Abstract
Purpose
This study aims to investigate the application value of O-arm navigation system in sacroiliac screw placement for the treatment of unstable pelvic ring injury.
Methods
A total of 40 patients (mean age = 30.75 ± 14.99 years, 25 males, 15 females) were included. From January 2016 to July 2018, 40 patients with posterior pelvic ring injury treated in our hospital were included. Of them, 19 patients underwent O-arm navigation for screw placement (O-arm group) while the other 21 received C-arm fluoroscopy guidance (C-arm group) for sacroiliac screw placement. Intraoperative outcomes and the outcome of screw placement were compared between groups. The quality of radiological images was assessed by Matta’s radiological outcome grade. The outcome of complex pelvic fracture treatment was evaluated by Majeed Functional score.
Results
All demographic and clinical characteristics were comparable between the two groups. Compared with the C-arm groups, the O-arm group had a shorter surgery time (33.19 ± 3.14 vs. 48.35 ± 4.38 min, P < 0.001), a higher overall good outcome “excellent + good” rate of screw placement (95.45% vs. 73.91%, P < 0.05), and a significantly higher Majeed Functional score better outcome of complex pelvic fracture treatment at 1 and 3 months postoperation (both P < 0.05).
Conclusion
Our results demonstrated that O-arm navigation system is feasible and safe for the treatment of posterior pelvic ring injury and can effectively improve the accuracy and safety of sacroiliac screw placement, shorten the operation time, and help rapid postoperative functional recovery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adult pelvic fractures are most commonly caused by high-energy trauma due to raid traffic accidents and fall from height [1]. Pelvic fractures are frequently associated with other complications, such as hemorrhagic shock, craniocerebral injury, and abdominal injury, with mortality ranging from 5 to 16% [2].
The current standard treatment for posterior pelvic ring injury is sacroiliac joint cannulated lag screw fixation [3], which is a method of internal fixation through the sacrum and sacrum [4]. The posterior pelvic ring injuries are usually located near the sacroiliac joint and are adjacent to important nerves, blood vessels, and abdominal organs, increasing the difficulty of surgery [5]. As a result, in the sacroiliac joint cannulated lag screw fixation, intraoperative C-arm fluoroscopy should be repeatedly taken for positioning, and the radiation exposure to both the patient and surgical staff is large [6]. In addition, the obtained images are blurry and cannot clearly show the anatomical structure around the sacroiliac joint. Especially in the presence of anatomical variation, the rate of screws malpositioning is increased [7].
It has been reported that the C-arm fluoroscopy-guided sacroiliac screw placement has a malpositioning rate of 2 to 15% and an incidence of lumbosacral nerve and hip vascular injuries of 7.7% [8]. The surgical treatment of posterior pelvic ring injury is even more challenging for young surgeons. An accurate and intuitive intraoperative fluoroscopy device is urgently needed to assist the operation and improve the safety of the operation.
The O-arm navigation system is a new generation of intraoperative imaging platform providing real-time multidimensional images for surgeries [9]. The O-arm navigation system has been adopted to assist surgeons in safe and accurate screw placement for the internal fixation of pelvic ring injuries [10, 11]. Merritt et al. have demonstrated that the application of O-arm navigation system to assist the placement of sacroiliac screw in the treatment of sacral fractures can improve the accuracy of screw placement, shorten the operation time, and reduce postoperative complications [9]. However, the studies on O-arm navigation system in the treatment for pelvic ring injury are still limited [12, 13]. The purpose of this study was to investigate the feasibility and safety of the O-arm navigation system in sacroiliac screw placement for the treatment of pelvic ring injury.
Methods
Study subjects
From January 2016 to July 2018, 40 patients with posterior pelvic ring injury treated in our hospital were included. The inclusion criteria were the following: (1) Denis classification of sacrum fracture type 1 and type 2, (2) sacroiliac joint dislocation (SIJ dislocation), (3) pelvic fracture tile classification B or C, (4) Malgaigne fracture (i.e., fractures of unilateral rami ischiopubicus or pubic symphysis, combined with extensive fractures of the sacrum, sacroiliac joint, or sacrum). The exclusion criteria included the following: (1) severe osteoporosis; (2) poorly closed reduction; (3) congenital malformations; (4) patients with severe underlying diseases, such as heart disease or pulmonary insufficiency; (5) preoperative evaluation of patients who cannot tolerate anesthesia. Of which, 19 patients undergoing O-arm navigation for screw placement were designated as the O-arm group (n = 19), while patients receiving C-arm fluoroscopy guidance were designated as the C-arm group (n = 21). This study was approved by the institutional review board of our hospital. Written informed consent was obtained from each patient.
Preoperative preparation
All patients underwent routine preoperative examinations, including electrocardiogram, blood routine test, and abdominal B-ultrasound, as well as preoperative X-ray and 64-slice spiral CT examinations of the pelvis to fully evaluate the pelvic ring injury and pelvic anatomic variations. Patients with hip dislocation received emergency hip reduction first. For patients with displaced sacroiliac joint dislocations/patella fractures, bone traction was required. Before surgery, the surgeon explained the different features of O-arm navigation system– and traditional C-arm–assisted surgeries to the patients and their families. The patients and their families chose the surgical method according to their own willingness. Surgery was performed by the same group of patients in both groups.
Surgical methods
For the O-arm navigation, the patient was placed in the supine position under general anesthesia. The anterior superior iliac spine on the affected side was identified, and a 0.5-cm incision was made. The subcutaneous tissue was bluntly separated until the anterior superior iliac bone. The referencing frame of the tracer was inserted, and the binocular infrared camera was adjusted to ensure that the reflection ball of the tracer within its camera receiving area. The O-arm 2D scan mode was used to take the front and side radiographs and confirmed that the affected sacroiliac joint and the surrounding structure of S1/S2 were in the middle of the O-arm screen. The surgical navigation equipment was connected to perform a 360° scan. The 3D reconstruction was automatically completed and transmitted to the Medtronic navigation device to complete the registration process. The tip of the instrument was used to contact the anterior superior iliac spine or pubic symphysis to verify the accuracy of the instrument corresponding to the actual anatomical structures and to prevent image drift. A 1–1.5-cm incision was made, and the subcutaneous tissue was bluntly separated until the lateral bone surface of the sacrum. The position of the virtual guide needle on the coronal, sagittal, and cross section of the target segment was observed on the screen. After selecting a proper position of the guide needle, the sacroiliac screw was inserted. Then, another 3D scan was performed to check whether the position and length of the screw are appropriate to ensure accurate screw placement. The poorly located screws should be identified in time and revised.
For the C-arm fluoroscopy, the patient was placed in the supine position under general anesthesia. The C-arm was placed on the healthy side; the anteroposterior (AP) pelvis radiograph, the standard lateral pelvic radiograph, the inlet pelvis radiograph, and the outlet pelvis radiograph were taken; and the tilt angles of the C-arm during radiographing were recorded. Under the C-arm fluoroscopy, the incision was selected based on the surgeon’s experience, combined with the patient’s body surface marks, anterior superior iliac spine, and iliac spine. The subcutaneous tissue was bluntly separated to exposes the lateral bone surface of the patella. The insertion point was about 2 cm below the intersection of the vertical line of the anterior superior iliac spine and axis of the femoral shaft. The guide needle was implanted under perspective. After confirming that there was no perforation, the screw was implanted. Finally, the AP and lateral pelvic radiographs were taken again to check if the screw position and length was appropriate.
Postoperative management
In both groups, an aerodynamic pump was applied to the affected limb to prevent deep vein thrombosis of the lower extremity. X-ray films and CT were taken 3 days after the operation. On the 1st day after the operation, the hip joint of the affected limb was moved and supplemented with massage to further prevent deep vein thrombosis of the lower extremity. The postoperative landing time and timing for functional exercises were determined based on the degree of injury and bone quality of patients after surgery.
Patients with good bone quality and posterior pelvic ring injury on the same side can stand with the aid of a walker 2 weeks after surgery, and the healthy limb can be fully weight-bearing. Partial weight bearing can be performed on the affected limb from 1 to 1.5 months, and complete weight-bearing could be considered depending on the fracture healing status at 3 months postoperation.
For patients with bilateral unstable posterior ring fractures/dislocations, X-rays or CT examinations should be performed at 3 months after surgery to assess fracture healing and weight-bearing can only be performed after fracture healing. After the posterior pelvic ring injury has completely healed, the sacroiliac screw generally does not need to be removed.
Evaluation of outcome of screw placement
In the O-arm group, immediately after the screw placement was completed, the 3D scanning was performed in the O-arm 3D scanning mode, and the sacroiliac joint screw position was evaluated using the Richter method [5] as follows: excellent, the screw was completely located in the pedicle of the sacral pedicle; good, the screw only penetrated out of the cortex of the sacral pedicle (no more than one-fourth of the screw diameter); and poor, the screw clearly penetrates the sacral pedicle (more than one-fourth of the screw diameter). Screws with a poor grade were considered to be malpositioned screws, and all were revised intraoperatively.
In the C-arm group: three-dimensional (3D) CT scan was used to evaluate sacroiliac screw placement: Siemens 64-row spiral CT thin-layer scan and 3D reconstruction were used for evaluation and were independently evaluated by three radiologists. The screw position was also evaluated by the Richter method [5].
Evaluation of reduction quality by the Matta score
Fracture reduction quality was assessed by Matta’s radiological score [14] as follows: excellent, anatomical reduction (shift < 1 mm); good, satisfactory reduction (shift < 3 mm); and poor, unsatisfactory reduction (shift > 3 mm). In the O-arm group, following the screw placement, the reduction quality can be evaluated after the 3D scanning. In the C-arm group, 3D CT scans were performed 3 days postoperation for evaluation of reduction quality.
Functional evaluation
The pelvis function was evaluated by the Majeed pelvic score [15] before surgery, 1 month after surgery, and 3 months after surgery. Majeed functional scoring system consists of several questions in seven items, including pain (30 points), standing (36 points), sitting (10 points), working ability (20 points), and sexual function (4 points), which make up the total score ranging from 0 to 100. The Majeed pelvic score of 85 to 100 points was defined as “excellent,” 70 to 84 was defined as “good,” 55 to 69 points was defined as “normal,” and 54 points and below was defined as “bad.”
Statistical analysis
Continuous data were indicated with mean ± standard deviation (SD). For the comparisons between two groups, the Student independent t test and paired t test were used for independent and repeated measurements, respectively. Two-way mixed design ANOVA was used to test the overall significance of results at preoperative, 1 month, and 3 months after operation in both groups. A P < 0.05 would be recognized as reaching the significance of each test, two-tailed. All analyses were performed using IBM SPSS Version 25 (SPSS Statistics V25, IBM Corporation, Somers, New York).
Results
Patients’ demographic and clinical characteristics
A total of 40 patients with posterior pelvic ring injury (mean age = 30.75 ± 14.99 years, 25 males, 15 females) were included, 19 patients underwent O-arm navigation for screw placement while the other 21 received C-arm fluoroscopy guidance for sacroiliac screw placement. The causes of injury included traffic accidents (n = 21, 52.50%), falling (n = 14, 35.00%), and injured by crashing objects (n = 5, 12.50%). As for the fracture pattern, 31 (77.50%) were categorized into Tile classification B and 9 (22.50%) cases were Tile classification C. The mean duration from injury to surgery was 30.75 ± 14.99 days. Patients’ demographic and clinical characteristics were summarized in Table 1. There was no significant difference in all characteristics above between the O-arm group and the C-arm group (all P > 0.05), indicating well comparability between the two groups.
Intraoperative findings
The mean surgery time was significantly shorter in the O-arm group than in the C-arm group (33.19 ± 3.14 vs. 48.35 ± 4.38 min, P < 0.001; Table 2). However, there was no significant difference in the intraoperative bleeding between the two groups (P = 0.589; Table 2).
Postoperative results
As shown in Table 2, the overall outcome of screw placement was significantly different between the two groups (P = 0.037). The overall good outcome (excellent + good) rate of screw placement was significantly higher in the O-arm group (than in the C-arm group (95.45% vs. 73.91%, P < 0.05). Fracture reduction quality was assessed by Matta’s radiological score. The result showed that the excellent + good rate was not significantly different between the O-arm group (94.74%) and the C-arm group (95.24%).
The outcome of complex pelvic fracture treatment was evaluated by Majeed Functional score. In the intragroup comparisons of both groups, the Majeed Functional score was significantly improved at 1 month and 3 months postoperation as compared with the results in preoperation (all P < 0.05; Table 2; Fig. 1). As for the intergroup comparison, the O-arm group had a significantly higher Majeed Functional score than the C-arm group at 1 month and 3 months postoperation (both P < 0.05).
Classic case
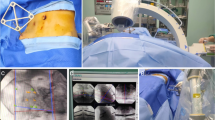
A 29-year-old female patient was admitted 1 h after a car accident. The diagnosis was a right sacral fracture and bilateral upper and lower limb fractures of the pubis (C1–3 type). Figure 2 indicates the preoperative X-ray (Fig. 2a) and CT (Fig. 2b). Intraoperative O-arm navigation was performed (Fig. 2c), and the 3D scan showed a good screw position during operation (Fig. 2d). Postoperative CT (Fig. 2e) and X-ray (Fig. 2f) showed that the screws were in good position after the operation. The patient’s pelvic function recovered well 3 months after operation (Fig. 2g).
a Preoperative X-ray showed: (1) the right sacral fracture and (2) bilateral upper and lower limb fractures of the pubis. b Preoperative CT scan showed: (1) the right sacral fracture and (2) bilateral upper and lower limb fractures of the pubis. c Implantation of the guide pin in O-arm navigation during operation. d O-arm 3D scan showed a good screw position during operation. e Postoperative CT showed the good position of the screw. f The X-ray showed that the screws were in good position after the operation. g Three months after surgery, pelvic function recovered well
Discussion
Compared with conventional intraoperative C-arm fluoroscopy navigation, the O-arm navigation system often requires less operative time [16]. The O-arm navigation system used in this study is composed of O-arm surgical fluoroscopy, display image system, and Medtronic surgical navigation system. It can complete high-quality image acquisition, 3D reconstruction, and transmission process within 60 s, and the scanned data can be directly transferred to the navigation computer for automatic matching and registration, which markedly simplifies the tedious registration procedure in other conventional computer-assisted navigation systems, such as preoperative CT navigation, intraoperative two-dimensional C-arm navigation, and intraoperative isocentric C-arm 3-dimensional navigation [17], thus further shortening the operation time. In this study, we found that the mean operation time was significantly shorter in the O-arm group than in the C-arm group. The main reason is that the O-arm navigation system can intraoperatively acquire high-quality images within only 13 s and complete the 3D reconstruction within 30 s. The registration is automatically completed after connecting to the Medtronic navigation system. After the image transmission, the relative positional relationship between the surgical instrument and the important anatomical structures (such as sacral pedicle, spinal canal, anterior iliac foramen, vertebral body) can be directly displayed. This allows the operation to be performed “under direct view,” and repeated fluoroscopy guidance is unneeded, avoiding inducing damages to important nerves, blood vessels, and other physiological anatomical structures, thereby shortening the screw placement time, improving the accuracy of screw placement, and reducing complications.
It has been shown that O-arm navigation system can improve the accuracy of iliosacral screw placement and reduction of screw malposition [3, 18]. In addition, O-arm navigation system has been shown to reduce the rate of screw malposition for less experienced surgeons [19, 20]. Supporting these findings, our results found that in the O-arm group, the overall good outcome rate (excellent + good) of sacroiliac screws placement was 95.45%. There were no cannulated lag screws penetrating the sacral pedicle or the cortex of the sacral vertebra into the sacral canal or pelvis. In the C-arm group, the overall good outcome rate of screw placement was 73.91%, which was significantly lower than that of the O-arm group. In the C-arm group, 6 patients (26.09%) had poor screw placement, as the poor screw placement could be identified only by postoperative 3D CT scan. By contrast, the O-arm group had only one case (4.55%) of poor screw placement, and the case should be attributed to that the surgical assistant accidentally hit the referencing frame, leading to image drift and then screws malposition. Maintaining stability of referencing frame and patient position during operation are important prerequisites for accurate screw placement of O-arm navigation. The loose or displacement of the referencing frame or the change of the patient’s pelvic position will cause the image drift, resulting in screw malposition.
O-arm combined with the Medtronic navigation system can achieve highly visualizable screw placement in a real-time manner, avoiding the inaccuracies caused by anatomical variations or variations in the surgeon’s hand feeling based on traditional C-arm positioning. This result suggested that in the sacroiliac screw placement, the intraoperative O-arm navigation system is more accurate than the C-arm navigation. The O-arm navigation system can intraoperatively re-perform a 3D scan of the surgical site immediately after completing screw placement, and the malpositioned screws can be revised or removed in time to avoid reoperation.
In both groups of this study, the volume of intraoperative bleeding ranged from 11 approximately to 25 mL, and no significant difference was observed between the two groups. The surgical procedures of both groups belonged to closed screw placement, the surgical incisions were about 1 cm, and the percutaneous implantation reduces the damage to the muscles, the nerves, and the ligaments around the sacroiliac joint. The amounts of intraoperative bleeding of both groups were relatively small, meeting the standard of minimally invasive surgery. As for the postoperative complications, no obvious neurological symptoms occurred in the O-arm group, whereas 2 cases had numbness and predehydration in the left lower extremity after surgery, which were resolved by symptomatic treatments, such as hormone and nutritional nerve treatment for 3 months. In the C-arm group, 3 patients showed postoperative nerve root injury, and the symptoms improved significantly after 3–6 months of treatment. One patient had screw displacement that required removal and reinsertion. On the other hand, in most cases with O-arm navigation system, screw placement can be completed with a single scan, and the radiation exposure to the surgeon and patient is low [21], further increasing the safety of the operation.
Guo et al. have studied on pedicle screw implantation in bovine lumbar spine specimens using the O-arm navigation system and found that the movement of bovine spine specimens and loose referencing frame may induce changes in the relative position in the 3D images, causing screw malposition [22]. Before each insertion of the guide needle, an intelligently certified sleeve must be used to contact body surface landmarks, such as the anterior superior iliac spine or the pubic symphysis, to verify whether the navigation image indeed corresponds to the actual anatomical landmark and determine whether rescan is needed based on surgeon’s clinical experience and anatomy knowledge. In addition, the referencing frame should be fixed as close as possible to the operation area (the needle entry point on the outside of the sacrum), because the referencing frame too far away from the operation area will also cause image drift. A study on O-arm navigation system–assisted spinal pedicle screw placement has revealed that the referencing frame too far from the vertebral body of the target segment will increase the risk of pedicle perforation [23]. Placing the infrared camera system on the healthy side can reduce the smart infrared camera system from being blocked by front objects and reduce the number of times to adjust the navigation position to find the signal of the reflection ball, thus effectively shortening the operation time. In this study, the O-arm group had a significantly higher Majeed Functional score than the C-arm group at 1 month and 3 months postoperation, implying a better postoperative functional recovery in the O-arm navigation system for the sacroiliac screw placement as compared with the C-arm fluoroscopy guidance.
The 3D scanning of the O-arm navigation system has a higher dose of radiation exposure than ordinary X-ray fluoroscopy [24]. To minimize the radiation dose in the O-arm system, Su et al. have reported that the fluoroscopy dose of the O-arm for pediatric can be reduced by larger than 75% without impacting the image quality to guide the screw placement and the accuracy of screw placement [25]. Kassis et al. have proposed a protocol of combining pedicle screw stimulation with spinal navigation to reduce radiation exposure in thoracolumbar spine instrumentation [26]. After screw placement, the pedicle screw-induced electromyography can be used to determine the screw position. If there are no abnormalities in the electromyography, O-arm 3D scanning is not required after screw placement.
There are still some limitations of this study. First, the doctor’s learning curve may have some impact on the results. In addition, the sample size of this study was small, and the follow-up duration was short. Moreover, we did not measure the exact radiation exposure of the O-arm navigation and C-arm fluoroscopy in this study. All these limitations should be addressed in the future. A well-designed prospective trial should be conducted to verify the findings of the current study.
Conclusions
In summary, our results demonstrated that compared with conventional C-arm fluoroscopy, O-arm navigation can effectively improve the accuracy and safety of sacroiliac screw placement, shorten the operation time, and provide reliable internal fixation, meeting the concepts of minimally invasive medical and precision medicine and helping rapid postoperative functional recovery.
References
Ghosh S, Aggarwal S, Kumar V et al (2019) Epidemiology of pelvic fractures in adults: our experience at a tertiary hospital. Chin J Traumatol 22:138–141. https://doi.org/10.1016/J.CJTEE.2019.03.003
Saxena P, Agrawal A, Sakale H (2014) Introduction to pelvic injury and its acute management. J Orthop Traumatol Rehabil 7:1. https://doi.org/10.4103/0975-7341.133995
Richter PH, Gebhard F, Dehner C, Scola A (2016) Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 47:402–407. https://doi.org/10.1016/j.injury.2015.11.023
Briem D, Linhart W, Lehmann W et al (2006) Computer-assisted screw insertion into the first sacral vertebra using a three-dimensional image intensifier: results of a controlled experimental investigation. Eur Spine J 15:757–763. https://doi.org/10.1007/s00586-005-0992-5
Zwingmann J, Konrad G, Kotter E et al (2009) Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin Orthop Relat Res 467:1833–1838. https://doi.org/10.1007/s11999-008-0632-6
De Silva T, Punnoose J, Uneri A et al (2018) Virtual fluoroscopy for intraoperative C-arm positioning and radiation dose reduction. J Med Imaging 5:1. https://doi.org/10.1117/1.JMI.5.1.015005
Zwingmann J, Hauschild O, Bode G et al (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133:1257–1265. https://doi.org/10.1007/s00402-013-1788-4
Moed BR, Ahmad BK, Craig JG et al (1998) Intraoperative monitoring with stimulus-evoked electromyography during placement of iliosacral screws: an initial clinical study. J Bone Jt Surg - Ser A 80:537–546. https://doi.org/10.2106/00004623-199804000-00010
Liu Z, Jin M, Qiu Y et al (2016) The superiority of intraoperative O-arm navigation-assisted surgery in instrumenting extremely small thoracic pedicles of adolescent idiopathic scoliosis. Medicine (Baltimore) 95:e3581. https://doi.org/10.1097/MD.0000000000003581
Rosenberger RE, Dolati B, Larndorfer R et al (2010) Accuracy of minimally invasive navigated acetabular and iliosacral fracture stabilization using a targeting and noninvasive registration device. Arch Orthop Trauma Surg 130:223–230. https://doi.org/10.1007/s00402-009-0932-7
Behrendt D, Mütze M, Steinke H et al (2012) Evaluation of 2D and 3D navigation for iliosacral screw fixation. Int J Comput Assist Radiol Surg 7:249–255. https://doi.org/10.1007/s11548-011-0652-7
Coste C, Asloum Y, Marcheix PS et al (2013) Percutaneous iliosacral screw fixation in unstable pelvic ring lesions: the interest of O-ARM CT-guided navigation. Orthop Traumatol Surg Res 99:S273–S278. https://doi.org/10.1016/j.otsr.2013.03.002
Ghisla S, Napoli F, Lehoczky G et al (2018) Posterior pelvic ring fractures: intraoperative 3D-CT guided navigation for accurate positioning of sacro-iliac screws. Orthop Traumatol Surg Res 104:1063–1067. https://doi.org/10.1016/j.otsr.2018.07.006
Hsu AR, Lee S (2014) Evaluation of tarsal navicular stress fracture fixation using intraoperative O-arm computed tomography. Foot Ankle Spec 7:515–521. https://doi.org/10.1177/1938640014532130
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Jt Surg - Ser B 71:304–306. https://doi.org/10.1302/0301-620x.71b2.2925751
Qureshi S, Lu Y, McAnany S, Baird E (2014) Three-dimensional intraoperative imaging modalities in orthopaedic surgery: a narrative review. J Am Acad Orthop Surg 22:800–809
He J, Tan G, Zhou D et al (2016) Comparison of isocentric C-arm 3-dimensional navigation and conventional fluoroscopy for percutaneous retrograde screwing for anterior column fracture of acetabulum: an observational study. Medicine (Baltimore) 95:e2470. https://doi.org/10.1097/MD.0000000000002470
Takao M, Nishii T, Sakai T et al (2014) Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury 45:988–994. https://doi.org/10.1016/j.injury.2014.01.015
Verma SK, Singh PK, Agrawal D et al (2016) O-arm with navigation versus C-arm: a review of screw placement over 3 years at a major trauma center. Br J Neurosurg 30:658–661. https://doi.org/10.1080/02688697.2016.1206179
Takao M, Nishii T, Sakai T, Sugano N (2013) CT-3D-fluoroscopy matching navigation can reduce the malposition rate of iliosacral screw insertion for less-experienced surgeons. J Orthop Trauma 27:716–721. https://doi.org/10.1097/BOT.0b013e31828fc4a5
Grelat M, Zairi F, Quidet M et al (2015) Assessment of the surgeon radiation exposure during a minimally invasive TLIF: comparison between fluoroscopy and O-arm system. Neurochirurgie 61:255–259. https://doi.org/10.1016/j.neuchi.2015.04.002
Guo N, Zhang H, Li J et al (2013) O-arm based navigation vs X-ray fluoroscopy in accuracy of pedicle drilling in bovine lumber spine specimens. J Third Mil Med Univ 35:277–279
Tow BPB, Yue WM, Srivastava A et al (2015) Does navigation improve accuracy of placement of pedicle screws in single-level lumbar degenerative spondylolisthesis? A comparison between free-hand and three-dimensional o-arm navigation techniques. J Spinal Disord Tech 28:E472–E477. https://doi.org/10.1097/BSD.0b013e3182a9435e
Pitteloud N, Gamulin A, Barea C et al (2017) Radiation exposure using the O-arm® surgical imaging system. Eur Spine J 26:651–657. https://doi.org/10.1007/s00586-016-4773-0
Su AW, Luo TD, McIntosh AL et al (2016) Switching to a pediatric dose O-arm protocol in spine surgery significantly reduced patient radiation exposure. J Pediatr Orthop 36:621–626. https://doi.org/10.1097/bpo.0000000000000504
Kassis SZ, Abukwedar LK, Msaddi AK et al (2016) Combining pedicle screw stimulation with spinal navigation, a protocol to maximize the safety of neural elements and minimize radiation exposure in thoracolumbar spine instrumentation. Eur Spine J 25:1724–1728. https://doi.org/10.1007/s00586-015-3973-3
Acknowledgments
We are grateful for the help from Professor Tan Haitao who is the secretary of the hospital’s party committee and the chief physician of orthopedics, as well as the help from the team of orthopedic surgeons.
Funding
This study is supported by the Inversion and Application of Scientific and Technical Payoffs of Guigang, Guangxi Province (GKZ 1701002), Guangxi Science and Technology Project (AD17129017, AD17195042), Guangxi Natural Science Foundation Project (2018GXNSFAA294129), the Key Clinical Specialty Construction Projects in Guangxi Zhuang Autonomous Region, and Guigang Scientific Research and Technology Development Projects (GKT 1834002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review board of our hospital. Written informed consent was obtained from each patient.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lu, S., Yang, K., Lu, C. et al. O-arm navigation for sacroiliac screw placement in the treatment for posterior pelvic ring injury. International Orthopaedics (SICOT) 45, 1803–1810 (2021). https://doi.org/10.1007/s00264-020-04832-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04832-2