Abstract
Purpose
The main aim of this study was to investigate the correlation between radiographic findings and clinical outcomes following the first metatarsophalangeal (MTP) joint arthrodesis.
Methods
In a comparative retrospective study, on 46 patients (48 ft), the correlation between post-operative radiographic findings including hallux valgus angle (HVA) and first MTP dorsiflexion angle (MTPDA) and clinical outcomes including VAS pain, modified AOFAS hallux score, and FFI questionnaire were evaluated. Moreover, clinical outcomes were compared between cases with pre-operative diagnosis of first MTP inflammatory arthritis, hallux valgus, hallux varus, and grade 3 and 4 of hallux rigidus. The effect of first MTP arthrodesis on Meary’s angle and intermetatarsal angle (IMA) were found out.
Results
The mean age of the patients was 56.3 ± 9.1 (range, 29–69) years, including 42 (91.3%) females and 4 (8.7%) males. We had fusion rate of 97.9%, one asymptomatic nonunion case (2.1%). Totally, mean scores of modified AOFAS hallux score, FFI percentage, and VAS pain were 88.9 ± 12.6, 9.4 ± 16.5, and 1.23 ± 2.24, respectively. Hallux varus was associated with the most favourable outcomes; whereas, patients with first MTP arthritis got the worst outcome. Regression analysis test between clinical outcomes and HVA > 15° and first MTPDA >15° showed correlation coefficient of almost zero. No statistically significant differences were found between the clinical outcomes of grade 3 and 4 of hallux rigidus (p value of modified AOFAS hallux score, FFI percentage, and VAS pain: 0.879, 0.906, and 0.298, respectively). Mean of HVA and IMA reduction in 15 hallux valgus underwent first MTP fusion were 34.4° and 8.4°, respectively. Meary’s angle increased about 4° with statistically significant difference (p value 0.001).
Conclusion
Patients with first MTP fusion > 15° in coronal and transverse plans could have acceptable clinical outcomes. The clinical outcome of first MTP arthrodesis for grade 3 hallux rigidus is comparable with grade 4. First MTP fusion would have positive effect on IMA and Meary’s angle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first metatarsophalangeal (MTP) joint arthropathy is a common disorder among referred patients to the foot and ankle clinics. These patients complain of chronic forefoot pain, reduced range of motion of the big toe, decreased activities of daily living, and difficulty to find suitable shoes [1]. Arthrodesis of the first MTP joint is a well-established procedure for treating patients with destructive inflammatory joint diseases like rheumatoid arthritis or gouty arthritis, advanced hallux rigidus, severe hallux valgus with arthritic changes, unreconstructible hallux varus deformity, old dislocated 1st MTP joint, and neuromuscular conditions as well as a salvage procedure for a failed first MTP arthroplasty [2,3,4,5]. Successful arthrodesis has been achieved by various fixation methods [6, 7].
In recent years, the literature has witnessed ongoing interest in evaluation of outcomes following the first MTP joint arthrodesis [8]. Majority of these studies have focused only on one patient group such as hallux valgus or hallux varus [5, 9,10,11,12,13]. Most of available researches in this line, however, have been concentrated on the changes of different angles such as intermetatarsal angle (IMA) following the first MTP arthrodesis [5, 12,13,14,15,16]. Moreover, to the best of our knowledge, there are only few studies which have demonstrated the correlation between clinical foot function and hallux position after first MTP fusion [17, 18].
The main aim of the presented study was to investigate the correlation between post-operative radiographic findings and clinical outcomes of the patients following first MTP arthrodesis, especially in cases fused in more than the angle limitation in sagittal and transverse planes. In other words, what would be clinically happened to the patients if the first MTP had been fused in hallux valgus angle (HVA) more than 15° and/or first MTP dorsiflexion angle (MTPDA) more than 15°. The other goal was to compare the functional outcomes of the first MTP arthrodesis based on the different primary diagnoses including grade 3 and 4 hallux rigidus, inflammatory destructive arthropathies, hallux valgus, and hallux varus. Moreover, we would like to find the changes in HVA and IMA in hallux valgus cases after first MTP fusion and its effect on Meary’s angle.
Materials and methods
After approval of the study by the ethic committee of our university in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its later amendments (IR.SUMS.MED.REC.1397.519), in a cross-sectional comparative retrospective study, all consecutive patients that underwent first MTP joint arthrodesis by the senior author (ARV) between July 2015 and December 2018 were approached for eligibility. Indications for first MTP arthrodesis were grade 3 hallux rigidus with > 50% cartilage loss, grade 4 hallux rigidus, first MTP inflammatory arthropathies with severe joint destruction without involvement of other lesser toes, hallux valgus combined with lesser toes deformities in rheumatoid forefoot, severe hallux valgus or varus deformities associated with degenerative arthritis, fixed unreconstructible hallux varus deformities, and hallux valgus in neuromuscular diseases like cerebral palsy.
Exclusion criteria were refusal to give informed consent for participating in the study, any neurodegenerative disorder leading to a sensory deficit, and any history of trauma or surgery of the foot and ankle. All patients were contacted to have a follow-up visit, at least six months following the surgery.
Demographic characteristics, primary diagnosis, surgical fixation method, additional procedures done at the time of first MTP joint arthrodesis, and post-operation complications were compiled from the patients’ files.
Surgical technique
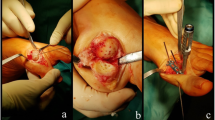
In brief, all cases were operated in supine position with inflation of a thigh tourniquet. Through medial longitudinal approach to the first MTP joint, after medial capsulotomy and resection of synovium and osteophytes, the articular surface was prepared for arthrodesis using curve osteotomes. After drilling the first metatarsal head and the proximal phalanx articular surfaces, the position of big toe for arthrodesis was adjusted and fixed using a k-wire from distal medial through the proximal phalanx to proximal lateral in the first metatarsal. It was tried to have a HVA of 15° in transverse plane and first MTPDA of 15° in sagittal plane without any rotation in the frontal plane. In order to achieve first MTPDA of 15°, a flat metal surface was placed beneath the sole of the foot in neutral position of the ankle joint. The tip of the big toe should touch the metal plate with possibility to have dorsiflexion through interphalangeal joint. Because adjustment of the first MTP fusion position is an experimental surgical technique, post-operative inaccuracies may be seen. Often, two crossing screws were used to fix the arthrodesis, except in cases with severe osteoporosis or bone loss for whom 3 screws or a cross screw and dorsal locking plate were used. It should be mentioned that no adductor tenotomy was done for all 48 operated feet.
Clinical evaluation
All patients were interviewed and physically examined. The following tools were used in order to assess the clinical outcomes:
-
a.
A subjective yes/no satisfaction question about the operation.
-
b.
Visual analogue scale (VAS) pain, scoring by “no pain” and “pain as bad as it could be” from 0 to 10 [19].
-
c.
The reliable translated Persian version of the American Orthopaedic Foot and Ankle Society’s (AOFAS) hallux metatarsophalangeal-interphalangeal score (AOFAS hallux) [20], evaluating patient’s pain, function (including activity limitations, footwear requirements, MTP and IP joint motion, MTP-IP stability, callus related to hallux MTP-IP), and hallux alignment. Since the first MTP joint motion is eliminated by the arthrodesis, this scale was modified by exclusion of the ten related points and maximum score of 90 was normalized to 100. The physical examinations were done by two authors independently and the average of the measurements was used as the final values.
-
d.
Foot function index (FFI) was designed to measure foot function in subscales of pain, disability, and activity restrictions by 23 subjective questions. The scale is from 0 as the best functional condition of the foot to 100 as the worst, adapted to percentile report in our study [21].
Radiographic evaluation
On the pre-operative and the last follow-up weight-bearing plain radiographs of the patients, HVA and IMA in dorsoplantar view and also Meary’s angle and first MTPDA in lateral view were measured by the other author based on the American Orthopaedic Foot & Ankle Society on angular measurements (Fig. 1) [22, 23]. Furthermore, the assessment of tibial sesamoid position was conducted in dorsoplantar view relative to the first metatarsal longitudinal bisection using Hardy and Clapham’s classification, scoring from 0 to 7 [24].
Statistical analysis
Statistical analysis was performed using the statistical package for the social sciences version 16.0 for windows (SPSS Inc. Chicago, IL, USA). Descriptive data such as demographics, clinical outcomes, and radiographic findings were expressed as frequency, mean, and standard deviation. Paired sample t test and its non-parametric equivalent were employed to evaluate the significance of the difference between pre- and post-operative radiological findings.
Patients were categorized into two groups based on HVA and also MTPDA (greater and lesser than 15°). Clinical findings were compared between the groups using Mann-Whitney U test. The alpha level was set at 0.05. Moreover, in order to estimate the relationship between post-operative clinical outcomes and HVA and MTPDA > 15°, regression analysis was used to find the correlation coefficient.
Results
From 57 patients underwent first MTP fusion, eleven patients were not joined the project: one died due to cardiovascular disorder, one wheelchair-bound case with diagnosis of multiple sclerosis, two patients migrated to another city or country, two subjects were unavailable without accurate contact address, and five patients refused to participate.
Finally, 46 patients with mean age of 56.3 ± 9.1 (range, 29–69) years, including 42 (91.3%) females and four (8.7%) males were enrolled. As two women underwent bilateral first MTP fusion, 48 feet were studies (right, 29 and left, 19). Mean follow-up visit for the patients was 21.7 ± 11.8 (range, 6–45) months.
Of the 46 patients, 15 had underlying diseases: one had Behcet’s disease, one had diabetes mellitus, and 13 had rheumatoid arthritis (RA). The most common primary diagnosis was hallux rigidus (23 ft), followed by rheumatoid arthritis (14 ft: 9 hallux valgus with lesser metatarsal rheumatoid deformities and 5 first MTP destructive inflammatory arthropathies), hallux valgus (6 ft), hallux varus (3 ft: one idiopathic, one with old traumatic subluxation of the first MTP joint, one case of old fracture disruption of medial sesamoid), and cerebral palsy (2 cases). Among 23 ft with primary diagnosis of hallux rigidus, there were 15 females of grade 3 with mean age of 57.4 years. Hallux rigidus grade 4 was the primary diagnosis of eight feet, five females and two males, one bilateral.
Fixation methods for arthrodesis included two cross screws for 40 feet, three cross screws for three feet, and a screw and dorsal locking compression plate for five rheumatoid feet. Bone graft was impacted in the site of first MTP fusion for 31 out of the 48 (64.6%) operated feet; one of them was harvested from resected second and third metatarsal head during resection arthroplasty procedure and all the others from the calcaneus. For 21 patients, additional surgical procedures for lesser metatarsal bones including arthrodesis of proximal interphalangeal joint, flexor to extensor tendon transfer, weil osteotomy, extensor tendon tenotomy, resection arthroplasty, Morton neuroma excision, and gastrocnemius recession were done at the same time.
Of the 48 feet underwent first MTP fusion, four (8.3%) showed a post-operation complication: one case of superficial infection with wound healing disturbances responsive to dressing change and oral antibiotic, one hardware removal due to pain and foreign body sensation, one deep vein thrombosis treated by anticoagulant medications, and one case of asymptomatic radiologic nonunion without needing a revision surgery with primary diagnosis of hallux rigidus grade 3 (Fig. 2).
Post-operative outcomes
Totally, satisfaction rate was 93.8% with only three unsatisfied patients. Scores of modified AOFAS hallux, FFI, and VAS pain are shown in Table 1. It should be mentioned that in tables, first MTP arthritis includes hallux rigidus in addition to destructive rheumatoid arthritis without valgus or varus deformities. Hallux varus was associated with the most favourable outcomes, based on the mean scores of modified AOFAS hallux, FFI percentage, and VAS pain. Notably, patients with first MTP arthritis got the worst outcome due to their higher VAS and FFI scores in comparison with other primary diagnosis; however, overall they were excellent. Mean scores of modified AOFAS hallux score were similar for first MTP arthritis and hallux valgus.
Pre- and post-operative radiographic values of all cases are summarized in Tables 2 and 3. Post-operative − 6.8° of HVA was for a nonflexible hallux varus case with pre-operative HVA of − 25.5°. Comparison of the pre-operative radiographic findings with post-operation values indicated that HVA, IMA, and Meary’s angles reduced significantly while first MTPDA were significantly increased.
Table 4 shows pre- and post-operative radiographic values in 15 ft with hallux valgus. As predicted, mean of HVA and IMA reduction in cases with hallux valgus underwent first MTP fusion were 34.4° and 8.4°, respectively.
Meary’s angle changes based on the pre-operation diagnosis are presented in Table 5. Meary’s angle increased in all cases with statistically significant difference (p value 0.001). In the other word, first MTP arthrodesis can correct longitudinal arch of the foot by 3 to 4°.
As illustrated in Table 6, there is no statistically significant difference between the cases with HVA ≥ 15° and HVA < 15° and also between case with first MTPDA ≥ 15° and first MTPDA < 15° for all clinical outcome measurements (p value > 0.05). Furthermore, regression analysis test between clinical outcomes and HVA and first MTPDA more than 15° showed correlation coefficient of almost zero (Table 7). Scatterplot graph of clinical outcome scores revealed no any correlation between reduction in clinical outcomes and increased HVA and first MTPDA (Figs. 3 and 4); however, the maximum values for HVA and first MTPDA were 25.1° and 32.6°, respectively.
We found no statistically significant differences between clinical outcome of grade 3 and 4 hallux rigidus, as shown in Table 8.
Discussion
First MTP joint arthrodesis is a safe and effective treatment for cases with first MTP hallux rigidus, inflammatory arthropathies or severe varus, or valgus deformities with low complication rates. Wholly, we had fusion rate of 97.9% with one asymptomatic fibrous nonunion (2.1%). This is superior to average fusion rate of about 90 to 95%, as previously reported in the literature [10, 25,26,27,28]. Our higher union rate may be due to use of bone graft in 64.6% of cases. As we used osteotome to resect remnant of cartilages, we had to use autograft in cases with irregularity in the matching surfaces of metatarsal head and proximal phalanx base. The other important point is using two or three cheap 3.5-mm cortical screws to fix the first MTP arthrodesis for 43 feet instead of expensive plates, as we had to use these locking plates for five rheumatoid osteoporotic feet.
The literature review showed that previous studies about radiographic findings of the first MTP arthrodesis has focused on the IMA correction following arthrodesis in patients with hallux valgus deformity [13, 15, 29]. Our findings showed a mean IMA decrease of 3.7° in all cases and 8.4° in 15 cases with hallux valgus, which could be exactly the same as 8.22° reported by Cronin et al. [29] and 8.3° described by McKean et al. [13]. The main structure resulted in reduction in IMA after first MTP arthrodesis is the intact adductor of big toe. Moreover, mean HVA change was 34.4°, similar to 36.4° reported previously [13].
The alignment of the big toe is essential for weight bearing during gait cycles and to balance the physiologic load pressure between metatarsal bones. So, any malalignment could result in difficulties in shoe wearing, lateral metatarsalgia, and possible big toe interphalangeal joint arthritis [2]. Our primary purpose to perform this study was to determine the importance of the literature-defined radiographic angles for first MTP arthrodesis in the clinical outcomes. As mentioned in Table 2, the mean of pre-operative first MTPDA was 16.1°, the normal and expected angle that should be achieved during first MTP arthrodesis surgery, but we had more mean post-operative first MTPDA (20.7°). This means that adjusting the first MTPDA during first MTP fusion surgery with a flat steel plate may result in overestimation of dorsiflexion of the big toe; whereas, the clinical results can be acceptable. Doeselaar et al. [17] found out that there is no correlation between the hallux position and the final clinical outcomes by assessing 62 cases after first MTP fusion (median FFI 8; range 0 to 59). Notably, they had post-operative first MTPDA range of 7 to 45° and HVA range of − 2 to 33°. Mann and Oates [18] had mean of post-operative first MTPDA 31° (range, 15–44°) and HVA 15° (range, 0–33°) by reviewing 41 first MTP fusion. They did not approve any correlation between the post-fusion position of the great toe and the patient’s evaluation of the surgical procedure. They did not use any validated score for assessing foot function. Our maximum post-operative angles were fewer (first MTPDA range, 3 to 32° and HVA, − 7 to 25°). In our study, there was no significant difference between patients with HVA or first MTPDA ≥ 15° and cases with HVA or first MTPDA < 15°, regarding final clinical outcomes.
In this study, we have categorized the patients into three groups based on the primary diagnosis; hallux valgus, hallux varus, and first MTP arthritis includes hallux rigidus in addition to destructive rheumatoid arthritis without valgus or varus deformities. We decided to combine hallux rigidus and inflammatory arthropathies without deformities because of the nature of both diseases as a joint destructive disease. The results indicated that patients with first MTP arthritis got the worst scores in FFI percentage and VAS pain post-operatively. On the other hand, hallux varus cases had the highest scores, although we had only three cases of hallux varus. The patients with hallux varus deformity may have the best final result because they can get rid of painful range of motion besides an unpleasant deformity. In contrary to our results, a previous study compared the first MTP arthrodesis outcomes in hallux valgus and hallux rigidus patients and concluded no significant differences between them [17]. Korim and Allen [30] categorized the 116 patients who underwent first MTP arthrodesis into four groups including hallux valgus, hallux rigidus, inflammatory arthropathy, and salvage surgery. They reported hallux valgus cases are associated with higher nonunion rates in comparison with the other groups. Based on our results, first MTP arthrodesis would be an excellent option for specific types of hallux valgus deformity without nonunion; however, the routine surgical techniques for hallux valgus correction are surgical soft tissue release and different kinds of open or minimally invasive osteotomies [31,32,33,34,35].
The strengths of the presented study are performing all surgeries by a single orthopaedic foot and ankle surgeon using screws as the constant fixation method in all patients except osteoporotic rheumatoid cases. This leads to a prevention from the common technical bias in previous studies, evaluating the first MTP arthrodesis outcomes done by multiple surgeons [8, 9, 36]. Also, there were some limitations. First, having only three cases of hallux varus made the results difficult to be generable for this group of patients. The study was designed to assess the relationship between the post-operative radiographic findings and clinical outcomes, not the improvement from the arthrodesis, as it has previously been discussed and established very well in the literature by comparing pre-operative to post-operative scores [9,10,11, 27].
In conclusion, we found out that first MTP arthrodesis has a positive effect on IMA and Meary’s angle. Moreover, this study can illustrate that the first MTP arthrodesis, in a variety of primary diagnoses, can lead to a high patient satisfaction with fusion rate of more than 95% and excellent clinical outcomes. The study showed that clinical outcomes of the patients with post-operative HVA ≥ 15° and HVA < 15° are similar. Furthermore, patients with first MTP fusion ≥ 15° in coronal and transverse plans could have acceptable clinical outcomes, albeit the maximum post-operative HVA and first MTPDA should be less than 25° and 32°, respectively.
References
Bergin SM, Munteanu SE, Zammit GV, Nikolopoulos N, Menz HB (2012) Impact of first metatarsophalangeal joint osteoarthritis on health-related quality of life. Arthritis Care Res 64:1691–1698
Fuhrmann RA (2011) First metatarsophalangeal arthrodesis for hallux rigidus. Foot Ankle Clin 16:1–12
Little JB (2014) First metatarsophalangeal joint arthrodesis in the treatment of hallux valgus. Clin Podiatr Med Surg 31:281–289
Womack JW, Ishikawa SN (2009) First metatarsophalangeal arthrodesis. Foot Ankle Clin 14:43–50
Geaney LE, Myerson MS (2015) Radiographic results after hallux metatarsophalangeal joint arthrodesis for hallux varus. Foot Ankle Int 36:391–394
Harris E, Moroney P, Tourné Y (2017) Arthrodesis of the first metatarsophalangeal joint—a biomechanical comparison of four fixation techniques. Foot Ankle Surg 23:268–274
Maleki F, Ramesh A, Cassar-Gheiti AJ, Fox C, Kelly P, Stephens MM, McKenna JV (2019) Comparison of 4 different techniques in first metatarsophalangeal joint arthrodesis. Ir J Med Sci 188:885–891. https://doi.org/10.1007/s11845-018-01961-x
Latif A, Dhinsa BS, Lau B, Abbasian A (2019) First metatarsophalangeal fusion using joint specific dorsal plate with interfragmentary screw augmentation: clinical and radiological outcomes. Foot Ankle Surg 25:132–136
DeSandis B, Pino A, Levine DS, Roberts M, Deland J, O’Malley M, Elliott A (2016) Functional outcomes following first metatarsophalangeal arthrodesis. Foot Ankle Int 37:715–721
Chraim M, Bock P, Alrabai HM, Trnka H-J (2016) Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int Orthop 40:2401–2408
Stevens J, de Bot RT, Hermus JP, van Rhijn LW, Witlox AM (2017) Clinical outcome following total joint replacement and arthrodesis for hallux rigidus: a systematic review. JBJS Rev 5:e2
Alentorn-Geli E, Gil S, Bascuas I, Donaire MF, Boza R, Pidemunt G, Puig L, Zabala S, Ginés-Cespedosa A (2013) Correlation of dorsiflexion angle and plantar pressure following arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int 34:504–511
McKean RM, Bergin PF, Watson G, Mehta SK, Tarquinio TA (2016) Radiographic evaluation of intermetatarsal angle correction following first MTP joint arthrodesis for severe hallux valgus. Foot Ankle Int 37:1183–1186
Dalat F, Cottalorda F, Fessy M-H, Besse J-L (2015) Does arthrodesis of the first metatarsophalangeal joint correct the intermetatarsal M1M2 angle? Analysis of a continuous series of 208 arthrodeses fixed with plates. Orthop Traumatol Surg Res 101:709–714
Costa MT, Neto DLL, Kojima FH, Ferreira RC (2015) Evaluation of the intermetatarsal angle after the arthrodesis of the first metatarsophalangeal joint for treatment of the hallux valgus. Rev Bras Ortop 47:363–367
Sung W, Kluesner AJ, Irrgang J, Burns P, Wukich DK (2010) Radiographic outcomes following primary arthrodesis of the first metatarsophalangeal joint in hallux abductovalgus deformity. J Foot Ankle Surg 49:446–451
Doeselaar DJ, Heesterbeek PJ, Louwerens JWK, Swierstra BA (2010) Foot function after fusion of the first metatarsophalangeal joint. Foot Ankle Int 31(8):670–675
Mann RA, Oates JC (1980) Arthrodesis of the first metatarsophalangeal joint. Foot Ankle 1:159–166
Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK (2019) A systematic review of the outcome evaluation tools for the foot and ankle. Foot Ankle Spec 12(5):461–470
Mahdaviazad H, Kardeh B, Vosoughi AR (2020) American Orthopedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal Joint Scale: a cross-cultural adaptation and validation study in the Persian language. J Foot Ankle Surg 59:729–732. https://doi.org/10.1053/j.jfas.2020.01.006
Mousavian A, Mohammadi A, Seyed-Hosseinian S-H, Shahpari O, Elahpour N, Orooji A, Ebrahimzadeh MH, Moradi A (2019) Reliability and validity of the Persian version of the foot function index in patients with foot disorders. Arch Bone Jt Surg 7:291–296
Lamm BM, Stasko PA, Gesheff MG, Bhave A (2016) Normal foot and ankle radiographic angles, measurements, and reference points. J Foot Ankle Surg 55:991–998
Coughlin MJ, Saltzman CL, Nunley JA (2002) Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int 23:68–74
Hardy RH, Clapham JC (1951) Observations on hallux valgus; based on a controlled series. J Bone Joint Surg (Br) 33-B:376–391
Coughlin MJ (1990) Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics 13:1037–1044
Baumhauer JF, Singh D, Glazebrook M, Blundell C, De Vries G, Le IL, Nielsen D, Pedersen ME, Sakellariou A, Solan M (2016) Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int 37:457–469
Wanivenhaus F, Espinosa N, Tscholl PM, Krause F, Wirth SH (2017) Quality of early union after first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg 56:50–53
Korim MT, Mahadevan D, Ghosh A, Mangwani J (2017) Effect of joint pathology, surface preparation and fixation methods on union frequency after first metatarsophalangeal joint arthrodesis: a systematic review of the English literature. Foot Ankle Surg 23:189–194. https://doi.org/10.1016/j.fas.2016.05.317
Cronin JJ, Limbers JP, Kutty S, Stephens MM (2006) Intermetatarsal angle after first metatarsophalangeal joint arthrodesis for hallux valgus. Foot Ankle Int 27:104–109. https://doi.org/10.1177/107110070602700206
Korim MT, Allen PE (2015) Effect of pathology on union of first metatarsophalangeal joint arthrodesis. Foot Ankle Int 36:51–54. https://doi.org/10.1177/1071100714549046
Seo JH, Lee HS, Choi YR, Park SH (2020) Distal chevron osteotomy with lateral release for moderate to severe hallux valgus patients aged sixty years and over. Int Orthop 44:1099–1105. https://doi.org/10.1007/s00264-020-04562-5
Montiel V, Suárez Á, Riera L, Villas C, Alfonso M (2020) Akin osteotomy: is the type of staple fixation relevant? Int Orthop 44:1435–1439. https://doi.org/10.1007/s00264-020-04563-4
Malagelada F, Sahirad C, Dalmau-Pastor M, Vega J, Bhumbra R, Manzanares-Céspedes MC, Laffenêtre O (2019) Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop 43:625–637. https://doi.org/10.1007/s00264-018-4138-x
Kaufmann G, Dammerer D, Heyenbrock F, Braito M, Moertlbauer L, Liebensteiner M (2019) Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop 43:343–350. https://doi.org/10.1007/s00264-018-4006-8
Tsikopoulos K, Papaioannou P, Kitridis D, Mavridis D, Georgiannos D (2018) Proximal versus distal metatarsal osteotomies for moderate to severe hallux valgus deformity: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop 42:1853–1863. https://doi.org/10.1007/s00264-018-3782-5
Ellington JK, Jones CP, Cohen BE, Davis WH, Nickisch F, Anderson RB (2010) Review of 107 hallux MTP joint arthrodesis using dome-shaped reamers and a stainless-steel dorsal plate. Foot Ankle Int 31:385–390. https://doi.org/10.3113/fai.2010.0385
Acknowledgements
The present article was extracted from the thesis with control field no. 20181225190316.0 and grant no. 97-01-01-18677 which was written by Amir Human Hoveidaei for the degree of Doctor of Medicine. The authors would also like to thank Dr. Zahra Bagheri, Dr. Najaf Zare, and the Research Consultation Center (RCC) of Shiraz University of Medical Science in their assistance in statistical analysis of this manuscript.
Funding
The project was financed by Vice Chancellor for Research of the Shiraz University of Medical Science (Grant No. 97-01-01-18677).
Author information
Authors and Affiliations
Contributions
All the authors as participated in the design of the study, has contributed to the collection of the data, has participated in the writing of the manuscript, and assumes full responsibility for the content of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work has been submitted solely to International Orthopedics journal and is not published, in press, or submitted elsewhere.
Level of evidence: Level III, retrospective comparative series
Rights and permissions
About this article
Cite this article
Hoveidaei, A.H., Roshanshad, A. & Vosoughi, A.R. Clinical and radiological outcomes after arthrodesis of the first metatarsophalangeal joint. International Orthopaedics (SICOT) 45, 711–719 (2021). https://doi.org/10.1007/s00264-020-04807-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04807-3