Abstract
Introduction
Working hypothesis: The distal humeral bone density influences supracondylar fracture threshold. The aim of this study was first to develop a reproducible model of intra-articular distal humeral fractures and second to establish a relationship between bone mineral density (BMD) and the fracture threshold of the humerus.
Materials and methods
An original model of the fracture was developed using ten sawbones. After obtaining a reproducible and clinically relevant fracture model, we tested 21 cadaveric distal humeri for which the BMD was known with a stainless-steel custom-made proximal ulna jig. Fractures were created using a servo hydraulic-testing machine in axial compression to simulate a fall onto an outstretched hand. Fracture lines, load to failure, and rigidity of the bone were recorded based on the stress-strain curves.
Results
The fracture generation was reliable, reproducible, and clinically relevant (type B2). A significant correlation between the BMD and the fracture threshold was found. Mean threshold was 901.86 N/m2. Mean distal humerus BMD was 0.9097 g/cm2 (r = 0.7321).
Conclusions
We developed a reproducible articular fracture of the distal humerus model and found a correlation between the fracture threshold and bone mineral density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal humerus fractures in elderly patients are often complex and difficult to treat because of the high frequency of comminution and underlying osteoporosis. Osteoporosis is the most common bone disease in the western world and is recognized as a major cause of morbidity [1]. Fractures of the distal end of the humerus are almost always treated surgically to obtain the best outcome [2,3,4]. Osteoporosis is also a factor of open reduction and internal fixation (ORIF) failure with secondary displacement and arthroplasty loosening. The surgeon needs clinical, reliable, and objective tools to decide between ORIF and arthroplasty because the post-operative follow-up, and some specific complications are significantly different. Thanks to these elements, the surgeon is able to adapt the medical management specifically to the patient. Bone mineral density (BMD) of the distal end of the humerus can be estimated on standard radiographs [5, 6]. The relationship between BMD and fracture threshold is not established for the distal end of the humerus. However, this is essential to decide between ORIF and elbow arthroplasty. The hypothesis is that there is a relationship between BMD and fracture threshold, and the primary objective of this study is to establish this relationship. The secondary objective was to create an original and reproducible model of articular fracture of the distal extremity of the humerus which can be used in other studies and facilitate understanding of these difficult fractures.
Material and methods
Creation of a fracture model
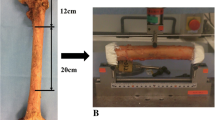
To simulate a fall onto the upper limb and create an original fracture model, the humeri were tested with 10° valgus and 20° flexion using a servo hydraulic-testing machine (INSTRON 8500 plus, INSTRON Corporation, High Wycombe, Buckinghamshire, UK). Ten fourth-generation distal humeri sawbones (Sawbones®, Division of Pacific Research Laboratories Inc.): five simulating an osteoporotic bone and five a healthy/non-osteoporotic adult bone. For non-osteoporotic sawbones, cortical thickness was 3 mm with a Young modulus of 16.7 GPa. The cancellous bone was dense with a Young modulus of 0.155 GPa. For osteoporotic sawbones, cortical thickness was 2 mm corresponding to a Young modulus of 16.7 GPa. The cancellous bone was alveolar with a Young modulus of 0.137 GPa. Each humeral distal end was held in place just above the olecranon fossa by a metal sleeve and 6 screws. The sleeve was connected to the machine using a hydraulic cylinder. The various assemblies were photographed in lateral, front, and rear views. The correct position on the machine was similar each time. The olecranon clamp was simulated using a stainless-steel custom-made proximal ulna jig surrounding the trochlea. In a sagittal view, the angle between the distal humeral shaft and the stainless-steel custom-made proximal ulna jig was 20° (Fig. 1). Before each test, the humerus and the jig were put in contact without fastening the humerus, allowing a natural valgus induced by the trochlea [7]. A contact pressure between the humerus and the jig was set at 10 N using the pressure sensor [8].
Use of humeri specimens
After obtaining a reproducible model of fracture, we used specimens from a previous study carried out under the same conditions [5]. Twenty-one unpaired fresh-frozen human cadaveric distal humeri were harvested and preserved at − 20 °C in order to keep the structural integrity and biomechanical properties of the bone intact. The entire soft tissue of the elbow was removed to keep only the epiphysis and 15 cm of the distal humerus. The tests were performed after an overnight thawing at room temperature. There were ten males and 11 females and nine right and 12 left distal humeri. The procedures of body donation were scrupulously respected for the specimens of this study.
Biomechanical testing
The humeri were placed on the machine in the same configuration as the sawbones. The mechanical test was performed in an axial compression. With a 10-N preload, the stainless-steel custom-made proximal ulna jig was translated superiorly at 50 mm per second using the machine actuator. The strain applied over time on the distal humerus (recorded by the INSTRON load cell) was recorded on an Excel sheet (Windows 8; Microsoft Corporation, Redmond, WA); load–displacement curves were created for each construct. The data acquisition frequency was 2500 points per second. Stress/strain curves for each bone were created to determine the load to failure and the relative stiffness of the distal humerus.
Statistical analysis
Statistical analysis was made using xlstat 2016 (Addinsoft, Paris, France). The Spearman goodness-of-fit test was used to confirm the assumption of normality for the continuous variables. The Pearson product-moment correlation coefficient (r) was calculated to evaluate the linear association between the bone mineral density (BMD) and the ultimate stress. A cutoff p value of 0.05 was chosen for all statistical significance.
Results
Sawbones
For the five sawbones simulating an osteoporotic bone, the fracture threshold was 315 N/m2 with a maximum at 382 N/m2 and minimum at 251 N/m2. The mean was 315 N/m2.
For the five sawbones simulating a non-osteoporotic bone, the fracture threshold was 1381.6 N/m2 with a maximum at 1551 N/m2 and minimum at 1075 N/m2. The mean was 1381.6 N/m2. With these sawbones, we created a reliable and reproducible experimental model of distal end humeral AO type B fracture [9]. The results obtained with the sawbones were similar with those obtained with human bones.
Human specimens
The distal humerus of human specimens had an average bone mineral density of 0.9097 g/cm2 with a maximum of 0.938 g/cm2 and a minimum of 0.2244 g/cm2. The fracture threshold average was 1017.8 N/m2 (maximum = 1361 N/m2; minimum = 697 N/m2), with a mean at 901.86 N/m2. The results are summarized in Table 1.
There is a correlation between bone mineral density and the fracture threshold (r = 0.7321) (Fig. 2).
Discussion
We demonstrated that there is a relationship between BMD and fracture threshold using a reproducible fracture model of distal humerus. However, fracture pattern of the distal humerus has not been thoroughly studied. To our knowledge, there is no study on the relationship between bone strength and BMD at the distal end of the humerus. It occurs more and more frequently in the trauma centres due to aging. Osteoporosis has been identified as one of the cause of these fractures and constitutes a challenge for its management. Most of the studies found in the literature evaluating the resistance of the different osteosynthesis methods created the fractures with a saw or an osteotome [10,11,12]. In the present study, we have simulated the fracture pattern of the distal humerus thanks to an original montage. This reproducible montage allowed us to establish a significant relationship between fracture threshold and BMD. Our results are similar to those of Augat [6]. Other montage could be created to obtain different types of fractures of the distal humerus in order to assess new osteosynthesis methods.
There are some limitations to our study. The physiological conditions for a fracture to occur are not completely reproduced. Our fracture model does not consider the presence of soft tissue (ligaments, muscles, tendon, joint capsule). During a fall, the axial compression is sudden and limited in time, which is not the case in our model since the compression is applied progressively by the machine. This difference in kinetics can potentially affect the results on both the fracture threshold and the type of fracture. Axial compression has been mainly taken into account while rotations and valgus-varus movements are associated with this type of trauma. Cancellous bone and cortical bone were not studied independently. Their share in the resistance of the distal humerus could not be established. The forearm framework is not complete, and the action of the radius is not analyzed. We have created an axial pressure. Torsion and shear phenomena are not studied in this experimental model. Finally, our custom-made proximal ulna jig had the mechanical property of steel and not bone. This friction torque difference could affect the results. We only obtained one type of fracture.
Conclusion
Surgical management of distal humerus fractures is performed most of the time. Bone quality is a determining factor for a most optimal outcome. These fractures are increasing in the elderly population. We have established a relationship between BMD and fracture threshold. Knowledge on the fracture threshold of the distal end of the humerus according to BMD can provide help in the difficult choice between arthroplasty and osteosynthesis.
We created a fracture model that can be used in other studies to test the strength of osteosynthesis closer to real clinical fractures. Moreover, this original method could be modified to obtain other types of fracture by replacing the proximal ulnar jig by another material or other shapes. Finally, this resistance threshold does not correspond completely to clinical reality due to the absence of soft tissue and bone segments of the forearm. Other biomechanical studies could clarify the different mechanisms and their consequences on the strength of the distal extremity of the humerus.
References
Lippuner K, Johansson H, Kanis J, Rizzoli R (2009) Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int 20(7):1131–1140. https://doi.org/10.1007/s00198-008-0779-8
Pidhorz L, Alligand-Perrin P, De Keating E, Fabre T, Mansat P, (SoFCOT). Sfdcoet (2013) Distal humerus fracture in the elderly: does conservative treatment still have a role? Orthop Traumatol Surg Res 99(8):903–907. https://doi.org/10.1016/j.otsr.2013.10.001
Clavert P, Ducrot G, Sirveaux F, Fabre T, Mansat P, SOFCOT (2013) Outcomes of distal humerus fractures in patients above 65 years of age treated by plate fixation. Orthop Taumatol Surg Res 99(7):771–777. https://doi.org/10.1016/j.otsr.2013.08.001
Mansat P, Nouaille Degorce H, Bonnevialle N, Demezon H, Fabre T, SOFCOT (2013) Total elbow arthroplasty for acute distal humeral fractures in patients over 65 years old - results of a multicenter study in 87 patients. Orthop Taumatol Surg Res 99(7):779–784. https://doi.org/10.1016/j.otsr.2013.08.003
Clavert P, Javier R, Charrissoux J, Obert L, Pidhorz L, Sirveaux F, Mansat P, Fabre T (2016) How to determine the bone mineral density of the distal humerus with radiographic tools? Surg Radiol Anat 38(4):389–393. https://doi.org/10.1007/s00276-015-1569-6
Augat P, Schorlemmer S (2006) The role of cortical bone and its microstructure in bone strength. Age Ageing 35(Suppl 2):ii27–ii31. https://doi.org/10.1093/ageing/afl081
Goldfarb C, Patterson J, Sutter M, Krauss M, Steffen J, Galatz L (2012) Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elb Surg 21(9):1236–1246. https://doi.org/10.1016/j.jse.2011.10.026
O'Driscoll S, Morrey B, An K (1990) Intraarticular pressure and capacity of the elbow. Arthroscopy 6(2):100–103. https://doi.org/10.1016/0749-8063(90)90007-z
Rüedi T, Buckley R, Moran C (2007) AO principles of fracture management. Thieme, Stuttgart
Shimamura Y, Nishida K, Imatani J, Noda T, Hashizume H, Ohtsuka A, Ozaki T (2010) Biomechanical evaluation of the fixation methods for transcondylar fracture of the humerus:ONI plate versus conventional plates and screws. Acta Med Okayama 64(2):115–120. https://doi.org/10.18926/AMO/32855
Windolf M, Maza E, Gueorguiev B, Braunstein V, Schwieger K (2010) Treatment of distal humeral fractures using conventional implants. Biomechanical evaluation of a new implant configuration. BMC Musculoskelet Disord 4(11):172. https://doi.org/10.1186/1471-2474-11-172
Kollias C, Darcy S, Reed J, Rosvold J, Shrive N, Hildebrand K (2010) Distal humerus internal fixation: a biomechanical comparison of 90° and parallel constructs. Am J Orthop (Belle Mead NJ) 39(9):440–444
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marcoin, A., Eichler, D., Kempf, JF. et al. Biomechanical model of distal articular humeral fractures—influence of bone density on the fracture threshold. International Orthopaedics (SICOT) 44, 1385–1389 (2020). https://doi.org/10.1007/s00264-020-04624-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04624-8