Abstract
Background
Few studies have described the characteristics and prognostic factors of elderly patients with osteosarcoma. We retrospectively investigated clinico-pathological features and prognostic factors in osteosarcoma patients > 40 years old.
Methods
Patients with high-grade osteosarcoma > 40 years old who were treated at our institutions from 2000 to 2016 were recruited for this study. Information on patient, tumour, and treatment-related factors was collected and statistically analyzed. The median follow-up was 26.5 months (range, 5–139 months) for all patients.
Results
Fifty patients (30 males and 20 females) were included. The median age at diagnosis was 59.5 years (range, 41–81 years). The primary lesions were found in the limbs in 32 patients, trunk in 12, and craniofacial bones in six. Primary and secondary osteosarcoma occurred in 41 and 9 patients, respectively. Eight patients exhibited initial distant metastasis. Definitive surgery and chemotherapy were performed in 39 patients each. The rate of good responders after neoadjuvant chemotherapy was 38%. The five year overall survival (OS) rates for all patients and those without distant metastasis at diagnosis were 44.5% and 51.1%, respectively. Multivariate analysis showed that definitive surgery was the only significant prognostic factor in non-metastatic patients. The five year OS and disease-free survival (DFS) rates for non-metastatic patients who received definitive surgery were 64.3% and 60%, respectively. Among these patients, neoadjuvant and/or adjuvant chemotherapy significantly improved both OS and DFS.
Conclusions
Complete surgical resection and intensive chemotherapy should be performed for osteosarcoma patients > 40 years old despite distinct clinicopathological characteristics from those of younger patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma is the most commonly diagnosed primary malignant bone tumour and predominantly occurs in adolescents and young adults, but there is a second incidence peak in the seventh and eighth decades of life [1]. Before the 1970s, the prognosis for patients with high-grade osteosarcoma was poor with long-term survival rates of < 20% [2]. The prognosis of osteosarcoma in younger patients has recently improved markedly because of advances in neoadjuvant and adjuvant chemotherapy and improved surgical techniques [2,3,4]. If the disease is localized, patients with high-grade osteosarcoma have long-term survival rates > 70% [2,3,4]. However, these data are not applicable to adult patients > 40 years old. It has been reported that the prognosis in older patients with osteosarcoma is still poorer than that in children and adolescents [5,6,7,8,9,10,11,12,13].
Although the clinical and histopathological features of osteosarcoma in adolescent patients have been well described, there are only a few reports of the clinico-pathological features and prognostic factors of osteosarcoma in elderly patients, and little is known about the treatment selection and its outcome in these patients [5,6,7,8,9,10,11,12,13,14,15]. Elderly patients with osteosarcoma demonstrate clinico-pathological characteristics including greater likelihood of axial location, onset often secondary to Paget’s disease or radiation therapy (RT), less tolerance to aggressive chemotherapy, and generally poorer outcome [5,6,7,8,9,10,11,12,13,14,15]. Surgery combined with adjuvant or neoadjuvant chemotherapy is considered standard management of younger patients with osteosarcoma [16, 17]. However, the efficacy of chemotherapy in elderly patients with osteosarcoma is still controversial. Some authors have reported no difference between surgery alone and surgery combined with chemotherapy, whereas others suggested that chemotherapy combined with surgery is more beneficial in patients older than 40 years [5,6,7,8,9,10,11,12,13,14,15]. Recently, there has been an increasing incidence of older patients with osteosarcoma as a result of the rapid increase in the number of the elderly in the population and the decrease of birth rates [18]. Therefore, the need for a study in this specific patient group has been increasing.
The aim of this retrospective study was to investigate the different clinicopathological features, clinical outcomes, and prognostic factors in patients > 40 years old with high-grade osteosarcoma in our affiliated hospitals.
Patients and methods
This study was designed as a multi-institutional retrospective study and was conducted by three tertiary musculoskeletal oncology hospitals: Osaka International Cancer Institute, Osaka University Hospital, and Osaka National Hospital. We retrospectively reviewed the records of each institute between January 2000 and December 2016. Patient eligibility criteria were diagnosis of high-grade osteosarcoma of bone with pathological confirmation by a musculoskeletal tumour pathologist at each institute and age at diagnosis > 40 years. The rationale for the cutoff of older than 40 in this study was that most previous clinical trials for osteosarcoma set the inclusion criteria up to 40 years [19,20,21]. This study was approved by the Institutional Review Boards of each participating institution.
Fifty patients over 40 years old with high-grade osteosarcoma were included in this study. Information on patient-related factors (age and sex), tumour-related factors (site of primary lesions, type [primary vs. secondary], size, and the presence or absence of metastasis at diagnosis), treatment-related factors (type of local therapy and chemotherapy status), local and distant relapse, follow-up period, and oncological outcome at final follow-up were anonymously collected from the patients’ medical charts. Osteosarcoma is classified as primary and secondary. Primary osteosarcoma arises de novo from the bone in the absence of a precursor lesion or treatment. Secondary osteosarcoma occurs in pre-existing benign bone lesions, such as Paget’s disease and irradiated bone, and results from the malignant transformation of those lesions. Additional information, such as the surgical margin (Enneking classification system) in patients who underwent surgery, the setting and course number of chemotherapies, and histological evaluation (Huvos necrosis grading system) in those who received chemotherapy, were also obtained [22, 23].
Of 50 patients over 40 years of age with high-grade osteosarcoma, the 30 males (60%) and 20 females (40%) had a median age of 59.5 years (range, 41–81 years). The sites of primary lesions were appendicular bones, such as the femur, tibia, and humerus, in 32 patients (64%); axial bones, including the spine and pelvis, in 12 (24%); and craniofacial bones in 6 (12%). Histologically, 41 (82%) and 9 (18%) patients had primary and secondary osteosarcomas, respectively. Of nine secondary osteosarcoma patients, three patients had a history of RT, and the remaining six patients were previously diagnosed with benign bone lesions, including giant cell tumours of bone (three patients), fibrous dysplasia (two patients), and Paget’s disease (one patient). The tumour size was > 8 cm in the greatest dimension in 25 cases (50%) and was ≤ 8 cm in the greatest dimensions in 25 (50%). According to the American Joint Committee on Cancer staging system, 22 patients (44%) were classified as IIA, 20 (40%) were IIB, 4 (8%) were IVA, and 4 (8%) were IVB, which indicated that 42 patients (84%) had localized disease and 8 (16%) had distant metastatic disease at diagnosis. Metastases involved only the lungs in four patients, only the bones in three, and both in one.
Forty-one patients (82%) received surgery for a primary tumour. Of those patients, 35 patients had limb salvage, five had an amputation, and one had curettage because of the axial location. An adequate margin, including a radical and wide margin, was achieved in 39 patients, and an inadequate margin, including a marginal and intralesional margin, was noted in two patients. From the viewpoint of surgical planning, we defined definitive surgery as surgery that was intended to achieve an adequate margin. Therefore, 39 patients (78%) underwent definitive surgery. The remaining nine patients (18%) did not receive surgery because of insufficient systemic conditions or inoperative local conditions for surgical treatment. Six patients with localized disease judged medically inoperable received carbon-ion radiotherapy (CIRT) and two metastatic patients received palliative RT to the primary site. One patient did not undergo any local treatment.
Chemotherapy was given to 39 patients (78%) and was not administered to 11 (22%) as a result of their poor systemic condition or their refusal. In patients who received surgery, a documented grading of tumour necrosis after pre-operative chemotherapy was available in 24 patients. Tumour necrosis rates in the surgical specimens were ≥ 90% in nine patients and < 90% in 15, which suggested that the 24 patients comprised nine good responders, including grade 3 or 4, and 15 poor responders, including grade 1 or 2. Among 34 patients who had no distant metastasis at initial diagnosis and received definitive surgery, 26 patients received neoadjuvant and/or adjuvant chemotherapy. Neoadjuvant and adjuvant chemotherapy was performed in 23 and 21 patients, respectively. The median course number of neoadjuvant and adjuvant chemotherapy was three (1–6) each. Most patients were treated with varying combinations of chemotherapy consisting of doxorubicin (DXR), cisplatin (CDDP), ifosfamide (IFM), and methotrexate (MTX). Various chemotherapy regimens, including DXR/CDDP (55 courses in 21 patients), high-dose IFM (48 courses in 21 patients), high-dose MTX (21 courses in 8 patients), and DXR/IFM (17 courses in 3 patients), were administered.
Overall survival (OS) was calculated from the date of the diagnostic biopsy to the date of death from any cause or last follow-up visit. In surgical complete remission patients, disease-free survival (DFS) was calculated from the date of surgery to the date of distant metastasis or local recurrence or last follow-up. Patients with distant metastasis at initial referral and without definitive surgery were excluded from the analysis of DFS. OS and DFS were calculated by using the Kaplan–Meier product limit method and the impact of prognostic factors was assessed by using the log rank test in univariate analysis. Multivariate analysis was performed by using Cox’s proportional hazard method with variables chosen by using a forward conditional stepwise approach. Differences were considered significant when p values were < 0.05. Statistical analyses were performed by using EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Survival and outcome
The median follow-up period was 26.5 months (range, 5–139 months) for all 50 patients. Nineteen patients (38%) were continuously disease free, three (6%) had no evidence of disease, two (4%) were alive with disease, 24 (48%) were dead of disease, and two (4%) were dead of other causes at the final follow-up.
The five year OS for all patients was 44.5% and the median OS was 55 months (range, 5–139 months). The five year OS for 42 patients (84%) without distant metastasis at initial diagnosis was 51.1%, whereas the two year OS for 8 patients (16%) with metastasis at diagnosis was 12.5%. The median OS for the metastatic patients was 13 months (range, 5–30 months). Thirty-four patients (68%) had no distant metastasis at initial diagnosis and received definitive surgery. Of those patients, 13 patients relapsed during follow-up. The first recurrences were metastases in ten cases and local recurrences in three. Two of the three local recurrences subsequently developed metastases. The five year OS and DFS rates for the patients without metastasis at initial diagnosis who received definitive surgery were 64.3% and 60%, respectively.
Prognostic factor analyses
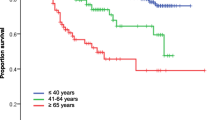
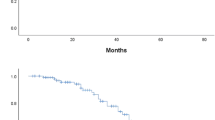
Among 42 patients with localized disease, age (p = 0.0261), definitive surgery (p < 0.0001), and chemotherapy (p = 0.0032) were correlated with prognostic factors for OS in univariate analysis (Table 1). Multivariate analysis showed that definitive surgery (p = 0.0025) was the only significant prognostic factor in these patients (Table 1 and Fig. 1). Among 34 patients without metastasis at initial diagnosis who received definitive surgery, age (p = 0.042), chemotherapy (p = 0.0096), and neoadjuvant and/or adjuvant chemotherapy (p = 0.0001) were significant prognostic factors for OS in the univariate analysis (Table 2). Multivariate analysis demonstrated that neoadjuvant and/or adjuvant chemotherapy (p = 0.02) was the only independent prognostic factor for OS (Table 2). On the other hand, neoadjuvant and/or adjuvant chemotherapy (p = 0.0298) was also the only favourable prognostic factor for DFS in the univariate analysis (Table 2). Therefore, neoadjuvant and/or adjuvant chemotherapy significantly improved both OS and DFS in this patient population (Figs. 2 and 3).
Discussion
Several studies have shown that elderly patients with osteosarcoma exhibited various clinical features distinct from those of adolescents [5,6,7,8,9,10,11,12,13,14,15]. This older group is characterized by more secondary lesions, more axial locations, more metastatic cases at diagnosis, and fewer patients receiving definitive surgery and chemotherapy, which might result in a worse prognosis [5,6,7,8,9,10,11,12,13]. Due to a predilection for axial localization, definitive surgery was technically difficult and incomplete surgical resection was more common. Chemotherapy was not often administered because of patients’ refusal, decreased bone marrow tolerance, and decreased renal or cardiac dysfunction.
Generally, osteosarcoma of the trunk is rare, representing 6.3% of all osteosarcomas [16]. However, in agreement with previously published data on osteosarcoma in patients over 40 years of age, there was a prominent tendency toward unusual location, especially in axial bones in the present study. It has been shown that patients with osteosarcoma occurring in axial bones are more likely to have initial distant metastasis [24]. Metastasis at diagnosis has also been frequently observed in elderly patients, with an incidence between 5% and 33% [8, 9, 11, 13, 14]. In the current study, 16% of the patients had distant metastasis to lungs and/or bones at initial diagnosis. However, 6 (19%) out of 32 patients with osteosarcoma arising in appendicular bones had distant metastasis at initial diagnosis, whereas 2 (17%) out of 12 patients in axial bones did, indicating that there was no relationship between initial distant metastasis and axial bone involvement. Consequently, there was no statistically significant difference in the outcomes between osteosarcoma patients over 40 years of age involving axial and appendicular bones.
It has been reported that the clinical outcome for patients with involvement of axial bones remains unsatisfactory because of difficulty to achieve local control [6, 7, 9, 11, 12]. A novel RT, such as CIRT, which can achieve excellent dose conformity while not exceeding the limits of tolerance of healthy surrounding tissue, can offer an option for patients with inoperable osteosarcoma in axial bones [25]. CIRT would be a mainstay for unresectable osteosarcoma of the trunk and could be an alternative to surgery. In the current study, eight out of 11 completely unresectable cases involved the axial skeleton, and six patients received CIRT. However, the five year OS for those patients was 0%. In accordance with previous reports, difficulty to perform definitive surgery was the main reason underlying the poorer survival in patients without distant metastasis at initial diagnosis. Aggressive local treatment can be successful in improving the outcome in patients > 40 years old with non-metastatic osteosarcoma.
It has been reported that distant metastasis at diagnosis and definitive surgery are significant prognostic factors for survival according to the results of previous studies concerning osteosarcoma in the elderly [5, 8, 10,11,12]. However, the role of chemotherapy in elderly patients with osteosarcoma has remained controversial [5,6,7,8,9,10,11,12,13,14,15]. These differences probably have arisen from different pharmacokinetics of low sensitivity to chemotherapy, modification of chemotherapy because of intolerance or less chemotherapy because of patient refusal, poor general condition, and impaired organ function, such as a renal failure or cardiac dysfunction [26]. Although some reports have stated that chemotherapy in elderly patients with osteosarcoma is beneficial [6, 8, 14, 15], other studies have shown that chemotherapy does not influence survival [5, 7, 9,10,11,12,13]. In the current study, neoadjuvant and/or adjuvant chemotherapy significantly improved both OS and DFS in patients with non-metastatic osteosarcoma who underwent definitive surgery, suggesting that those patients are regarded as good candidates for neoadjuvant and/or adjuvant chemotherapy whenever possible.
Previously, Kudawara et al. reported the favourable outcome of use of our four-drug regimen (OOS-D) consisting of DOX/CDDP, high-dose IFM, and high-dose MTX for young Japanese patients < 40 years old with non-metastatic osteosarcoma of the extremities [27]. However, the side effects associated with chemotherapy are generally more prominent in older patients and the planned dose intensity often cannot be completed. Although DXR/CDDP, high-dose IFM, and high-dose MTX were mainly administered according to the OOS-D protocol in the current study, each patient received different drugs, dosage, and dose intensity considering the patients’ general condition. Especially, the use of high-dose MTX was usually avoided because of the increased toxicity in patients aged > 60 years.
As shown in Table 3, previous studies have demonstrated ≥ 90% tumor necrosis in 0–48% of cases following neoadjuvant chemotherapy in osteosarcoma aged > 40 years [6,7,8,9, 11,12,13,14,15]. In accordance with previous reports, 38% of the patients who received neoadjuvant chemotherapy were good responders in the present study. These differences probably resulted from the diversity of the chemotherapy regimens, dose, and cycles. If the dose intensity could be increased with careful attention to patients’ general condition, patients’ prognoses might be improved. Further studies are required to investigate the most beneficial chemotherapy regimen and other alternatives, such as molecular-targeting chemotherapy, in elderly patients with osteosarcoma.
In conclusion, the present study revealed distinct clinicopathological features of osteosarcoma patients over 40 years of age such as the high incidence of axial tumours and the high frequency of secondary lesions due to pre-existing conditions. The non-metastatic patients should be treated aggressively with complete surgical excision and effective neoadjuvant and/or adjuvant chemotherapy whenever possible. Definitive surgery is still a mainstay of treatment, but it is also important to tailor chemotherapy protocols for patients over 40 years of age. Because of the rarity of aged osteosarcoma patients, a prospective multi-institutional study would be necessary to better assess the efficacy of chemotherapy.
References
Mirabello L, Troisi RJ, Savage SA (2009) Osteosarcoma incidence and survival rates from 1973 to 2004: data from the Surveillance, Epidemiology, and End Results Program. Cancer 115:1531–1543
Bacci G, Picci P, Ferrari S et al (1993) Primary chemotherapy and delayed surgery for nonmetastatic osteosarcoma of the extremities. Results in 164 patients preoperatively treated with high doses of methotrexate followed by cisplatin and doxorubicin. Cancer 72:3227–3238
Bacci G, Longhi A, Fagioli F et al (2005) Adjuvant and neoadjuvant chemotherapy for osteosarcoma of the extremities: 27 year experience at Rizzoli Institute, Italy. Eur J Cancer 41:2836–2845
Ferrari S, Smeland S, Mercuri M et al (2005) Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups. J Clin Oncol 23:8845–8852
Carsi B, Rock MG (2002) Primary osteosarcoma in adults older than 40 years. Clin Orthop Relat Res 397:53–61
Grimer RJ, Cannon SR, Taminiau AM et al (2003) Osteosarcoma over the age of forty. Eur J Cancer 39:157–163
Okada K, Hasegawa T, Nishida J et al (2004) Osteosarcomas after the age of 50: a clinicopathologic study of 64 cases—an experience in northern Japan. Ann Surg Oncol 11:998–1004
Manoso MW, Healey JH, Boland PJ et al (2005) De novo osteogenic sarcoma in patients older than forty: benefit of multimodality therapy. Clin Orthop Relat Res 438:110–115
Jeon DG, Lee SY, Cho WH et al (2006) Primary osteosarcoma in patients older than 40 years of age. J Korean MedSci 21:715–718
Longhi A, Errani C, Gonzales-Arabio D et al (2008) Osteosarcoma in patients older than 65 years. J Clin Oncol 26:5368–5373
Nishida Y, Isu K, Ueda T et al (2009) Osteosarcoma in the elderly over 60 years: a multicenter study by the Japanese Musculoskeletal Oncology Group. J Surg Oncol 100:48–54
Iwata S, Ishii T, Kawai A et al (2014) Prognostic factors in elderly osteosarcoma patients: a multi-institutional retrospective study of 86 cases. Ann Surg Oncol 21:263–268
Joo MW, Shin SH, Kang YK et al (2015) Osteosarcoma in Asian populations over the age of 40 years: a multicenter study. Ann Surg Oncol 22:3557–3564
Bacci G, Ferrari S, Donati D et al (1998) Neoadjuvant chemotherapy for osteosarcoma of the extremity in patients in the fourth and fifth decade of life. Oncol Rep 5:1259–1263
Bacci G, Ferrari S, Mercuri M et al (2007) Neoadjuvant chemotherapy for osteosarcoma of the extremities in patients aged 41-60 years: outcome in 34 cases treated with adriamycin, cisplatinum and ifosfamide between 1984 and 1999. Acta Orthop 78:377–384
Bielack SS, Kempf-Bielack B, Delling G et al (2002) Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol 20:776–790
Meyers PA, Schwartz CL, Krailo M et al (2005) Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol 23:2004–2011
Stark A, Kreicbergs A, Nilsonne ULF et al (1990) The age of osteosarcoma is increasing. JBJS (Br) 72-B:89–93
Ferrari S, Ruggieri P, Cefalo G et al (2012) Neoadjuvant chemotherapy with methotrexate, cisplatin, and doxorubicin with or without ifosfamide in nonmetastatic osteosarcoma of the extremity: an Italian sarcoma group trial ISG/OS-1. J Clin Oncol 30:2112–2118
Bielack SS, Smeland S, Whelan JS, EURAMOS-1 investigators et al (2015) Methotrexate, doxorubicin, and cisplatin (MAP) plus maintenance pegylated interferon alfa-2b versus MAP alone in patients with resectable high-grade osteosarcoma and good histologic response to preoperative MAP: first results of the EURAMOS-1 good response randomized controlled trial. J Clin Oncol 33:2279–2287
Marina NM, Smeland S, Bielack SS et al (2016) Comparison of MAPIE versus MAP in patients with a poor response to preoperative chemotherapy for newly diagnosed high-grade osteosarcoma (EURAMOS-1): an open-label, international, randomised controlled trial. Lancet Oncol 17:1396–1408
Enneking WF, Spanier SS, Goodman MA (1980) A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res 153:106–120
Huvos AG, Rosen G, Marcove RC (1977) Primary osteogenic sarcoma: pathologic aspects in 20 patients after treatment with chemotherapy en bloc resection, and prosthetic bone replacement. Arch PatholLab Med 101:14–18
Bielack SS, Wulff B, Delling G et al (1995) Osteosarcoma of the trunk treated by multimodal therapy: experience of the Cooperative Osteosarcoma Study Group (COSS). Med Pediatr Oncol 24:6–12
Matsunobu A, Imai R, Kamada T et al (2012) Impact of carbon ion radiotherapy for unresectable osteosarcoma of the trunk. Cancer 118:4555–4563
Brouwer CAJ, Gietema JA, van den Berg MP et al (2006) Long-term cardiac follow-up in survivors of a malignant bone tumor. Ann Oncol 17:1586–1591
Kudawara I, Aoki Y, Ueda T et al (2013) Neoadjuvant and adjuvant chemotherapy with high-dose ifosfamide, doxorubicin, cisplatin and high-dose methotrexate in non-metastatic osteosarcoma of the extremities: a phase II trial in Japan. J Chemother 25:41–48
Acknowledgments
This work was supported by JSPS KAKENHI Grant Number JP16H05448 and Grant of Japan Orthopaedics and Traumatology Research Foundation, Inc.372. We thank Enago for providing high-quality editing service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Imura, Y., Takenaka, S., Kakunaga, S. et al. Survival analysis of elderly patients with osteosarcoma. International Orthopaedics (SICOT) 43, 1741–1747 (2019). https://doi.org/10.1007/s00264-019-04332-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04332-y