Abstract
Purpose
This nationwide study assessed associations between comorbidity and mortality after hip fracture in young and middle-aged patients.
Methods
Data on 19,682 patients aged 18 to 65 years were extracted from Danish registries out of 154,047 patients who experienced a hip fracture between 1996 and 2012. Mortality and comorbidity were assessed using information on vital status, hospital admissions, and prescriptions.
Results
Of the 19,682 patients 17,722 (90.0%) were middle-aged (40–65 years) and 1960 (10.0%) were young (18–39 years). The 30-day mortality rates were 3.2% (n = 570) and 1.6% (n = 32), respectively. Indicators of multi-trauma (hazard ratio (HR), 3.5 95% confidence interval (CI) [1.6–7.8], n = 2056) and having diabetes (HR, 4.4 [1.2–11.3], n = 59) and heart disease (HR, 4.4[1.3–14.8], n = 57) increased 30-day mortality in the young patients, while having cancer (HR, 5.0 [4.2–5.9], n = 1958) increased 30-day mortality in the middle-aged patients.
Conclusion
Heart disease and diabetes were associated with high mortality in the young patients while having cancer was associated with high mortality in the middle-aged patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures present a challenge to the worldwide health care system and patients who suffer from a hip fracture often have excess morbidity and mortality [1, 3]. Factors such as age, sex, anaemia, high Charlson Comorbidity Index, high American Society of Anesthesiologists (ASA) score, and dementia have all been related to mortality [14, 20]. Hip fractures among elderly patients are generally sustained in falls, whereas hip fractures in a younger population more often are caused by high-energy trauma [10, 17, 26]. The mortality after hip fracture has been heavily investigated among the elderly population. However, studies on hip fracture-related mortality among younger adults aged < 65 years are relatively scarce [27]. Young patients present a challenge in hip fracture treatment with a high incidence rate of post-surgical complications and a re-operation rate approaching 20% [30].
Until now, only a few nationwide population-based studies of mortality after hip fracture in younger patients have been published [15, 16, 32]. We hypothesize that both young and middle-aged patients below 65 years have a higher mortality rate after hip fracture compared to the general population, and that comorbidity affects mortality in both age groups. Hence, this study assesses the mortality after hip fracture and the association with comorbidity in young and middle-aged patients using a large sample of patients from the Danish National Patient Register.
Materials and methods
Study population
In the Danish National Patient Registry, we identified all patients aged between 18 and 65 years who were admitted with a fractured hip with the following ICD-10 codes: DS720 (femoral neck), DS721 (pertrochanteric), and DS722 (subtrochanteric) in Denmark during the period January 1, 1996 to December 31, 2012. Patients who appeared more than once during the period due to a contralateral fracture or to subsequent hip fractures were included with the index fracture only. Deaths registered in the Danish Registries from time of hip fracture in the period Jan 1, 1996 to the end of follow-up as of Dec 31, 2012 were included as the primary outcome variable.
We included a total of 19,682 patients between 18 and 65 years of age subsequently separated into a young group aged between 18 and 39 years and a middle-aged group between 40 and 65 years old. We included sex, age, and comorbidity in the form of groupings from the Charlson Comorbidity Index (CCI), which was coded based on the method described by Quan et al. [24]. Comorbidity was assessed by ICD-10 codes registered in the National Patient Registry before the time of hip fracture. The following comorbidity groups were included in the study: heart disease, cerebrovascular disease, peptic ulcer disease, chronic pulmonary disease, rheumatic disease, renal disease, liver disease, cancer, diabetes mellitus, hemi/paraplegia, and HIV/AIDS (Supplementary Table 1). Furthermore, to adjust for alcoholism or concurrent traumas, indicators of these conditions were included in the analyses (Supplementary Tables 2 and 3).
National patient registries
The Danish Civil Registration System is a database where all Danish citizens are registered by a unique ten -digit civil registration number. The unique civil registration number makes it possible to retrieve information on individuals from a selection of national registries [29]. The Danish National Patient Register covers all somatic hospital admissions [18]. The Danish National Prescription Database includes information on all prescription drugs sold in Denmark since 1994 [13]. Data for calculating annual mortality rates in both men and women from the general Danish population in the years 1996–2012 were obtained from Statistics Denmark’s website: https://dst.dk/da/Statistik/statistikbanken.
Statistics
Continuous data were presented as means with standard deviations (SD), categorical data as numbers and percentages (%). For comparison of variables between age groups, student t tests, chi squared tests, or Fischer’s exact tests were applied when appropriate. Cox regression models were used for computing 30-day and one year hazard ratios for all-cause mortality with 95% confidence intervals for both univariate (unadjusted) and multivariate (adjusted) analyses. The multivariate regression models were based on variables significant at a 5% level by univariate analysis as well as sex and age. The proportional hazards assumption was assessed graphically plotting Schoenfeld residuals of all included variables. No major violations were detected. P values less than 0.05 were considered statistically significant.
Results
Among the 19,682 patients aged 18–65, 90% (n = 17,722) were middle-aged (40–65 years) and the remaining 10% (n = 1960) were young (18–39 years). Among the young patients, there was a higher proportion of males (77.24%) compared to females, in contrast to the even distribution of sex in the middle-aged patients (50% males). Also, the middle-aged patients had a higher prevalence of all comorbidities dominated by heart disease and indicators of excess use of alcohol (Table 1). In contrast, the young patients were more likely to be admitted with concurrent trauma and fractures besides the hip fracture and the most frequent comorbidities were hemi/paraplegia, diabetes mellitus, and heart disease (Table 1).
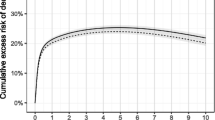
The young patients had a 30-day mortality rate of 1.6% (n = 32) and a one year mortality rate of 3.9% (n = 77). The middle-aged patients had a 30-day mortality rate of 3.2% (n = 570) and a one year mortality rate of 12.8% (n = 2259). For comparison the age-matched background population had 30 day mortality rates for individuals 18 to 39 years of 0.0063%, and 40 to 65 years of 0.05% and one year mortality rates of 0.075% and 0.59%, respectively.
Comorbidity was more frequent in the middle-aged patients (45.5%) compared to the young patients (14.4%) (Table 1). In the young patients, indicators of multi-trauma (adjusted HR, 3.5 [1.6–7.8]), diabetes mellitus (diabetes mellitus adjusted HR, 4.4 [1.2–11.3]), and heart disease (heart disease adjusted HR, 4.4 [1.3–14.8]) were associated with increased 30-day mortality (Fig. 1). In contrast, in the middle-aged patients, having cancer was associated with the largest increase in 30-day mortality (adjusted HR, 5.0 [4.2–5.9]). Furthermore, indicators of alcoholism (adjusted HR, 1.7 [1.4–2.1]) and liver disease (adjusted HR, 1.7 [1.3–2.2]) were also associated with a modest increase in 30-day mortality (Fig. 2). For both young (adjusted HR, 13.7 [7.5–25.1]) and middle-aged patients, cancer was associated with the largest increase in one year mortality (young adjusted HR, 13.7 [7.5–25.1], middle-aged adjusted HR, 7.3 [6.7–7.9]) (Tables 2 and 3). Other comorbidities such as renal disease in the young (adjusted HR, 4.4 [1.4–14.4]) and liver disease or renal disease in the middle-aged patients (liver adjusted HR, 1.9 [1.6–2.1]; renal adjusted HR, 1.8 [1.4–2.2]) associated with a modest increase in one year mortality.
Discussion
The most important finding in this nationwide study of almost 20,000 patients aged 18–65 years, is that comorbidity was associated with mortality after hip fracture in both young and middle-aged patients. In the young patients, heart disease and diabetes associated with the highest risk estimates for 30-day mortality, also when adjusting for indicators of multi-trauma, while having cancer was associated with the highest risk estimates in the middle-aged patients. Our findings support the notion that hip fractures among young patients present a real risk and additionally, that certain comorbidities need to be taken into consideration in the care of the young and middle-aged patients. An integrated multidisciplinary model as introduced for the elderly by orthopaedic units in Europe [5, 7] is warranted.
The mortality rates after hip fracture in the middle-aged and the young patients are almost ten times as high as in the same age groups in the background population. Thus, experiencing the trauma of a hip fracture increases mortality as for the elderly population [21]. Also, these patients could be selected by their comorbid conditions that increase the risk of hip fracture such as it has been proven in studies of the elderly population [4]. However, it is plausible that certain comorbid conditions have impact on mortality in one age group and not in another as shown in the present study. Lastly, age is a very strong predictor of mortality after hip fracture even in the elderly [7].
Compared to elderly patients aged 65 years and above who have an increasing burden of comorbidity over time [3], the middle-aged patients in our study population had a lower overall comorbidity burden. Furthermore, the most important comorbid condition affecting mortality in the middle-aged patients was having a cancer diagnosis while heart- and peptic ulcer-disease only had modest associations with increased mortality. In an elderly population, comorbid conditions inferring a higher ASA-score or more severe osteoporosis which both have effect on mortality [4] would be expected to have the strongest association with increased mortality. Therefore, distinguishing between the elderly and the middle-aged patients in relation to the peri-operative care of comorbid conditions is warranted.
Diabetes mellitus and heart disease were among the most frequent comorbidities in the young patients and associated with the highest risks of 30-day mortality after hip fracture in our study. However, the number of patients are quite low if calculated per year (59 and 57 over a period of 13 years) with an average of less than five young patients having these comorbidities per year in Denmark. Thus, our results should be interpreted in the light of the relatively low comorbidity burden in the young patients in our population-based study compared to other studies [2, 28, 31]. Of note, patients aged 20–40 years from a nationwide study in Asia also had low frequencies of comorbidity [15].
Patients with type 1 diabetes have increased risk of hip fractures compared with both patients with type 2 diabetes and matched control individuals [8], and diagnosis at an early age as well as the duration of diabetes have been identified as risk factors for fractures in general [6]. A recent population-based study showed that low body mass index and diabetes have an effect on the incidence of hip fractures, but also that these two factors interact [9]. In a population of 50 years and above, also patients with type 2 diabetes have increased post-fracture mortality compared to non-diabetic patients [19]. Generally, in patients with diabetes, coronary heart disease is more common [22]. However, for comparison to our study, there is limited information from studies assessing the frequency of coronary heart disease in a younger population of patients after hip fracture. Thus, it may not be surprising that having diabetes and heart disease could increase mortality after hip fracture in young patients.
In the middle-aged patients, the most frequent comorbidity was heart disease, which is also corroborated by an Estonian population-based cohort study that found congestive heart disease to be the most common comorbidity among patients above 50 years of age [11]. Furthermore, a Danish population-based study showed cerebrovascular disease, cancer, and congestive heart failure to be the most frequent [12]. However, in the middle-aged patients, having heart disease was not associated with increased mortality. In contrast, the less prevalent comorbidity cancer increased both the 30-day and one year hazard ratio for death. Patients with cancer who experience a hip fracture might be more frail patients who already have an increased risk of death before they experience a hip fracture. Of note, one year mortality was affected quite dramatically by having cancer in the young patients, where the same issue of frailty might apply.
Up to 50–60% of multi-trauma patients die from their injuries alone prior to arrival at a hospital [23], and this could lead to selection bias in our study. We adjusted for indicators of multi-trauma such as ICD-10 codes for other concurrent fractures and traumas in the multivariate regression analysis but we cannot eliminate all potential bias. Also, we adjusted for patients who suffer from alcoholism, as they are predisposed to cancer, liver cirrhosis, and alcohol-related injuries which all lead to increased mortality [25]. Another study reported about a quarter of both young and middle-aged patients to be self-reported high-volume drinkers [2]. We found less than 10% alcohol-related admissions and or use of alcohol medication among the young patients and 18–22% in the middle-aged patients. Thus, we could have underestimated the association between alcohol and mortality in the young patients.
Since the study was register-based, we had no loss to follow up but at the same time, limitations such as no direct information on surgery, peri-operative management, complications, anaesthesia, smoking habits, alcohol consumption, under-weight or obesity, or exercise. Confounding by these factors can therefore neither be evaluated nor ruled out. Of note, concerning the timing of surgery, small delays have not proven to affect mortality [33]. Overall mortality was obtained by registry linkage. The Danish Civil Registration system has a very high validity, and the risk of misclassification is considered minimal [29]. The main strength of the study is the large number of patients covering all registered Danish patients between 18 and 65 years with a hip fracture over a period of 13 years. Thus, the study is both representative of the Danish population and generalizable for similar populations.
In conclusion, both young and middle-aged patients experience increased mortality after hip fracture compared to the background population. Heart disease and diabetes were associated with high mortality in the young patients while having cancer was associated with high mortality in the middle-aged patients. Attention to patients with these comorbid conditions is warranted to prevent deaths in young and middle-aged patients after hip fracture.
Abbreviations
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- ICD-10:
-
International classification of diseases
References
Abrahamsen B et al (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20(10):1633–1650
Al-Ani AN et al (2013) Risk factors for osteoporosis are common in young and middle-aged patients with femoral neck fractures regardless of trauma mechanism. Acta Orthop 84(1):54–59
Brauer CA et al (2009) Incidence and mortality of hip fractures in the United States. Jama 302(14):1573–1579
Carow J et al (2017) Mortality and cardiorespiratory complications in trochanteric femoral fractures: a ten year retrospective analysis. Int Orthop 41(11):2371–2380
Civinini R et al (2019) Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the "Florence hip fracture unit". Int Orthop 43(1):187–192
Dhaliwal R et al (2018) Determinants of fracture in adults with type 1 diabetes in the USA: results from the T1D exchange clinic registry. J Diabetes Complicat 32(11):1006–1011
Forni C et al (2018) Predictive factors for thirty day mortality in geriatric patients with hip fractures: a prospective study. Int Orthop
Hamilton EJ et al (2017) Risk and associates of incident hip fracture in type 1 diabetes: the Fremantle diabetes study. Diabetes Res Clin Pract 134:153–160
Huang HL et al (2018) Associations of body mass index and diabetes with hip fracture risk: a nationwide cohort study. BMC Public Health 18(1):1325
Hwang LC et al (2001) Intertrochanteric fractures in adults younger than 40 years of age. Arch Orthop Trauma Surg 121(3):123–126
Jurisson M et al (2017) The impact of comorbidities on hip fracture mortality: a retrospective population-based cohort study. Arch Osteoporos 12(1):76
Kannegaard PN et al (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39(2):203–209
Kildemoes HW et al (2011) The Danish National Prescription Registry. Scand J Public Health 39(7 Suppl):38–41
Laulund AS et al (2012) Routine blood tests as predictors of mortality in hip fracture patients. Injury 43(7):1014–1020
Leu TH et al (2016) Incidence and excess mortality of hip fracture in young adults: a nationwide population-based cohort study. BMC Musculoskelet Disord 17:326
Lin JC et al (2014) Mortality and complications of hip fracture in young adults: a nationwide population-based cohort study. BMC Musculoskelet Disord 15:362
Lofthus CM et al (2006) Young patients with hip fracture: a population-based study of bone mass and risk factors for osteoporosis. Osteoporos Int 17(11):1666–1672
Lynge E et al (2011) The Danish National Patient Register. Scand J Public Health 39(7 Suppl):30–33
Martinez-Laguna D et al (2017) Excess of all-cause mortality after a fracture in type 2 diabetic patients: a population-based cohort study. Osteoporos Int 28(9):2573–2581
Norring-Agerskov D et al (2013) Metaanalysis of risk factors for mortality in patients with hip fracture. Dan Med J 60(8):A4675
Papadimitriou N et al (2017) Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health 2(5):e239–e246
Peters SA et al (2014) Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 57(8):1542–1551
Pfeifer R et al (2016) Mortality patterns in patients with multiple trauma: a systematic review of autopsy studies. PLoS One 11(2):e0148844
Quan H et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139
Rehm J, Shield KD (2013) Global alcohol-attributable deaths from cancer, liver cirrhosis, and injury in 2010. Alcohol Res 35(2):174–183
Robinson CM et al (1995) Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res (312):238–246
Rogmark C et al (2018) Hip fractures in the non-elderly-who, why and whither? Injury 49(8):1445–1450
Samuel AM et al (2016) Surgical treatment of femoral neck fractures after 24 hours in patients between the ages of 18 and 49 is associated with poor inpatient outcomes: an analysis of 1361 patients in the National Trauma Data Bank. J Orthop Trauma 30(2):89–94
Schmidt M et al (2014) The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol 29(8):541–549
Slobogean GP et al (2015) Complications following young femoral neck fractures. Injury 46(3):484–491
Verettas DA et al (2002) Fractures of the proximal part of the femur in patients under 50 years of age. Injury 33(1):41–45
Wang MT et al (2017) Hip fractures in young adults: a retrospective cross-sectional study of characteristics, injury mechanism, risk factors, complications and follow-up. Arch Osteoporos 12(1):46
Wong SHJ et al (2018) Hip fracture time-to-surgery and mortality revisited: mitigating comorbidity confounding by effect of holidays on surgical timing. Int Orthop 42(8):1789–1794
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical approval
According to Danish law, ethical committee approval is not required for this type of observational study. The data were obtained through secure remote access to Statistics Denmark (ref. 704670). The study was approved by the Danish Data Protection Agency (2012-58-0004)/local number BBH-2014-050.
Informed consent
For observational register-based studies, formal consent from patients is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 40 kb)
Rights and permissions
About this article
Cite this article
Omari, A., Madsen, C.M., Lauritzen, J.B. et al. Comorbidity and mortality after hip fracture in nineteen thousand six hundred and eighty two patients aged eighteen to sixty five years in Denmark from 1996 to 2012. International Orthopaedics (SICOT) 43, 2621–2627 (2019). https://doi.org/10.1007/s00264-019-04323-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04323-z





