Abstract
Background
The use of custom-made 3D-printed prostheses for reconstruction of severe bone defects in selected cases is increasing. The aims of this study were to evaluate (1) the feasibility of surgical reconstruction with these prostheses in oncologic and non-oncologic settings and (2) the functional results, complications, and outcomes at short-term follow-up.
Methods
We analyzed 13 prospectively collected patients treated between June 2016 and January 2018. Diagnoses were primary bone tumour (7 patients), metastasis (3 patients), and revision of total hip arthroplasty (3 patients). Pelvis was the most frequent site of reconstruction (7 cases). Functional results were assessed with MSTS score and complications according to Henderson et al. Statistical analysis was performed using Kaplan-Meier and log-rank test curves.
Results
At a mean follow-up of 13.7 months (range, 6–26 months), all patients except one were alive. Oncologic outcomes show seven patients NED (no evidence of disease), one NED after treatment of metastasis, one patient died of disease, and another one was alive with disease. Overall survival was 100% and 80% at one and two years, respectively. Seven complications occurred in five patients (38.5%). Survival to all complications was 62% at two years of follow-up. Functional outcome was good or excellent in all cases with a mean score of 80.3%.
Conclusion
3D-printed custom-made prostheses represent a promising reconstructive technique in musculoskeletal oncology and challenging revision surgery. Preliminary results were satisfactory. Further studies are needed to evaluate prosthetic design, fixation methods, and stability of the implants at long-term.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent decades, thanks to the advances in chemotherapy, radiological and surgical techniques, limb-salvage surgery has been shown to be safe and effective for the management of primary and secondary bone tumors. Different reconstructive strategies may be used to replace bone defect after tumour removal, but each has its own specific indications and contraindications [1,2,3]. Modular endoprostheses are nowadays the most common method of reconstruction after resection of the long bones in the extremities for their availability, relative ease use, immediate fixation and long-term stability, early weight bearing, relatively rapid restoration of function, and acceptable cosmesis [3,4,5]. Modular prosthetic implants have been used also for pelvic reconstructions with acceptable results [6, 7]. With the advent of computer-aided design techniques and the improvement of 3D printing technology, in the last years, there is the possibility to reconstruct bone defects with personalized custom-made prostheses [8, 9]. These types of implants are specifically tailored for the defect and produced by electron beam melting (EBM) technology that allows the integration of the porous structure of the implant with the host bone [10,11,12]. The expectation at long-term follow-up is the reduction of mechanical complications, such as loosening and fracture/breakage compared to conventional prosthetic or allograft reconstructions [4, 10].
The aims of this study were to evaluate (1) the feasibility of surgical reconstruction with custom made 3D-printed prostheses in patients with oncologic and non-oncologic settings and (2) the functional results, complications, and outcomes at short-term follow-up.
Materials and methods
We analyzed patients treated with custom-made 3D-printed prosthesis, prospectively collected at the Authors’ institution from June 2016 to January 2018. The research has been performed in accordance with the Declaration of Helsinki. All patients or their relatives gave written informed consent to be included in scientific studies at the admission to the hospital. As this analysis consists of anonymized clinical routine data, Research Ethics Committee Approval was not necessary in our Institution. For all patients, we reviewed data regarding patient comorbidities, cancer type, disease duration, staging, and prognosis. Moreover, the analysis includes pre-operative history and course, imaging evaluation, surgical data, use of adjuvant treatments, oncologic outcome, complications, and their applied treatment.
Thirteen patients were included in the study: there were 3 males (23%) and 10 females (77%) with a mean age of 55.3 years (range, 10–77 years) at surgery. The demographic and oncological data are summarized in Table 1. All patients underwent pre-operative plain radiography, computerized tomography (CT), and magnetic resonance imaging (MRI) of the affected bone segment. Moreover, a high-resolution CT scan (thin layer 1 mm) was performed on every patient before the surgical procedure, possibly after removal of all previous implants in case of revision surgery. The acquired images in DICOM format were transferred to the manufacturing company, and an accurate 3D virtual image and project was created, via software, for each patient. In order to increase the stability of the reconstruction, screw holes and other tools for fixation of the prosthesis were designed together with engineers. In two cases of pelvic reconstruction, polyaxial screws were used on the back for connection with lumbar pedicle instrumentation. With the EBM technology, the previously designed titanium prosthesis is printed by the sintering of titanium powder and then adequately prepared before surgical implantation. The custom-made 3D-printed prostheses are provided with cutting guides and textured surfaces to improve their integration with bone and soft tissue. It took approximately three to four weeks for the design and manufacture of each personalized 3D-printed prosthesis. Three different implants were used: Promade (Lima, San Daniele del Friuli, Udine, Italy), Mt. Ortho (Catania, Italy), and C-Fit 3D® (Implantcast Ltd., Buxtehude, Germany).
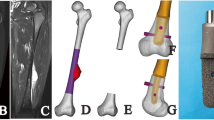
Clinical data and surgical procedures
Despite multiple surgeons contributing to patients’ management, the choice of operative strategy was based on multidisciplinary evaluation of our oncological team. The general indications for resection and reconstruction with custom-made 3D-printed prosthesis were (1) extensive bone loss and bone destruction that precluded the use of standard modular prostheses and (2) affecting site where massive allografts were the only alternative reconstructive method. Reasons for custom-made 3D-printed prosthetic implant were reported in Table 2. In summary, in three patients, it was used as revision implant after failure of total hip replacement, and in ten patients with oncologic disease as primary implant after resection of bone tumour (7 cases) or as revision implant after failed previous replacement (2 cases) or local recurrence (1 case). Revision surgery in oncologic setting was performed in one patient using an intercalary custom prosthesis after breakage of femoral intramedullary nail due to myeloma diaphyseal localization, in another patient as revision of mobilized modular stemmed acetabular cup and in a patient with recurrent giant cell tumor (GCT) of the distal tibia after multiple intralesional treatments. Anatomical sites of reconstruction were pelvis in seven cases and scapula, ulnar diaphysis, distal radius, calcaneus, distal tibia, and femoral diaphysis in one case each. Stem fixation was cemented in older patients with bone metastases and low bone stock (3 cases), while press-fit in younger patients and patients with primary bone tumours (10 cases). Histological diagnoses in ten patients with oncologic disease included chondrosarcoma in three (23%) patients, metastatic carcinoma in three (23%), osteosarcoma in two (15.3%), Ewing’s sarcoma and giant cell tumour in one each. According to the surgical staging system for musculoskeletal tumors, one benign tumour was classified as stage 3 and malignant tumours were classified as stage IIb (n = 6) and stage IIIb (n = 3). Adjuvant treatments were administered according to the primary cancer. Chemotherapy was performed in six patients with osteosarcoma, Ewing’s sarcoma, and metastatic lesion, whereas three of these received external beam radiotherapy also. The patient treated for recurrent GCT had pre-operative treatment with denosumab.
Post-operative assessments
All patients were followed by the rehabilitation center at our institution. Post-operative immobilization was obtained with pelvic-thigh brace in all cases of pelvic reconstruction: brace was positioned at 10° of abduction and fixed in extension for 1 month, then with flexion up to 90° for another month. Weight bearing was allowed after one week in case of cemented stem and after one month in case of press-fit stem. Immobilization for a month was obtained with brace at 15° of abduction after shoulder reconstruction, with Velpeau-brace after ulnar reconstruction, with Walker-brace after distal tibia reconstruction and with wrist-brace after distal radio reconstruction. Anti-thrombotic stockings and calf compression devices were routinely used for prophylaxis against deep vein thrombosis after lower limb or pelvic reconstruction. Routine follow-up examinations were performed with ambulatory checks every three months during the first three years after surgery, then every four months in the fourth years, then every six months for one year, and then annually. Follow-up evaluations included physical examination, radiographs, and disease-specific chest imaging. No patient was lost to follow-up. Oncologic results were evaluated according to local recurrence, metastasis, or death, and patients were classified as follows: (1) no evidence of disease at the latest routine check (NED); (2) disease free after treatment of local recurrence or metastasis (NEDrl or NEDm); (3) alive with disease, due to presence of local recurrence or metastasis (AWD); and (4) dead of disease (DWD). Survival was defined as the time from surgery to last follow-up or death. Complications were classified according to Henderson et al. [13] in type I (soft tissue failure), type II (aseptic loosening), type III (breakage), type IV (infection), and type V (local recurrence). Moreover, complications were considered as intra-operative, early (within 6 months post-operatively), and late (more than 6 months post-operatively). Functional results were assessed for all surviving patients using the Musculoskeletal Tumor Society (MSTS) functional rating system.
Statistical analysis
The categorical variables were expressed as percentages. Survival was analyzed using the Kaplan-Meier analysis. Comparison of the curves was done with the log-rank test. Differences were considered statistically significant when the p value was less than 0.05. The data were recorded in a Microsoft1 Excel1 2003 spreadsheet and analyzed using Med-Calc Software Version 11.1 (MedCalc Software, Mariakerke, Belgium).
Results
Operational outcomes
En-bloc resection was achieved in all patients with wide surgical margins. One patient had an osteosarcoma with suspicious tumour localization in the fifth lumbar vertebra; therefore, resection was extended and cement was used to fill the space between custom-prosthesis and host bone at the time of surgery. Two patients with oncologic pelvic reconstruction were stabilized with spino-pelvic instrumentation, whereas in the other two cases, iliac and sacral screws were used. No patient died of intra/perioperative complications.
Oncologic outcomes
At a mean follow-up of 13.7 months (range, 6–26 months), patients with oncologic disease were NED in seven cases, AWD in one case, NEDm in one case, and DWD in one case. One patient with distal radius osteosarcoma is without evidence of disease after surgical treatment of lung metastasis, one patient with stage IIb pelvic osteosarcoma died 15 months after surgery due to rapid tumour progression with bone and visceral metastases, while one patient with breast cancer metastasis is still alive with disease and she is under chemotherapy for other bone metastases. Overall survival was 100% and 80%, respectively, at 12 and 24 months (Fig. 1).
Complications
Complications occurred in 38.5% of cases (7 complications in 5/13 patients), at a mean time of 2.7 months (range, 0.3–12 months). Survival of the entire series to all complications was 62% at one year follow-up (Fig. 2a), whereas it was 72% considering major complications only (Fig. 2b). Type I complications occurred in four cases as post-operative (less than 1 month after surgery) wound dehiscence. Wound dehiscence was successfully treated with surgical wound debridement, antibiotic therapy per os, and VAC therapy in one patient (case no. 1 Table 2) with custom prosthesis as revision of THA failure. The patient with reconstruction of the calcaneus (case no. 13 Table 2) was successfully treated with surgical debridement and musculocutaneous flap without implant removal. In the other cases (pelvic reconstruction, case nos. 5 and 6 Table 2), wound dehiscence was treated with surgical debridement and antibiotic therapy, but successively, patients developed deep infection (type IV) at a mean of four months (range, 1–12 months). One of these was early diagnosed and then successfully treated with surgical debridement and musculocutaneous flap without implant removal. The other one developed a late infection (12 months after surgery) and was treated with surgical debridement, plastic flap, and oral antibiotic drugs without prosthesis removal due to poor general condition: in fact, the patient had multiple bone and visceral metastases and died three months later. We observed a higher incidence of infections in patients treated with pelvic reconstructions than other sites, even if without a significant difference at univariate analysis (p = 0.2667). Type II and type V complications never occurred, while type III complication was reported in one case (case no. 11). Patient treated with intercalary femur reconstruction had a periprosthetic fracture due to fall 45 days after surgery and was revised with a less invasive stabilization system (LISS) plate and bone allograft.
Functional results
After surgery, all patients experienced improvement in quality of life resulting from reduction or resolving of pain. The recovery of the affected limb function was assessed according to the MSTS score in all alive patients at the final follow-up. The mean MSTS score was 80.3%, with good (between 51 and 75%) or excellent (between 76 and 100%) in all patients. Analyzing separately the functional results, we observed a mean MSTS score of 64.5% (range, 57–70%) in patients treated of complex revision surgery in non-oncologic settings, 74% (range, 73–76%) in reconstructions after resection of pelvic bone tumours, and 88% (range, 80–93%) in patients with reconstruction of sites other than pelvis, with a statistically significant difference (p = 0.010) (Fig. 3).
Graphic visualization of functional results at MSTS score. Patients were divided in three groups based on site of reconstruction and oncologic setting, showing significant lower results in those with pelvic reconstruction (p = 0.010). Dots represent the last MSTS score of each patient, whereas horizontal lines represent the mean MSTS score of the group. One patient who died of disease was excluded
Discussion
The introduction of 3D printing technology increased the armamentarium of the orthopaedic surgeon in approaching large bone defects in complex revision surgery and musculoskeletal oncology. This technology may realize customizable patient-specific implants that could be used as alternative to massive bone allografts or in other sites where modular prosthesis are not available [10, 14]. The advantages include (1) the possibility to produce implants with complex shapes with a porous structure; the porous scaffold allows the growth of host bone inside the implant to achieve a stable reconstruction; (2) the increased accuracy of skeletal reconstruction reducing the risk of miss-match between allografts/adapted prostheses to host bone; (3) immediate stability with production of titanium prostheses that has sufficient mechanical strength to bear the body weight or allow full function of the body segment; and (4) the full availability than the allograft or other systems in most institutions [10, 14,15,16,17]. We present the preliminary results of our series of 13 patients treated with custom-designed 3D-printed prostheses in different oncologic and non-oncologic settings. These prostheses have been used for different types of demanding bone defects, showing satisfactory results in terms of surgical technique, operating time, safety, and functional outcomes. The complication rate is comparable to that of other complex reconstructions based on skeletal site.
Our study has some limitations. (1) There was heterogeneity of the patient population, and indications for all patients were either oncologic or revision; therefore, surgical exposures were not standardized and were dictated by the tumor location or pre-existing incisions. (2) Although this study is one of the largest series of custom-made 3D-printed prostheses, it has only 13 patients with adequate follow-up and heterogeneous surgical indications, thereby limiting the power of the series to show potentially statistically significant trends. On the other hand, this study provides interesting data and information for this new reconstructive technique. Moreover, considering the difficulty of analyzing large homogeneous series, a power analysis to determine how many patients in each group should be included to show a difference was not performed. (3) Heterogeneity and small sample size should be considered in the analysis of possible confounding variables. (4) The relatively short follow-up period of this study does not account for late complications that may arise as we follow these patients for a longer time. However, all the patients were prospectively analyzed and collected, reducing the risk of erroneous data or lost to follow-up. Larger multicentric studies should be realized for better evaluation of surgical indications, with comparison of different experienced centres at long-term follow-up.
The treatment of extensive acetabular bone loss and pelvic discontinuity is challenging in some cases of complex revisions. None of the commonly used reconstructive techniques has been able to provide optimal results in case of Paprosky 3A and 3B bone defects [18, 19]. In the recent years, several Authors have therefore begun to use custom-made 3D-printed prostheses in non-oncologic settings, with encouraging results [15, 20,21,22]. Some Authors reported encouraging results with custom 3D-printed tri-flanged acetabular implants for the management of severe acetabular defects: Taunton et al. retrospectively analyzed 57 patients with pelvic discontinuity reporting a stable implant at a mean follow-up of 65 months, despite high incidence of complications [21]. A significant improvement in functional scores and radiographic outcomes has been reported in other series of patients treated with custom-made 3D-printed pelvic reconstructions, with a complication rate ranging from 12.5 to 33.3% [23,24,25,26]. In our series, we reported similar results in three female patients (nos. 1, 2, and 3) with a mean age of 75 years (range, 68–79 years) treated for failed revised total hip arthroplasty. At a mean follow-up of 18 months (range, 8–24 months), only one complication (wound dehiscence) was observed and has been surgically treated without removal of the implant. At the last follow-up, all patients presented no sign of loosening at radiographs and the mean MSTS score was 64.5% (range, 57–70%). Considering the good results obtained in revision surgery of the pelvis, the use of 3D simulation and printing techniques have been recently extended in other fields of orthopedics, such as treatment of complex pelvic fractures [27, 28] or surgical planning and correction of technically challenging bone deformities [29, 30].
Concerning pelvic tumours, in the past, most of these cases were considered inoperable or the common method of managing was external hemipelvectomy [31]. Currently, with advances in radio/chemotherapy and surgical techniques, limb-salvage surgery has become an accepted treatment [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. Various biological and prosthetic methods have been used for pelvic reconstruction after tumor resection including arthrodesis, hip transposition, massive allograft/autograft, and different designed prosthetic implants [33, 34, 36]. However, the optimal reconstruction method remains controversial, especially in periacetabular area. Biological reconstruction has the theoretical potential of a permanent consolidation with host bone, even if the high rate of deep infection (range 15–55%) and mechanical failures (range 9–22%) significantly reduced their use in recent years [34, 37,38,39]. Prosthetic reconstruction has the advantages of allowing early mobilization, immediate and long-term stability with satisfactory cosmetic, and functional results [9, 35, 40, 41]. The advent of 3D printing technology may combine the benefits of both techniques, and recently, there has been a great increase in the use in oncologic settings [8, 9, 14, 41]. In 2002, Ozaki et al. [41] reported an experience with computer-aided custom-made Vitallium prostheses for pelvic reconstruction. In this early report, the Authors observed a high complication rate and poor functional results after hemipelvic resection and prosthetic reconstruction. Dai et al. [9] reported in 2007 their experience in using custom-made 3D-printed prostheses after pelvic resection. They analyzed ten patients treated for bone tumours involving the acetabular area at a mean age of 48 years. Despite the rate of complications remaining high compared to previous reports, functional results were good in more than 70% of the cases at a mean of 34-month follow-up [9]. Wang et al. [42] recently reported their experience in 11 treated for malignant tumours (localized sarcoma or solitary metastasis) in the periacetabular region. They used a 3D-printed prosthesis that precisely matched the residual part of the iliac crest, sacroiliac joint, or sacrum (fixed with cancellous and locking screws) and the pubis, searching a complete restoration of the pelvic ring. Liang et al. [14] reported the largest series of patients (35 cases) treated reconstructed with custom-made 3D-printed prostheses after pelvic resection for bone tumours. Types of pelvic resections were the following: type I in three cases, type II + III in 12 cases, type I + II in five cases, type I + II + III in two cases, type I + II + IV in ten cases, and type I + II + III + IV in 3 cases. They used three different prosthetic concepts. A 3D-printed iliac prosthesis of adequate size fixed with sacral, ischium, and pubic screws was used in type I resections to restore the continuity of the pelvic ring. A 3D-printed hemipelvic prosthesis of suitable size, augmented with bone cement and conventional total hip arthroplasty, was used for resections including acetabular area. The fixation was obtained with perfect fit to the contour of residual ilium, long sacral cancellous screws, and two or more cortical screws. A 3D-printed prosthesis with screw-rod connection has been used for larger reconstructions of the entire hemipelvis [14]. In our experience, we adopt a slightly different protocol to decide the type of pelvic reconstruction after bone tumor resection, primarily based on the proximal resection level of the ilium (Fig. 4). In pelvic resections involving the entire iliac bone or part of the sacrum, we prefer a reconstruction with a custom-made 3D-printed prosthesis with spinopelvic stabilization (Fig. 5a). The same choice when the residual part of the ilium is not adequate and sufficient to accommodate a modular stemmed acetabular cup (Fig. 5b). In type I–II resections with a good support of the iliac bone, we prefer a modular prosthesis with stemmed acetabular cup (Fig. 5c). A coarctation is used in specific cases such as young patients with limited muscle removal and limited shortening expected or old patients with poor general conditions (Fig. 5d).
Explicative cases of pelvic reconstruction based on our decision-making algorithm. a Twenty-six-year-old female, with stage III osteosarcoma of the iliac wing treated with type I pelvic resection and reconstruction with 3D-printed custom prosthesis and spinopelvic fixation (case no. 6 of the present series). b Fifty-three-year-old female, with Ewing’s sarcoma of the pelvis treated with type I–II pelvic resection and reconstruction with 3D-printed custom prosthesis and spinopelvic fixation (case no. 7 of the present series). c Seventy-two-year-old male, with peripheral chondrosarcoma of the acetabular area treated with type II pelvic resection and reconstruction using modular prosthesis with stemmed acetabular cup. d Fifty-eight-year-old male, with grade 2 chondrosarcoma of the acetabulum treated with type II resection and ileo-femoral coarctation considering the limited shortening expected and good muscle preservation
Other field of application of custom-made 3D-printed prostheses includes the reconstruction after bone resection for tumour in particular skeletal segments in which there are no available standard modular prostheses, as an alternative to massive allograft. In literature, there are described small series and case reports reporting custom-made prosthetic reconstructions of the scapula, clavicula, radius, vertebral body, and calcaneus [16, 43,44,45]. In most of the cases, immediate stability and good cosmetic appearance have been achieved with these anatomical reconstructions, even if the follow-up is usually too short in order to establish functional results and complication rate. In our series, we have reported six cases of custom-made 3D-printed prosthetic reconstructions of unusual sites (scapula, intercalary ulna, distal radius, calcaneus, distal tibia, and intercalary femur). At a mean follow-up of 9.4 months (range 6–17 months), two complications were observed: a periprosthetic fracture after accidental traumatic fall and a wound dehiscence which however did not require removal of the implant. Functional results were satisfactory in all cases, with an average MSTS score of 88% (range, 80–93%).
Conclusions
The use of 3D-printed titanium prostheses is growing in musculoskeletal oncology and revision surgery. This technology may be useful to obtain a complete restoration of the bone defect and acceptable functional results, even if the complication rate remains high in difficult sites such as the pelvis. We believe that custom-made 3D-printed prostheses represent today a promising reconstructive technique, maintaining however the correct indications for their use in musculoskeletal oncology and challenging revision surgery. Further studies are needed to validate the more appropriate design of prosthesis and its fixation to the host bone (especially in pelvic reconstructions), in terms of stability at long-term follow-up.
References
Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW (1996) Long term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res 324:86–97
Zeegen EN, Aponte-Tinao LA, Hornicek FJ, Gebhardt MC, Mankin HJ (2004) Survivor analysis of 141 modular metallic endoprostheses at early follow-up. Clin Orthop Relat Res 420:239–250
Pala E, Trovarelli G, Calabrò T, Angelini A, Abati CN, Ruggieri P (2015) Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res 473(3):891–899
Pala E, Trovarelli G, Angelini A, Maraldi M, Berizzi A, Ruggieri P (2017) Megaprosthesis of the knee in tumor and revision surgery. Acta Biomed 88(Supplement 2):129–138
Ahlmann ER, Menendez LR, Kermani C, Gotha H (2006) Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br 88:790–795
Ji T, Guo W, Yang RL, Tang XD, Wang YF (2013) Modular hemipelvic endoprosthesis reconstruction–experience in 100 patients with mid-term follow-up results. Eur J Surg Oncol 39:53–60
Guo W, Li D, Tang X, Yang Y, Ji T (2007) Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res 461:180–188
Sun W, Li J, Li Q, Li G, Cai Z (2011) Clinical effectiveness of hemipelvic reconstruction using computer-aided custom-made prostheses after resection of malignant pelvic tumors. J Arthroplast 26:1508–1513
Dai KR, Yan MN, Zhu ZA, Sun YH (2007) Computer-aided custom-made hemipelvic prosthesis used in extensive pelvic lesions. J Arthroplast 22:981–986
Shah FA, Snis A, Matic A, Thomsen P, Palmquist A (2016) 3D printed Ti6Al4V implant surface promotes bone maturation and retains a higher density of less aged osteocytes at the bone-implant interface. Acta Biomater 30:357–367
Sing SL, An J, Yeong WY, Wiria FE (2016) Laser and electron- beam powder-bed additive manufacturing of metallic implants: a review on processes, materials and designs. J Orthop Res 34:369–385
Xiu P, Jia Z, Lv J, Yin C, Cheng Y, Zhang K, Song C, Leng H, Zheng Y, Cai H, Liu Z (2016) Tailored surface treatment of 3D printed porous Ti6Al4V by microarc oxidation for enhanced osseointegration via optimized bone in-growth patterns and interlocked bone/implant Interface. ACS Appl Mater Interfaces 8:17964–17975
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, Hornicek FJ, Temple HT, Ruggieri P, Letson GD (2011) Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am 93(5):418–429
Liang H, Ji T, Zhang Y, Wang Y, Guo W (2017) Reconstruction with 3D-printed pelvic endoprostheses after resection of a pelvic tumour. Bone Joint J 99-B:267–275
Wong KC, Kumta SM, Geel NV, Demol J (2015) One-step reconstruction with a 3D- printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg 20:14–23
Xu N, Wei F, Liu X, Jiang L, Cai H, Li Z, Yu M, Wu F, Liu Z (2016) Reconstruction of the upper cervical spine using a personalized 3D- printed vertebral body in an adolescent with Ewing sarcoma. Spine (Phila Pa 1976) 41:E50–E54
Chen X, Xu L, Wang Y, Hao Y, Wang L (2016) Image-guided installation of 3D-printed patient-specific implant and its application in pelvic tumor resection and reconstruction surgery. Comput Methods Prog Biomed 125:66–78
DeBoer DK, Christie MJ, Brinson MF, Morrison JC (2007) Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am 89:835–840
Schatzker J, Wong MK (1999) Acetabular revision: the role of rings and cages. Clin Orthop Relat Res 369:187–197
Li G, Wang L, Pan W, Yang F, Jiang W, Wu X, Kong X, Dai K, Hao Y (2016) In vitro and in vivo study of additive manufactured porous Ti6Al4V scaffolds for repairing bone defects. Sci Rep 6:34072
Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ (2012) Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res 470(2):428–434
Wyatt MC (2015) Custom 3D-printed acetabular implants in hip surgery: innovative breakthrough or expensive bespoke upgrade? Hip Int 25(4):375–379
Li H, Qu X, Mao Y, Dai K, Zhu Z (2016) Custom acetabular cages offer stable fixation and improved hip scores for revision THA with severe bone defects. Clin Orthop Relat Res 474(3):731–740
Berasi CC, Berend KR, Adams JB, Ruh EL, Lombardi AV Jr (2015) Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res 473(2):528–535
Friedrich MJ, Schmolders J, Michel RD, Randau TM, Wimmer MD, Kohlhof H, Wirtz DC, Gravius S (2014) Management of severe periacetabular bone loss combined with pelvic discontinuity in revision hip arthroplasty. Int Orthop 38(12):2455–2461
Wind MA Jr, Swank ML, Sorger JI (2013) Short-term results of a custom triflange acetabular component for massive acetabular bone loss in revision THA. Orthopedics 36(3):e260–e265
Hung CC, Li YT, Chou YC, Chen JE, Wu CC, Shen HC, Yeh TT (2018) Conventional plate fixation method versus pre-operative virtual simulation and three-dimensional printing-assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int Orthop. https://doi.org/10.1007/s00264-018-3963-2
Zhuang Y, Cao S, Lin Y, Li R, Wang G, Wang Y (2016) Minimally invasive plate osteosynthesis of acetabular anterior column fractures using the two-incision minimally invasive approach and a preshaped three dimension plate. Int Orthop 40(10):2157–2162
Wan J, Zhang C, Liu YP, He HB (2018) Surgical treatment for shepherd's crook deformity in fibrous dysplasia: there is no best, only better. Int Orthop. https://doi.org/10.1007/s00264-018-4074-9
Shi J, Lv W, Wang Y, Ma B, Cui W, Liu Z, Han K (2018) Three dimensional patient-specific printed cutting guides for closing-wedge distal femoral osteotomy. Int Orthop. https://doi.org/10.1007/s00264-018-4043-3
Senchenkov A, Moran SL, Petty PM, Knoetgen J III, Clay RP, Bite U, Barnes SA, Sim FH (2008) Predictors of complications and outcomes of external hemipelvectomy wounds: account of 160 consecutive cases. Ann Surg Oncol 15(1):355–363
Puri A, Gulia A, Pruthi M (2014) Outcome of surgical resection of pelvic osteosarcoma. Indian J Orthop 48:273–278
Ozaki T, Hillmann A, Winkelmann W (1998) Treatment outcome of pelvic sarcomas in young children: orthopaedic and oncologic analysis. J Pediatr Orthop 18:350–355
Angelini A, Calabrò T, Pala E, Trovarelli G, Maraldi M, Ruggieri P (2015) Resection and reconstruction of pelvic bone tumors. Orthopedics 38(2):87–93
Angelini A, Guerra G, Mavrogenis AF, Pala E, Picci P, Ruggieri P (2012) Clinical outcome of central conventional chondrosarcoma. J Surg Oncol 106(8):929–937
Mavrogenis AF, Angelini A, Drago G, Merlino B, Ruggieri P (2013) Survival analysis of patients with chondrosarcomas of the pelvis. J Surg Oncol 108(1):19–27
Traub F, Andreou D, Niethard M, Tiedke C, Werner M, Tunn PU (2013) Biological reconstruction following the resection of malignant bone tumors of the pelvis. Sarcoma 2013:745360
Delloye C, Banse X, Brichard B, Docquier PL, Cornu O (2007) Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am 89:579–587
Ozaki T, Hillmann A, Bettin D, Wuisman P, Winkelmann W (1996) High complication rates with pelvic allografts. Experience of 22 sarcoma resections. Acta Orthop Scand 67:333–338
Zang J, Guo W, Yang Y, Xie L (2014) Reconstruction of the hemipelvis with a modular prosthesis after resection of a primary malignant peri-acetabular tumour involving the sacroiliac joint. Bone Joint J 96-B:399–405
Ozaki T, Hoffmann C, Hillmann A, Gosheger G, Lindner N, Winkelmann W (2002) Implantation of hemipelvic prosthesis after resection of sarcoma. Clin Orthop Relat Res 396:197–205
Wang B, Hao Y, Pu F, Jiang W, Shao Z (2018) Computer-aided designed, three dimensional-printed hemipelvic prosthesis for peri-acetabular malignant bone tumour. Int Orthop 42(3):687–694
Imanishi J, Choonga PFM (2015) Three-dimensional printed calcaneal prosthesis following total calcanectomy. Int J Surg Case Rep 10:83–87
Park JW, Kang HG, Lim KM, Kim JH, Kim HS (2018) Three-dimensionally printed personalized implant design and reconstructive surgery for a bone tumor of the calcaneus: a case report. JBJS Case Connect 8(2):e25
Fan H, Fu J, Li X, Pei Y, Li X, Pei G, Guo Z (2015) Implantation of customized 3-D printed titanium prosthesis in limb salvage surgery: a case series and review of the literature. World J Surg Oncol 13:308
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Study design: case series: level of evidence 4
Rights and permissions
About this article
Cite this article
Angelini, A., Trovarelli, G., Berizzi, A. et al. Three-dimension-printed custom-made prosthetic reconstructions: from revision surgery to oncologic reconstructions. International Orthopaedics (SICOT) 43, 123–132 (2019). https://doi.org/10.1007/s00264-018-4232-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4232-0