by Kuntscher since the 1940s [2]. IMN has been regarded as the gold standard for the treatment of femoral shaft fractures over time [3, 4]. Antegrade intramedullary nailing (AN-IMN) or retrograde intramedullary nailing (RE-IMN) has been proven to be effective technologies available to orthopaedic surgeons. Both of these techniques have been demonstrated to have high union rates and low complication rates [5, 6]. Compared to RE-IMN, AN-IMN is more disadvantageous for patients with obesity, pregnancy, pelvic and hip fractures, or distal fractures [3, 7, 8]. AN-IMN is always associated with residual hip or thigh pain, Trendelenburg gait, superior gluteal nerve injury, avascular necrosis of the femoral head, heterotopic ossification, and iatrogenic femur neck fractures [3, 9,10,11]. In contrast to the reduction methods used in the application of AN-IMN with a traction table, RE-IMN mainly relies on manual traction (MT) to achieve and maintain the reduction of fractures. The inescapable phenomenon for MT is that the number of surgical assistants increases, which has been demonstrated to be accompanied by an increased infection rate [12]. Compared to the traction table, MT cannot provide stable and continuous traction force to obtain anatomical or nearly anatomical reduction, which is critical to the success of operation and the healing of fractures [13]. However, no specific traction instrument has been identified for the treatment of femoral shaft fractures with RE-IMN.
The double reverse traction repositor (DRTR), a traction instrument, has been certified to help orthopaedic surgeons achieve the successful reduction of lower extremity long bone fractures involving femoral neck fractures, intertrochanteric fractures, and tibial plateau fractures [14,15,16]. In our previous study, we assessed the application of the DRTR in the AN-IMN of femur shaft fractures and demonstrated that it was comparative or superior to the traction table in the AN-IMN of femur shaft fractures [17, 18]. Compared to the traction table, the DRTR has the advantage of greater traction force, fewer complications, and a wider range of applications. However, whether the DRTR can be used in the surgery of femoral shaft fractures with RE-IMN is uncertain.
The aims of this prospective randomized study were to (a) introduce the application of DRTR in the surgery of femoral shaft fractures with RE-IMN and (b) compare the use of DRTR and MT in the surgery of femoral shaft fractures with RE-IMN.
Patients and methods
This prospective randomized study was conducted in a level I trauma centre of a tertiary university hospital. Seventy-seven patients were enrolled in the present study according to the inclusion and exclusion criteria. The inclusion criteria were patients with femoral shaft fractures (AO classification type 32 A, 32 B, and 32 C) treated by RE-IMN between January 2018 and January 2019. The exclusion criteria were as follows: (1) age < 18 years, (2) multiple fractures, (3) pathological fractures, (4) open fractures, (5) old fracture (time from injury to surgery > 21 days), (6) incomplete data, (7) no walking ability or capacity before surgery, and (8) less than 12 months of follow-up. All the patients in our study were randomized to two groups according to the admitted date, including 39 patients with DRTR and 38 patients with MT. DRTR was applied in patients on odd-numbered days, and MT was used in patients on even-numbered days. The demographics and fracture characteristics were noted in our study, including age, sex, American Society of Anaesthesiologists (ASA) score, mechanism of injury, and AO classification type. Implementation of this study was agreed upon by the Institutional Review Board of our hospital. Informed consent was acquired from all patients.
Surgical techniques and follow-up protocol
Surgical techniques
All operations were performed by the same team, which consisted of two orthopaedic trauma surgeons with at least ten years of experience. All surgery was conducted under spinal or general anaesthesia. Routine prophylactic antibiotics were used 30 minutes before surgery.
DRTR group
All patients were placed in a supine position on a radiolucent table (Fig. 1a). Skin preparation and draping were conducted following anaesthesia. A 2-cm oblique incision was made to expose the ipsilateral iliac spine around the anterior superior iliac spine. A 5-mm transverse screw was used to fix the proximal support rod of the DRTR in the iliac spine. Then, 1–2 drapes were placed under the distal femur to make the knee joint flex. A longitudinal incision of approximately 4 cm was made on the medial side of the patellar tendon. The subpatellar fat pad was removed to expose the intercondylar fossa. Supracondylar traction or traction of the tibial tubercle was adopted according to the displacement direction of the distal fracture. When the fracture fragment was displaced backwards, the supracondylar traction of the femur was selected to conducive to correcting the displacement. If the fracture fragment was displaced forward, the traction of the tibial tubercle was selected. The diameter of the Kirschner wire was 3.0 mm or 2.5 mm in supracondylar traction or traction of the tibial tubercle, respectively. After the DRTR was installed, the handle of the DRTR was rotated to generate traction force between the iliac spine and distal femur until the quadriceps femoris muscle was visibly tense. The traction force belonged to skeletal traction which was produced by the K-wires in the iliac spine and distal femur, and the traction direction was consistent with the alignment of femur. Most of the displacements could be reduced under the powerful traction force of the DRTR, including overlapping, lateral, and rotation displacements. When residual anterior displacement of the proximal femur was observed, a special compression bar was used to achieve reduction (Fig. 1b).
After reduction was conducted, the femoral intercondylar fossa was drilled with an open cone. The gold finger was inserted under the C-arm monitor. Different types of reamers are used for reaming with the help of the guide wire (Fig. 1c). A suitable main nail was chosen to implant the femoral medullary cavity. Then, distal locking screws were implanted (Fig. 1d). At this time, the DRTR was removed, and the proximal locking device was installed. The proximal screw and tail cap were inserted. Then, the status and quality of fracture reduction and the position of the implant are reconfirmed under fluoroscopy (Fig. 2a–d). Finally, the incision was sutured.
MT group
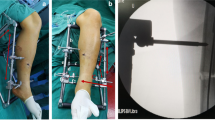
All patients were placed in a supine position on a radiolucent table. Skin preparation and draping were conducted following anaesthesia. The surgical approach in the MT group was similar to that in the DRTR group. In contrast to the surgery with the DRTR, the reduction was performed by at least two assistants who were used at the proximal and distal ends of the fracture separately to create traction force. When fracture reduction could not be achieved, a small incision was made around the fracture site to help perform fracture reduction. After reduction was achieved, the IMN was implanted under the traction of the assistants, which is the same as that used in the DRTR group. One more assistant is needed in the MT group compared to the DRTR group, and the continuous traction force and the maintenance of the reduction are disadvantages for the MT group compared with the DRTR group (Fig. 3a–c).
Follow-up protocol
Prophylactic antibiotic treatment was routinely used within 24 hours post-operatively, and pharmacological deep vein thrombosis prophylaxis was performed 24 hours after surgery. Active joint exercise in bed was gradually conducted 24 hours after surgery to prevent ankylosis postoperatively. Postoperatively, the patients should mobilize as soon as possible with partial weight-bearing within six weeks after the operation. Full weight-bearing was allowed when the fracture line disappeared in the X-ray.
Surgical data, including the duration of operation, the type of anaesthesia, the methods of reduction (closed or open), the number of perspectives, the intra-operative blood loss, intra-operative blood transfusion, the number of assistants, and post-operative complications, were recorded. Follow-up was routinely performed at one, three, six, nine and 12 months post-operatively. The final follow-up (12 months), including functional outcome interviews and radiographic evaluations, was required. If the fracture line was observed at the nine month follow-up, three consecutive months of follow-up were necessary for the patients. If limited progression was found, the outcome was defined as nonunion [19]. The Harris Hip Score (HHS) [20], visual analogue scale (VAS) [21], and Lysholm knee function score (LNY)[22] were evaluated at the final follow-up.
Statistical analysis
Data from patients completing the final follow-up (12 months) were analysed in this study. SPSS 23.0 software was used to analyse the data in the present study. Categorical variables are presented as frequencies and percentages, and continuous variables are presented as the means ± SD/mean ± SD (median). When continuous variables exhibit a normal distribution, Student’s t test was conducted to identify differences between the two groups. If not, the Mann-Whitney U test was employed. In the comparison of categorical variables between groups, the Pearson chi-square test and Fisher’s exact chi-square test were used. In all statistical analyses, statistical significance was accepted for a value of p <0.05.
Results
The comparison of demographics and fracture characteristics between the two groups is shown in Table 1. An older average age was noted in the DRTR group compared with the MT group (54.5 vs 47.5, p=0.288). The percentage of males in the DRTR group was 58.3%, which was greater than that in the MT group, but no significant difference was discovered between the two groups in sex (p=0.465). The other demographics and fracture data were comparable between the two groups.
The comparison of surgical data between the two groups is shown in Table 2. The average number of intra-operative perspectives in the DRTR group was 27.7, which was significantly lower than that in the MT group (31.3, p < 0.001). There were fewer assistants in the DRTR group compared with the MT group (1 (1–2) vs 2 (1–2), p < 0.001). A lower open reduction rate was discovered in the DRTR group compared to the MT group (2.8 vs 19.4, p=0.024). Although no significant difference was noted between the two groups in the duration of operation, the duration was shorter in the DRTR group compared with the MT group (134.3 vs 148.6). No significant differences in other surgical data were noted between the two groups.
The comparison of prognostic data between the two groups is shown in Table 3. No significant difference was noted in the functional outcome between the two groups. Complications between the two groups were comparable. All patients in the DRTR group achieved union in our study. Only one nonunion case was found in the MT group, and this case achieved successful union after secondary procedures.
Discussion
IM is regarded as the gold standard in surgery for adult femoral shaft fractures. Regardless of antegrade or retrograde nailing, ideal implantations were available to orthopaedic surgeons. Despite different indications, similar results regarding postoperative complications, union rate, short-term function outcomes, and long-term function outcomes were noted [23, 24]. As a reduction device, the traction table plays an important role in the reduction of femur shaft fractures treated by AN-IMN, which can offer continuous and stable traction forces. However, RE-IMN is unavailable for the treatment of femur shaft fractures in the knee flexion position during surgery. No effective reduction device has been designed for the reduction of femur shaft fractures with RE-IMN. As a rapid redactor, DRTR has been successfully used in the treatment of lower limb fractures [14, 18]. In the present study, the DRTR was applied in the treatment of femur shaft fractures with RE-IMN, which was the first reduction device to help achieve reduction in the treatment of femur shaft fractures with RE-IMN. The results of this study demonstrated that the DRTR was superior to manual traction in terms of the number of intra-operative perspectives, the number of assistants, and the open reduction rate for the treatment of femur shaft fractures with RE-IMN.
The quality of reduction is directly associated with the healing of fractures [13]. Intra-operative perspective could help the surgeon obtain ideal reduction. The average intra-operative perspective was 27.7 in the DRTR group, which was less than that in the MT group (31.3, p<0.001). In contrast to the MT, the traction force produced by the DRTR was continuous and stable, which contributed to the maintenance of the reduction until the intramedullary nail was successfully implanted. The preservation of the reduction could avoid an additional perspective for the implantation of the IMN. This notion might explain why the DRTR group had fewer intra-operative perspectives compared with the MT group. In addition, surgeons in the MT group might be exposed to more radiation given that the operation team is more approximated to the patient and C-arm device [25].
Compared to the MT, another advantage of the DRTR was that it was associated with a significant decrease in the number of assistants (Table 2). A previous study reported that an increasing number of assistants was closely related to increasing medical costs, especially for patients in developed countries [26]. Although the application of the DRTR might be associated with additional time for its installation, the duration of the surgery in the DRTR group was reduced compared with that in the MT group (134.3 mins vs 148.6 mins). The shorter reduction time and fixation time in the DRTR group might lead to this result. Besides, there were less blood loss (330.6 vs 358.3 ml), intra-operative blood transfusion (255.6 vs 269.4 ml), and postoperative hospital stay (8.8 vs 9.3 days) in the DRTR, compared to those in MT group. Although, no significant difference in them was observed between the two groups, the difference might be evident in future large-scale comparative studies.
Open reduction is always accompanied by increased trauma and more blood loss, which is associated with the increasing risks of nonunion and infection [27, 28]. The present study discovered a significantly lower open reduction rate in the DRTR group compared with the MT group. In our previous studies, we demonstrated that the DRTR could generate a traction force comparable to that of the traction table in the treatment of femur shaft fractures with AN-IMN [18]. Most overlapping deformities and anteroposterior or lateral deformities were corrected under adequate traction. In most cases, femur traction was chosen because more traction force could be generated compared to traction of the tibial tubercle. Femur traction was preferred if a posterior angular deformity was noted or the distal end of the fracture was shortened backward relative to the proximal end. The Kirschner wire was inserted as close as possible to the front of the femur such that the traction force was conducive to correcting the displacement. On implanting the Kirschner wire of femur traction, the supracondylar articular surface of the femur served as a reference through the anterior incision of the knee so that it would be as close as the anterior femoral cortex and not affect the implantation of the IMN. Traction of the tibial tubercle was preferred if there was an anterior angular deformity. In addition, the traction force was consistent with the mechanical axis of the femur, which would not aggravate the displacement of the wedge fragment. The rotational deformity in the distal femur was completely corrected.
The loss of follow-up rate was 6.9% (5 of 77 patients) in the present study, which guaranteed its quality. Some limitations remained in our study. First, the sample size in this study was small, and the follow-up time in patients was short. Second, this was a single-centre study that was limited by its inherent defects. A multicentre, large-sample study of the RE-IMN treatment of femur shaft fractures with DRTRs should be conducted in the future.
Conclusion
First, we introduced the application of the DRTR in the treatment of femur shaft fractures with RE-IMN in the present study. Second, we demonstrated that the DRTR could effectively and safely treat femur shaft fractures with RE-IMN and could achieve similar results as MT. Moreover, the DRTR was superior to the MT in terms of intra-operative perspectives, the number of assistants, and the open reduction rate.
References
Zhang Y (2016) Clinical epidemiology of orthopaedic trauma. Thieme, New York
Bong M, Koval J (2006) The history of intramedullary nailing. Bulletin of the NYU hospital for joint diseases 64(3-4):94–97
Ricci M, Gallagher B, Haidukewych G (2009) Intramedullary nailing of femoral shaft fractures: current concepts. The Journal of the American Academy of Orthopaedic Surgeons 17(5):296–305. https://doi.org/10.5435/00124635-200905000-00004
Giannoudis P, Stavrou Z, Papakostidis C. (2014) Nailing of femoral shaft fractures. In European surgical orthopaedics and traumatology: the efort textbook, Bentley, Ed. Springer Berlin Heidelberg: Berlin, Heidelberg, 2677-2697.
Papadokostakis G, Papakostidis C, Dimitriou R et al (2005) The role and efficacy of retrograding nailing for the treatment of diaphyseal and distal femoral fractures: a systematic review of the literature. Injury 36(7):813–822. https://doi.org/10.1016/j.injury.2004.11.029
Zhang F, Zhu L, Li Y et al (2015) Retrograde versus antegrade intramedullary nailing for femoral fractures: a meta-analysis of randomized controlled trials. Curr Med Res Opin 31(10):1897–1902. https://doi.org/10.1185/03007995.2015.1078783
Ricci W, Bellabarb C, Evanoff et al (2001) Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma 15(3):161–169. https://doi.org/10.1097/00005131-200103000-00003
Yu C, Singh V, Mariapan S et al (2007) Antegrade versus retrograde locked intramedullary nailing for femoral fractures: which is better? European journal of trauma and emergency surgery : official publication of the European Trauma Society 33(2):135–140. https://doi.org/10.1007/s00068-007-6156-z
Perez E, Jahangir A, Mashru R et al (2007) Is there a gluteus medius tendon injury during reaming through a modified medial trochanteric portal? A cadaver study. J Orthop Trauma 21(9):617–620. https://doi.org/10.1097/BOT.0b013e318157bda7
Helmy N, Jando V, Lu T et al (2008) Muscle function and functional outcome following standard antegrade reamed intramedullary nailing of isolated femoral shaft fractures. J Orthop Trauma 22(1):10–15. https://doi.org/10.1097/BOT.0b013e31815f5357
Sanders D, MacLeod M, Charyk-Stewart T et al (2008) Functional outcome and persistent disability after isolated fracture of the femur. Canadian journal of surgery. Journal canadien de chirurgie 51(5):366–370
Howard J, Hanssen A (2007) Principles of a clean operating room environment. J Arthroplast 22(7 Suppl 3):6–11. https://doi.org/10.1016/j.arth.2007.05.013
Kaufer H (1980) Mechanics of the treatment of hip injuries. Clin Orthop Relat Res 146:53–61
Zhao K, Zhang J, Li J et al. (2020). Treatment of unstable intertrochanteric fractures with proximal femoral nailing antirotation: traction table or double reverse traction repositor. Journal of investigative surgery: the official journal of the Academy of Surgical Research, 1–7. Advance online publication. https://doi.org/10.1080/08941939.2020.1786610.
Li S, Yin Y, Zhang R et al (2019) Minimally invasive treatment for fractures of lower extremity amputees using a rapid reductor. Int Orthop 43(6):1473–1478. https://doi.org/10.1007/s00264-018-4072-y
Li D, Song D, Ni J et al (2017) A case report of Schatzker type VI tibial plateau fracture treated with double reverse traction closed reduction combined with minimally invasive percutaneous plate osteosynthesis technique: a case report. Medicine 96(45):e8394. https://doi.org/10.1097/MD.0000000000008394
Chen W, Zhang T, Wang J et al (2016) Minimally invasive treatment of displaced femoral shaft fractures with a rapid reductor and intramedullary nail fixation. Int Orthop 40(1):167–172. https://doi.org/10.1007/s00264-015-2829-0
Zhang R, Yin Y, Li S et al (2018) Traction table versus double reverse traction repositor in the treatment of femoral shaft fractures. Sci Rep 8(1):5952. https://doi.org/10.1038/s41598-018-24317-y
Somford M, Bekerom M, Kloen P (2013) Operative treatment for femoral shaft nonunions, a systematic review of the literature. Strategies in trauma and limb reconstruction 8(2):77–88. https://doi.org/10.1007/s11751-013-0168-5
Harris H (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Kremer E, Atkinson J, Ignelzi R (1981) Measurement of pain: patient preference does not confound pain measurement. Pain 10(2):241–248. https://doi.org/10.1016/0304-3959(81)90199-8
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154. https://doi.org/10.1177/036354658201000306
Brewster J, Grenie G, Taylor B et al (2020) Long-term comparison of retrograde and antegrade femoral nailing. Orthopedics 43(4):e278–e282. https://doi.org/10.3928/01477447-20200415-04
Kumar P, Neradi D, Kansal R et al (2019) Greater trochanteric versus piriformis fossa entry nails for femur shaft fractures: resolving the controversy. Injury 50(10):1715–1724. https://doi.org/10.1016/j.injury.2019.07.011
Şahin E, Songür M, Kalem M et al (2016) Traction table versus manual traction in the intramedullary nailing of unstable intertrochanteric fractures: a prospective randomized trial. Injury 47(7):1547–1554. https://doi.org/10.1016/j.injury.2016.04.012
Burgers P, Hoogendoorn M, Van Woensel E et al (2016) Total medical costs of treating femoral neck fracture patients with hemi- or total hip arthroplasty: a cost analysis of a multicenter prospective study. Osteoporos Int 27(6):1999–2008. https://doi.org/10.1007/s00198-016-3484-z
Davis B (2005) Factors affecting rates of infection and nonunion in intramedullary nailing. The Journal of bone and joint surgery. British volume 87(4):589–590. https://doi.org/10.1302/0301-620X.87B4.16232
Harrop J, Styliaras J, Ooi Y et al (2012) Contributing factors to surgical site infections. The Journal of the American Academy of Orthopaedic Surgeons 20(2):94–101. https://doi.org/10.5435/JAAOS-20-02-094
Acknowledgments
We thank JL Guo of the Department of Orthopaedics of Statistics and Applications for their generous assistance.
Availability of data and materials
Not applicable.
Funding
The study was funded by National Key R&D Program of China (Grant No. 2019YFC0120600).
Author information
Authors and Affiliations
Contributions
YZ Z designed the study; KZ, XD L, SY T, ZZ W, and JZ Z searched relevant studies; JY L and WC analysed and interpreted the data; KZ wrote the manuscript; and YZ Z and ZY H approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Implementation of this study was agreed by the Institutional Review Board of Third Hospital of Hebei Medical University.
Consent to participate
All patients provided informed consent prior to participating.
Consent for publication
Informed consent for publication was obtained from all patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, K., Lian, X., Tian, S. et al. Traction methods in the retrograde intramedullary nailing of femur shaft fractures: the double reverse traction repositor or manual traction. International Orthopaedics (SICOT) 45, 2711–2718 (2021). https://doi.org/10.1007/s00264-021-04961-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-04961-2