Abstract
Purpose
The occurrence, evolution and treatment outcome of osteoarthritis are influenced by a series of factors, including obesity. Assessing how chronic inflammation present in obesity changes the values of peri-operative biological tests could facilitate a clearer interpretation of laboratory examinations for the proper management of possible complications.
Methods
This descriptive study compared biological and clinical factors during the peri-operative period in patients undergoing total hip/knee replacement, in order to identify the special characteristics of the inflammatory status in obese compared to normal weight patients. In the two groups (71 normoponderal, 74 obese), serum levels of fibrinogen, high-sensitivity C-reactive protein (hsCRP), tumour necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6) were determined 24 hours pre- and post-operatively.
Results
Our results found significant post-operative increases in serum levels of IL-6 and hsCRP in both groups (p = 0.0001), with inter-group differences in pre-operative hsCRP (p = 0.02) and post-operative IL-6 levels (p = 0.013). Interestingly, TNF-alpha levels were much higher in the obese pre-operatively than post-operatively (p = 0.002) and higher than the normoponderals (p = 0.003), decreasing to levels similar to those of the normal weight patients on day two.
Conclusions
Because of its important clinical implications, an appropriate comprehension of the peri-operative changes in a patient’s inflammatory status has the potential to influence therapeutic attitude. We failed to observe any significant post-operative differences in the mean values of the markers assessed, except those of IL-6, implying that serum levels of fibrinogen, hsCRP and TNF-alpha within 24 hours after large joint replacements are not influenced by the patient’s ponderal status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity are currently one of the main public health problems [1] and at the same time a major risk factor in the occurrence of chronic non-communicable diseases [2]. These include osteoarthritis, the frequency of which is four times higher in people with body mass index (BMI) values of 30–35 kg/m2 compared to normal weight individuals [3, 4].
It has been shown that an excess of adipose tissue plays the role of an endocrine organ, secreting adipokines, cell signalling proteins which function at the auto-, para- and endocrine levels, with major influences on metabolism and inflammatory status, and responsible for maintaining a low level of chronic inflammation in obese individuals [5]. This inflammatory status appears to have a major role in the progression of osteoarthritic disease and may negatively impact the results of interventions for large joint (hip, knee) replacement [6, 7]. The body’s inflammatory response is responsible for the onset of pain and the healing process, and is involved in postoperative morbidity and mortality [8]. Therefore, for obese individuals, chronic inflammation has the potential to create confusion in interpreting inflammatory tests necessary to identify possible post-operative complications [9].
Numerous studies have identified potential biomarkers with a diagnostic or prognostic role in the assessment of osteoarthritis [10]. Among them, interleukin 6 (IL-6) is considered a “burden of disease” biomarker, as it is a cytokine with both pro-and anti-inflammatory roles [11]. Although IL-6 values in the synovial fluid do not appear to be correlated with BMI, age or severity of osteoarthritis, some authors have observed the presence of elevated levels of cytokine in obesity [12,13,14]. It has also been observed that IL-6 serum values show circadian variations with a minimum at about six a.m. [15]. Other markers suitable for the identification of inflammation are fibrinogen, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are more commonly used in the clinical context to identify possible post-operative complications of an inflammatory/infectious nature [16]. Among thee, CRP levels seem to be influenced by the patient’s weight status [17, 18].
Based on the hypothesis that the inflammatory status of obese patients may imply significant peri-operative differences compared to normoponderal patients, we proposed to evaluate four inflammatory markers (fibrinogen, hsCRP, TNF-alpha and IL-6) during the 48-hours peri-operative period in two groups of patients undergoing total hip/knee replacement. The aim was to identify the particularities of the peri-operative inflammatory process in obese patients, in order to contribute to the optimization of post-operative therapeutic management and possibly provide a support for the interpretation of inflammatory tests in obese patients.
Patients and methods
Patients
The study was approved by the Ethics Committees of both the Clinic of Orthopaedics and Traumatology of the Clinical County Hospital Mureș and the University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureș. All participating patients gave their written informed consent prior to inclusion in the study, which was conducted in compliance with the guidelines of the Declaration of Helsinki.
The number of patients included (N) was determined using the power analysis formula:
where p stands for the prevalence, Zα is a constant, and d is the value for the precision. Considering a prevalence of 5%, the result is N = 0.05 × (1–0.05) × (1.96/0.05)2 = 73 patients.
Designed as a descriptive study, our investigation included 145 patients with advanced stages of hip or knee osteoarthritis (Kellgren Lawrence grades 3 or 4) who underwent total hip/knee replacement. Based on their body mass index (BMI) values, the patients were recruited for either the normoponderal group (BMI < 25 kg/m2, 71 patients total, 33 females and 38 males, mean age 66.05 ± 8.73 years) or the obese group (BMI > 30 kg/m2, 74 patients total, 52 females and 22 males, mean age 65.04 ± 9.17 years). For each patient, demographic and anthropometric data were collected (age, gender, weight, BMI, skinfold thickness, waist circumference, etc.), as well as data on the location, type and grading of osteoarthritis, disease history (onset, exacerbations, previous treatments, NSAID medication with duration and doses, etc.), any associated diseases and treatments followed, and previous laboratory data, in particular inflammatory markers (CRP, ESR, fibrinogen), where available.
Exclusion criteria were a personal medical history of systemic inflammatory diseases, autoimmune diseases, inflammatory arthritis or cancer, as well as any long-term corticotherapy. For all involved patients, surgical interventions were performed according to the clinic’s protocol, using a standard surgical technique, in spinal block. Post-operative wound drainage was provided by vacuum suction, and removed on the first day after surgery, the patients being mobilised on the second post-operative day. Patients were observed during their hospital stay for any post-operative complications.
Sample harvesting and laboratory methods
Two sets of blood samples were harvested from each patient, at the same time of the day (six am.)—a first set 24 hours before surgery (day 1–D1) and the second set in the first 24 hours post-operatively (day 2–D2). Blood was harvested in tubes treated with anticoagulant: sodium citrate for fibrinogen determination, and EDTA for the rest of the determinations (hsCRP, TNF-alpha, IL-6). After harvesting, tubes were centrifuged at 1500×g for 20 minutes to obtain platelet-poor plasma, and the samples were aliquoted and stored at − 80 °C until assessment. All blood samples were processed at the Centre for Advanced Medical and Pharmaceutical Research of the University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureș.
Determination of fibrinogen and hsCRP
For the quantitative determination of fibrinogen levels, the Clauss photo-optical method was used, with an STA Compact automated coagulometer and STA®-Liquid Fib reagent (Diagnostica Stago SAS, France). The reference range was 200–400 mg/dL, and the measuring range was 100–800 mg/dL (1:20 plasma dilution), with a minimum detection limit of 100 mg/dL, and intra- and inter-run coefficients of variability of < 4.9% and < 3.2%.
The quantitative determination of hsCRP was performed using a BN ProSpec® nephelometer, with CardioPhase® hsCRP reagent (Siemens Healthcare Diagnostics, GmbH, Marburg, Germany), and a reference range of < 3 mg/L. Measurement range was 0.175–11 mg/L, with a 0.175 mg/L minimum detection limit, and intra- and inter-run coefficients of variability of < 4.0%, and < 4.6%, respectively.
Determination of TNF-alpha
For measuring the plasma concentration of TNF-alpha, the sandwich enzyme-linked immunosorbent assay (ELISA) was used on the Dynex DSX analyser using the human TNF-alpha Quantikine reagent (R&D Systems, Inc. Minneapolis, USA) according to the manufacturer’s instructions. Monoclonal antibodies specific for TNF-alpha fixed on the solid reaction medium formed immune complexes with TNF-alpha from the sample; after addition of the secondary antibodies and development of the tetramethylbenzidine (TMB) reaction, the colour intensity developed at the end of the reaction was proportional to the concentration of the analyte of interest in the sample. The optical density of the samples, read at the end of the reaction, was interpolated on the calibration curve, thus obtaining the concentration of TNF-alpha. The measurement range was between 15.6 and 1000 pg/mL, the lower limit of detection (LLD) was 1.6 pg/mL and the intra- and inter-assay coefficients of variability (CV) were < 5.2% and < 5.4% respectively.
Determination of IL-6
Serum samples for IL-6 quantification were collected in EDTA-treated vacutainers and stored at − 80 °C after initial processing, until the assays were performed. The manufacturer asserts that any pre-analytical harvest errors do not affect the obtained results. For IL-6 determinations, the Immulite 2000 XPI Immunoassay System (Siemens Healthcare GmbH, Germany) was used and samples were processed according to the manufacturer’s recommendations. The analyser uses the sequential solid-phase chemiluminescence immunoassay consisting of 2 incubation cycles of 30 minutes. The analytical sensitivity of the method is 2 pg/mL, and the calibration curve provides results up to 1000 pg/mL. Coefficients of variability were 4.5% intra-run and 5.3% inter-run.
Statistical analysis
Statistical analysis was performed using SPSS for Windows version 20.0 (SPSS, Inc., Chicago, IL). To assess the normality of continuous variables (i.e. fibrinogen, hsCRP, TNF-alpha, IL6), the Shapiro-Wilk test was applied. Student’s t test paired and unpaired versions was used to assess the differences between means of continuous variables (expressed as mean ± SD), while differences between nonparametric variables (expressed as median, range) were compared using the Mann-Whitney and Wilcoxon test. We interpreted all tests against a p = 0.05 significance threshold and statistical significance was considered for p values below the significance threshold.
Results
The two groups were similar in terms of mean age and days of hospital stay, but with more female patients in the obese group (70.3% vs 46.5%). Table 1 shows the values for BMI and waist circumference (with significant inter-group differences), as well as those of common laboratory tests (glucose, cholesterol, uric acid, triglycerides)—all with similar results (ANOVA with Bonferroni multiple comparison test).
Table 2 shows the mean values for the inflammatory markers assessed in the two groups, on D1 and D2. In terms of fibrinogen values, there was no significant difference between values recorded for D1 and D2 in the obese or normoponderal group, and neither between the values for the two groups on either D1 or D2.
For hsCRP, within both groups of patients, there was a significant increase in serum values on D2 as compared to D1 (p = 0.0001, Wilcoxon test). We also found a significant difference, albeit smaller, between the values obtained on D1 for the two groups, with mean values for obese patients exceeding those of the normal weight group (p = 0.02, Mann-Whitney test); however, this difference was not observed when comparing inter-group values for D2 (p = 0.42, Mann-Whitney test).
As for TNF-alpha, on intra-group analysis, there was a statistically significant difference in serum values between D1 and D2 only in the obese group, with decreased mean values on D2 (p = 0.002, Wilcoxon test). For D1, the values of the obese group were also increased as compared to those of the normal weight group, with a significant difference (p = 0.003, Mann-Whitney test), but a similar difference was not observed for D2 (p = 0.65, Mann-Whitney test).
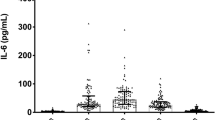
Both groups had significantly increased values of serum IL-6 on D2 compared to D1 (p = 0.0001, Wilcoxon test), but with significant inter-group differences only on D2 (p = 0.013, Mann Whitney test).
The post-operative evolution was uneventful for all patients, and they were discharged without any infectious complications.
Discussion
Obesity has long been considered a problematic medical condition, and the growing number of people affected worldwide, its multiple implications, and the risk factors it implies, have deemed it an important global public health issue. Thus, obesity is much more than merely an aesthetic or bothersome issue, as excessive adipose tissue influences a myriad of processes in the body, including inflammation, with several authors pointing out the presence of chronic inflammation in obesity. Its association with osteoarthritis becomes even more important in the context of the significant increase of the elderly population, a trend that is present globally, with significant socio-economic implications [4, 19]. Treatment of advanced osteoarthritis is usually joint replacement, with numerous costs related to surgery as well as possible immediate or late post-operative complications [20]. In this respect, a potential early detection of complications could be welcomed in the effort to reduce hospitalisation costs for these patients. A better understanding of the post-operative inflammatory process in obese patients with a low level of chronic inflammation could provide a basis for reducing the cost of repeated post-operative screening.
Our study included two groups of consecutive patients undergoing large joint replacement, similar in mean age and length of hospital stay. The obese group included more women, which might be explained by an increased prevalence of both advanced osteoarthritis and obesity in females [3].
The measured mean fibrinogen levels showed no inter- or intra-group differences on either day of assessment, only slightly deviating from the normal range. For hsCRP, both groups showed significantly increased values on D2 compared to D1, a result in line with that of other similar studies [21]. Interestingly, the inter-group difference for hsCRP was significant only on D1, with greater mean values in obese patients, in agreement with the chronic inflammation theory [6, 22]. However, even though they have started out with higher pre-operative values, obese patients show a post-operative level of the marker which is similar to that of normoponderal patients.
Both IL-6 and hsCRP have been repeatedly shown to correlate with inflammatory activity, making them valuable indicators of the post-operative inflammatory response [21,22,23]. In our study, the two groups showed an increase of IL-6 on D2 (p = 0.0001), with no significant inter-group differences on D1. However, on D2, IL-6 levels in the obese group significantly exceeded those found in the normoponderal patients. Hence, these results did not comply with the expected pre-operative increase in inflammation for the obese patients, but do corroborate with the accepted acute phase marker status of IL-6.
One intriguing result was the decrease in mean values of TNF-alpha found in both the obese and the normal weight groups, and particularly for the obese patient on intra-group analysis for D2, especially in view of the increased values compared to normoponderals on D1. This is in line with the overexpression of the macrophage produced inflammatory mediator TNF-alpha in overweight and obesity, which seems to also be released by the adipose tissue [22]. However, we could not find an explanation or similar results in the literature for the decrease in TNF-alpha levels in the post-operative measurements [24, 25].
Because of its important clinical implications, an appropriate comprehension of the peri-operative changes in a patient’s inflammatory status has the potential to influence the therapeutic attitude. However, the studied markers are still not part of the routine monitoring, perhaps because of the costs implied, and further studies are needed to map out the specific changed in marker levels, based on a multitude of patient characteristics and associated conditions. Still, for obese patients in particular, there is a potential to increase the efficiency of management, with a clearer identification of possible complications and improved quality of life after large joint replacement surgery [23]. Unfortunately, the interpretation of our study is limited by the relatively low number of patients in both groups, and the lack of multiple post-operative measurements of the markers. However, the results highlight the relative absence of significant changes induced by obesity in the mean values of the markers obtained either pre- or post-operatively as compared to normal weight patients, and bring attention to peculiar changes in TNF-alpha levels, which warrant further clarification.
Our results confirmed the post-operative increase of serum levels for IL-6 and hsCRP found by other studies, in both normoponderal and obese patients, but pre-operatively we could not detect the same difference between the two groups in terms of IL-6, and only a slight difference in hsCRP levels, which does not support the inflammatory status we expected to find in the obese group. However, TNF-alpha levels were much higher in the obese pre-operatively, and actually decreased to levels similar to those of the normal weight patients on the measurement made within 24 hours after surgery. Overall, we failed to observe any significant postoperative differences in the mean values of the markers assessed, except those of IL-6, implying that serum levels of fibrinogen, hsCRP and TNF-alpha within 24 hours after large joint replacements are not influenced by the patient’s ponderal status.
References
Ng M, Fleming T, Robinson M et al (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945):766–781. https://doi.org/10.1016/S0140-6736(14)60460-8
Rappaport SM (2016) Genetic factors are not the major causes of chronic diseases. PLoS One 11(4):e0154387. https://doi.org/10.1371/journal.pone.0154387
Wen L, Kang JH, Yim YR et al (2016) Associations between body composition measurements of obesity and radiographic osteoarthritis in older adults: data from the Dong-gu study. BMC Musculoskelet Disord 17(1):192. https://doi.org/10.1186/s12891-016-1040-9
Reyes C, Leyland KM, Peat G et al (2016) Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: a population-based cohort study. Arthritis Rheumatol 68(8):1869–1874. https://doi.org/10.1002/art.39707
Greenberg AS, Obin MS (2006) Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr 83(2):461S–465S. https://doi.org/10.1093/ajcn/83.2.461S
Cicuttini FM, Wluka AE (2016) Not just loading and age: the dynamics of osteoarthritis, obesity and inflammation. Med J Aust 204(2):47. https://doi.org/10.5694/mja15.01069
Ma Z, Guo F, Qi J, Xiang W, Zhang J (2016) Meta-analysis shows that obesity may be a significant risk factor for prosthetic joint infections. Int Orthop 40(4):659–667. https://doi.org/10.1007/s00264-015-2914-4
Hughes SF, Hendricks BD, Edwards DR, Bastawrous SS, Middleton JF (2013) Lower limb orthopaedic surgery results in changes to coagulation and non-specific inflammatory biomarkers, including selective clinical outcome measures. Eur J Med Res 18(1):40. https://doi.org/10.1186/2047-783X-18-40
Motaghedi R, Bae JJ, Memtsoudis SG et al (2014) Association of obesity with inflammation and pain after total hip arthroplasty. Clin Orthop Relat Res 472(5):1442–1448. https://doi.org/10.1007/s11999-013-3282-2
Bay-Jensen AC, Reker D, Kjelgaard-Petersen CF, Mobasheri A, Karsdal MA, Ladel C, Henrotin Y, Thudium CS (2016) Osteoarthritis year in review 2015: soluble biomarkers and the BIPED criteria. Osteoarthr Cartil 24(1):9–20. https://doi.org/10.1016/j.joca.2015.10.014
Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S (2011) The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta 1813(5):878–888. https://doi.org/10.1016/j.bbamcr.2011.01.034
Mabey T, Honsawek S (2015) Cytokines as biochemical markers for knee osteoarthritis. World J Orthop 6(1):95–105. https://doi.org/10.5312/wjo.v6.i1.95
Imamura M, Ezquerro F, Marcon Alfieri F et al (2015) Serum levels of proinflammatory cytokines in painful knee osteoarthritis and sensitization. Int J Inflam 2015:329792. https://doi.org/10.1155/2015/329792
Roytblat L, Rachinsky M, Fisher A, Greemberg L, Shapira Y, Douvdevani A, Gelman S (2000) Raised interleukin-6 levels in obese patients. Obes Res 8(9):673–675. https://doi.org/10.1038/oby.2000.86
Nilsonne G, Lekander M, Åkerstedt T, Axelsson J, Ingre M (2016) Diurnal variation of circulating interleukin-6 in humans: a meta-analysis. PLoS One 11(11):e0165799. https://doi.org/10.1371/journal.pone.0165799
Singh G (2014) C-reactive protein and erythrocyte sedimentation rate: continuing role for erythrocyte sedimentation rate. Adv Biol Chem 4:5–9. https://doi.org/10.4236/abc.2014.41002
Ishii S, Karlamangla AS, Bote M, Irwin MR, Jacobs DR, Cho HJ, Seeman TE (2012) Gender, obesity and repeated elevation of C-reactive protein: data from the CARDIA cohort. PLoS One 7(4):e36062. https://doi.org/10.1371/journal.pone.0036062
Aronson D, Bartha P, Zinder O, Kerner A, Markiewicz W, Avizohar O, Brook GJ, Levy Y (2004) Obesity is the major determinant of elevated C-reactive protein in subjects with the metabolic syndrome. Int J Obes Relat Metab Disord 28(5):674–679. https://doi.org/10.1038/sj.ijo.0802609
Richter M, Trzeciak T, Owecki M, Pucher A, Kaczmarczyk J (2015) The role of adipocytokines in the pathogenesis of knee joint osteoarthritis. Int Orthop 39(6):1211–1217. https://doi.org/10.1007/s00264-015-2707-9
Grecu D, Antoniac I, Trante O, Niculescu M, Lupescu O (2016) Failure analysis of retrieved polyethylene insert in total knee replacement. Mater Plast 53(4):776–780
Honsawek S, Deepaisarnsakul B, Tanavalee A, Sakdinakiattikoon M, Ngarmukos S, Preativatanyou K, Bumrungpanichthaworn P (2011) Relationship of serum IL-6, C-reactive protein, erythrocyte sedimentation rate, and knee skin temperature after total knee arthroplasty: a prospective study. Int Orthop 35(1):31–35. https://doi.org/10.1007/s00264-010-0973-0
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y (2017) Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci 13(4):851–863. https://doi.org/10.5114/aoms.2016.58928
Yoon JR, Yang SH, Shin YS (2018) Diagnostic accuracy of interleukin-6 and procalcitonin in patients with periprosthetic joint infection: a systematic review and meta-analysis. Int Orthop 42(6):1213–1226. https://doi.org/10.1007/s00264-017-3744-3
Si H, Yang T, Zeng Y, Zhou Z, Pei F, Lu Y, Cheng J, Shen B (2017) Correlations between inflammatory cytokines, muscle damage markers and acute postoperative pain following primary total knee arthroplasty. BMC Musculoskelet Disord 18(1):265. https://doi.org/10.1186/s12891-017-1597-y
Langkilde A, Jakobsen TL, Bandholm TQ, Eugen-Olsen J, Blauenfeldt T, Petersen J, Andersen O (2017) Inflammation and post-operative recovery in patients undergoing total knee arthroplasty-secondary analysis of a randomized controlled trial. Osteoarthr Cartil 25(8):1265–1273. https://doi.org/10.1016/j.joca.2017.03.008
Acknowledgements
We are grateful to the staff of the Clinic of Orthopaedics and Traumatology of the Clinical County Hospital Mureș and to the staff of the Centre for Advanced Medical and Pharmaceutical Research of the University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureș for their help and involvement in this research project and for kindly providing facilities.
Funding
This study was supported by a private research grant from SC CATTUS SRL and involved the University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureș, contract no. 5068/26.04.2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tilinca, M.C., Zazgyva, A. & Pop, T.S. Differences in peri-operative serum inflammatory markers between normoponderal and obese patients undergoing large joint replacement for osteoarthritis—a descriptive study. International Orthopaedics (SICOT) 43, 1735–1740 (2019). https://doi.org/10.1007/s00264-018-4238-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4238-7