Abstract
Purpose
Management of acute open tibial fractures with critical bone defect remains a challenge in trauma surgery. Few and heterogeneous cases have been reported about the treatment with the induced membrane technique.
Methods
We prospectively evaluated three patients treated with the induced membrane technique for acute Gustilo IIIB tibial fractures with critical bone defect. Success treatment was defined by bone union with patient pain free. Clinical and radiological evaluations were performed regularly until healing, then annually and with a minimum follow-up of five years.
Results
In all patients but one, a success was recorded, respectively, at four and six months. These two patients were pain free until the final follow-up, and no graft resorption or secondary complications related to the index surgery were observed. The third case was managed successfully with a bone transport technique.
Conclusion
The induced membrane technique is an alternative good option for the treatment of these severe lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of critical size bone defects of the medium/distal tibia in open fractures is a challenge because of the limited soft tissue, the subcutaneous location of the bone, the poor vascularity, and the high risk of infection [1]. Several techniques have been proposed, such as bone transport and free vascularized bone transfers. These techniques are associated with long healing times, and the complication rate ranges between 24 and 80% [2, 3]. Masquelet et al. developed the concept of the “induced membrane”, where a membrane induced by a foreign body acts as a biological chamber that prevents graft resorption by providing vascularization and growth factors [4]. One of the largest case series reporting results of the technique achieved a 90% rate of union in post-traumatic diaphyseal long bone reconstructions (61 tibia) of which 50% were infected [5]. However, few cases are reported in literature about the management of acute open fracture with critical size tibial bone defects mainly in post-acute phase [6,7,8,9,10,11,12,13]. Most of these cases are included in retrospective studies with a high heterogeneity of lesions treated and poor detailed patient information [14].
The aim of this prospective study is to present a preliminary results at medium-term follow-up of Masquelet technique for the treatment in acute phase of Gustilo IIIB tibial fracture with critical bone loss. The hypothesis is that Masquelet technique is an effective method to treat these lesions.
Patients and methods
Between January 2011 and May 2012, three consecutive patients were treated at the Division of Orthopaedic and Traumatology of University of Insubria, Hospital di Circolo, Varese—Italy for a Gustilo IIIB fracture of the medium/distal tibia with the Masquelet technique. Main inclusion criteria were: adult patients, acute traumatic Gustilo IIIB tibial fractures, critical size bone defect, at least one intact arterial vessel evaluated with angio-CT, and preserved sensitivity of the foot. Patients with a history of metabolic disease, malignant disease, and smoking were excluded.
All Masquelet procedures were performed by a single surgeon (MR) with a special interest in this technique. Surgical treatment adhered to a standardized protocol. Intravenous antibiotic therapy with vancomycin 500 mg × 4/die and meropenem 1 g × 3/die was started immediately at the admission in hospital. The leg fracture was treated with an accurate debridement of the contaminated tissues and stabilized with an external fixator (Hoffman II, Stryker, USA). According to the patient general conditions, the bone defect was filled with antibiotic cement containing gentamicin (Cemex Gent; Tecres spa, Italy) customized as described by Masquelet et al. [4, 15], and the soft tissue defect was reconstructed with a vascularized free flap. If the patient was haemodynamically unstable, the exposure was partially closed and covered with non-adherent gauzes, and within one week, the antibiotic cement implant and the soft tissue reconstruction were performed. The antibiotic therapy was continued at least for six weeks. Routine serum levels of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and white blood cell count (WBC) were checked every week. The second stage was performed when there were no clinical signs of infection (localized erythema, warmth, exudate, and pyrexia) and the haematological inflammatory markers returned to normal values and remained constant after the antibiotic suspension for two weeks. At that time, the external fixator was removed and the limb was braced in a cast for further two weeks to allow for pin-track healing. According to the general conditions, partial weight-bearing with crutches was allowed immediately.
The second stage consisted of elevation of the flap in a mini-open fashion opposite to the vascular pedicle, opening of the induced membrane longitudinally and antibiotic cement removing using osteotomies. Samples for microbiological culture were taken and all cases resulted negative. The medullary canal was cleaned and curetted. Tibia was stabilized with an internal fixation and the bone defect was filled with a composite graft: autologous bone harvested from the contralateral femur using the Reamer–Irrigation–Aspirator (RIA) system (Synthes, USA), allograft or bone substitute, and one dose of recombinant human bone morphogenetic protein-7 (rh-BMP-7; OP-1™, Olympus Biotech Corporation, USA). The induced membrane was closed with absorbable sutures, a superficial drainage was placed in the subcutaneous tissue in all cases, but the first and subcutaneous and skin layers were sutured. One week after surgery, antibiotic therapy (ciprofloxacin 500 mg × 2/die per os) was discontinued on the basis of negative microbiological cultures.
Full weight-bearing was not allowed until a radiographic healing was achieved. Bone union was defined by evidence at X-rays of three of the four cortices continuous and at least 2 mm thick with the patient pain free. We scheduled clinical and radiographic evaluations every month until bone healing, one year from the second procedure, and then annually. The patients were followed up for a minimum of five years. This study was approved by the institutional review board.
Case 1
A 31-year-old man sustained a work accident, boulder fallen on the right leg, and a Gustilo IIIB distal diaphyseal fracture (AO 42-C3) (Fig. 1a). The first procedure was performed in emergency. The bone defect measured 6.4 cm and a contralateral latissimus dorsi free flap was used to cover the soft tissue defect (Fig. 1b). At three months, the second step was performed and a locking plate (Axos, Stryker, USA) was used to stabilize the tibia. No drainage was placed (Fig. 1c, d). At 15 days, the wound was still opened with outer drainage of deep haematoma. Several debridement were necessary, and the microbiological culture was positive for Pseudomonas aeruginosa. Antibiotic therapy (gentamicin 400 mg × 1/die for 3 weeks and then colistin 200.0000 IU × 3/die for 3 weeks) and VAC (vacuum-assisted closure) therapy were started. At one month, the plate was removed and the tibia stabilized with an external fixation. After two months, a partial resorption of the graft was observed, and labeled leukocyte bone scan was positive. We then converted the treatment to a bone transport using an Ilizarov circular ring apparatus after a radical debridement of the composite graft. After 23 months, the external fixation was removed when docking site union and complete corticalization of bone regenerate were observed. At latest follow-up, the patient complained occasionally moderate ankle pain and stiffness (Fig. 1e). He refused any further treatment.
a A right leg Gustilo IIIB distal diaphyseal fracture (AO 42-C3). First step of the Masquelet technique. b Soft tissue coverage with latissimus dorsi free flap. Post-op X-rays with the cement spacer bridging the tibia ends and a Steinmann pin aligning the fibula. Second step of the Masquelet technique. c Final intra-operative view after tibia stabilization with a medial locking plate and membrane closure with absorbable stiches (white arrows). d X-rays with leg normoaligned and the graft filling the defect. e X-rays at 6-year follow-up. Docking site union and complete corticalization of bone regenerate after bone transport
Case 2
A 27-year-old man was struck by a forklift during his working activity. He sustained a right leg Gustilo IIIB distal diaphyseal fracture (AO 42-C3) with a bone loss of 7 cm (Fig. 2a, b). The first procedure was performed immediately as usual and the plastic surgeon covered the soft tissue defect with the contralateral latissimus dorsi free flap the day after (Fig. 2c, d). The second procedure was performed after three months and the tibia was stabilized with an intramedullary nail (T2, Stryker, USA) (Fig. 3a–d). Full weight-bearing and bone union were achieved at four months with the patient pain free. At 18 months, he returned to a recreational activities like running and jumping that maintained constant until the final follow-up (Fig. 3e, f).
a A right leg Gustilo IIIB distal diaphyseal fracture (AO 42-C3). First step of the Masquelet technique. b Tibial bone defect measured 7 cm. c Radical debridement and latissimus dorsi free flap in place. d X-rays show the cement spacer inside the bone defect and the tibia stabilized with an external fixation
Second step of the Masquelet technique. a Elevation of the latissimus dorsi free flap. Continuity between periosteum and membrane. b The membrane is thick and well vascularized all around the cememnt spacer. c Membrane closure. X-rays post-op (d) and at 6 years with a good integration and remodeling of the graft. d Functional result
Case 3
A 53-year-old male was run over and presented with an open-book pelvis fracture, a Gustilo IIIA left femur diaphyseal fracture (AO 32-A3) and a Gustilo IIIB left distal tibia meta-epiphyseal fracture (AO 43-C3) (Fig. 4a). In emergency, the open book was closed with external fixation, the femur fracture was stabilized with a nail, and the leg fracture was treated with pinning, and an external fixator bridging the ankle joint. When the general conditions improved at five days, the fracture was revised according to the protocol and the soft tissue defect was reconstructed with an extended free gracilis flap harvested from the contralateral thigh (Fig. 4b–e). The length of bone loss was 6 cm. At three months after the trauma, the second procedure was performed and a reamed retrograde Valor® fusion nail (Wright Medical technology Inc., USA) was implanted. The bone defect was filled as usual but with a bovine nanocrystalline carbonated hydroxyapatite scaffold (Orthoss®, Geisthich Pharma AG, Switzerland) as scaffold because the patient refused allograft (Fig. 5a–d). Full weight-bearing started at five months. At six months, the graft appeared completely integrated, but he complained persistent subtalar discomfort due to a non-complete subtalar fusion. The patient then underwent to a revision of subtalar arthrodesis with autologous cancellous omolateral iliac crest bone graft and stabilization with a 6.5-mm Acutrak® Plus compression screw (Acumed, USA). No more pain during walking was reported during the follow-up (Fig. 5e).
a A meta-epiphyseal Gustilo IIIB fracture of the left distal tibia (AO 43-C3). First step of the Masquelet technique. b Tibial bone defect sized about 6 cm after debridement. On the right side, the talar dome is visualized. c Customized cement spacer bridging tibia and talus. d Soft tissue coverage with gracilis free flap. e X-ray aspect of the cement spacer in antero-posterior and lateral view. Proper alignment and length of the limb obtained with external fixation (reprinted from Ronga M, Ferraro S, Fagetti A, et al. Injury. 2014 Dec;45 Suppl 6:S111-5, with permission from Elsevier)
Second step of the Masquelet technique. a After removal of the cement spacer, the membrane bridged the bony extremities showing its vascularity. b The composite graft implanted in the defect. c Closure of the membrane with separated stitches and drainage in place. d X-ray aspect of composite graft and nail in antero-posterior and lateral view. A complete filling of the defect is obtained maintaining correct limb alignment and length. e X-rays at 5 years. Bone healing and remodeling, integration of the graft on both sides, and complete talar fusion (a–d, reprinted from Ronga M, Ferraro S, Fagetti A, et al. Injury. 2014 Dec;45 Suppl 6:S111-5, with permission from Elsevier)
Discussion
Management of acute traumatic critical size bone loss of the limbs remains a challenge in trauma surgery. The most common methods of treating are the free vascularized bone graft and the bone transport using the Ilizarov technique [2, 3]. These techniques require specialized training and equipment and are associated with long healing time and several complications. The main complications for vascularized bone transfer are necrosis due to anastomosis failures, stress fracture, and infection at both donor and recipient sites. The main complications for bone transport are long periods of treatment, pain accompanying the transport, pin tract infection, reflex sympathetic dystrophy, non-union at the docking site, and a rate of revision surgery up to 23.8% [2, 3].
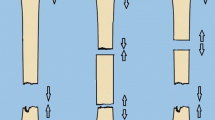
Masquelet et al. [4] proposed a surgical alternative option developing the concept of the “induced membrane”. This technique consists of a two-step reconstructive procedure. The first step comprises aggressive debridement of the necrotic and potential infected tissue, stabilization of the bony segment with an external fixation, implantation of a cement spacer that induces a pseudosynovial membrane formation and prevents fibrous tissue invasion of the defect area, and soft tissue coverage or free tissue transfer, if needed. The pseudosynovial membrane acts as a biological chamber that prevents the subsequent bone graft resorption by providing vascularization and growth factors. The second step is performed approximately six to eight weeks later and comprises removal of the cement spacer and filling of the cavity with morcellized cancellous bone autograft harvested from the iliac crest. A recent systematic review reported a union rate of 89.7% and an infections rectified in 91.1% of cases [14]. The main complications were superficial (4.9%) and deep surgical site infections (4.4%), failure of one of the two steps (persistence of infections or non-unions, 18%), with subsequent requirement for further surgery [14]. The average time of healing of 1-cm bone defect being 1.24 months is slightly faster compared to bone transport [16]. For defects over 20 cm, Masquelet technique has the advantage that the healing time is independent from the defect length comparing it to bone transport [16]. Our results confirm these data.
We adopted the Masquelet technique in our patients because of the extensive soft tissue damage and bone loss. Key points were: immediate radical debridement or within one week, antibiotic cement spacer that delivers locally antibiotics, coverage of the defect with a healthy and vascularized soft tissue that converts an open fracture to a closed one and delivers systemic antibiotics locally, external stabilization that reduces the risk of infections in acute phase [17, 18]. Such a strategy proved to be safe, as demonstrated by negative microbiological cultures at second stage, and reproduced the same conditions as for the aseptic non-unions. It seems that the quality of the initial debridement, although difficult to quantify, is the main factor of prognosis. Antibiotic therapy should only be considered as additional treatment for complete debridement [7, 9, 15, 19,20,21].
The optimal timing for cement spacer duration has not yet been definitively determined and theoretically depends on the number of arteries that vascularize the leg and support membrane formation [15, 17]. Current recommendations for spacer exchange range from four to eight weeks, but we waited further four weeks since our patients injured at least one artery during the trauma [15, 17].
We used an internal fixation at the second procedure to avoid problems and complication related to the external fixation as described in the original technique: long time to weight-bearing, secondary fractures, infection at the pin holes [4, 8, 15]. However, we chose an external fixation at the first procedure to reduce the risk of infection that was reported by Apart et al. [7] in 5/12 cases using an intramedullary nailing. The main drawback is the placement of a large foreign object in the medullary canal with the potential to maintain infection [9]. We suppose that the superficial haematoma, not aspirated by the drainage, and the early bacterial colonization of the plate caused the failure of the first case treated. After new debridement, including removal of the grafts and the plate, a bone transport was successful without any further problems. At the beginning of our experience, we did not use the drainage to avoid a potential aspiration of BMPs when eluted in the graft [17, 22]. On the basis of this experience, we suggest to put a drainage in the subcutaneous tissue since a meticulous procedure allows a nicely closure of the membrane and then avoids a possible aspiration of growth factors. We continued our experience with the intramedullary nailing because it allows for axial stimulation of the bone graft and then earlier weight-bearing, keeps the segments aligned, reduces the volume of graft needed filling the center of the defect, prevents secondary fractures, and seems to have shorter treatment times when compared to plating [8].
We used as cells source RIA instead of iliac crest graft, as described in the original technique [4, 15], due to the high complication rate for massive iliac crest bone grafting (19.37%) [23, 24] and to have a second chance of its successive use as in our third case (talar fusion procedure) [12].
The composite graft was used to obtain all factors needed for bone healing: osteoproductive cells derived from RIA, osteoconductive allograft/scaffold, and osteoinductive growth factors (BMP-7) [25, 26]. The role of recombinant growth factors with the induced membrane is still debated. However, in a prospective, controlled, randomized study of 450 patients with an open tibial fractures, the use of BMPs reduced significantly the infection rate [27].
Few cases have been reported in literature about the management of critical size tibial bone defects in open fractures and in emergency setting. Confounding factors, including the lack of distinction between post-traumatic defects (acute bone loss) and aseptic nonunion following a fracture and between the results achieved, do not allow to define the potential of Masquelet technique in such lesions [6,7,8, 10, 11, 13, 25]. Taylor et al. [13] in a retrospective study reported the results of 69 patients (35 tibia) with bone loss after open fracture. Union was obtained in 82.6% of the cases, but the authors did not specify when they performed the Masquelet technique (acute or chronic phase), reporting only an overall average time between the initial debridement and final fixation of 27.6 ± 61.6 days (range, 0–385) [13]. They were unable to determine any statistically significant correlation between any of variables such as site and Gustilo type of lesion, fixation constructs, treatment methods, etc. Morris et al. [10] in a retrospective study on 12 patients started the Masquelet technique within one week from the trauma in seven of them. In the whole case series, bony union was achieved in only five patients. Five patients experienced infective complications during treatment, with two requiring amputation because of severe infection. Several comments can be raised on this study. The average interval to the first procedure was 39.8 days and, excluding the first seven patients, was 90.2 days (range, 15–329). The success of this technique is based on a quick and radical debridement of the necrotic and potentially infectious tissues combined with implantation of antibiotic cement and early coverage with a vascularized free flap [9, 17]. Vancomycin was added to the cement spacer only in seven cases and its concentration was not reported. In 11/12 patients, the authors used immediately an internal fixation while it is advisable in the first stage an external fixation to prevent a bacterial colonization [4, 15]. Five patients developed infective complications before the second stage but they were not revised with a metal implant removing, further debridement, and new antibiotic cement spacer as suggested [4, 9, 15]. Seven of twelve patients were smokers, and this variable is considered a negative prognostic factor for all the several limb reconstruction procedures [4, 9, 15].
Major strengths of the present study are its prospective nature, that a single fully trained surgeon performed the Masquelet technique in a single centre, that we accurately selected our patients and followed them with the same protocol. Limitations are the relatively small number of patients and the lack of a comparison with traditional techniques. Acute critical bone defects are rare: the incidence is around 0.4% of all patients admitted to hospital with a fracture [1]. It would have been next to impossible for a single centre to collect a number of patients large enough to have two groups.
In conclusion, Masquelet technique appears to be an alternative limb-salvaging good option with a high success rate for the treatment of critical size bone defects of the tibia following a Gustilo IIIB acute fracture. It can be performed easily and by surgeons with varying experience and capability and does not require special device. It does not preclude the chance to switch to other procedures in case of failure. Multicenter controlled comparative trials are needed to define the real potential of this technique over other in treatment of acute cases.
References
Molina CS, Stinner DJ, Obremskey WT (2014) Treatment of traumatic segmental long-bone defects: a critical analysis review. JBJS Rev 2(4):1. https://doi.org/10.2106/JBJS.RVW.M.00062
El-Gammal TA, Shiha A, El-Deen M, El-Deen MA, El-Sayed A, Kotb MM, Addosooki AI, Ragheb YF, Saleh WR (2008) Management of traumatic tibial defects using free vascularized fibula or ilizarov bone transport: a comparative study. Microsurgery 28(5):339–346. https://doi.org/10.1002/micr.20501
Yokoyama K, Itoman M, Nakamura K, Tsukamoto T, Saita Y, Aoki S (2001) Free vascularized fibular graft vs Ilizarov method for post-traumatic tibial bone defect. J Reconstr Microsurg 17(1):17–25
Masquelet AC, Fitoussi F, Bégué T, Muller GP (2000) Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet 45:346–353
Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC (2012) Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumatol Surg Res 98:97–102. https://doi.org/10.1016/j.otsr.2011.11.001
Azi ML, Teixeira AA, Cotias RB, Joeris A, Kfuri M Jr (2016) Membrane induced osteogenesis in the management of posttraumatic bone defects. J Orthop Trauma 30:545–550. https://doi.org/10.1097/BOT.0000000000000614
Apard T, Bigorre N, Cronier P, Duteille F, Bizot P, Massin P (2010) Two-stage reconstruction of post-traumatic segmental tibia bone loss with nailing. Orthop Traumatol Surg Res 96:549–553. https://doi.org/10.1016/j.otsr.2010.02.010
Olesen UK, Eckardt H, Bosemark P, Paulsen AW, Dahl B, Hede A (2015) The Masquelet technique of induced membrane for healing of bone defects. A review of 8 cases. Injury 46:S44–S47. https://doi.org/10.1016/S0020-1383(15)30054-1
Giannoudis PV, Harwood PJ, Tosounidis T, Kanakaris NK (2016) Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury 47:S53–S61. https://doi.org/10.1016/S0020-1383(16)30840-3
Morris R, Hossain M, Evans A, Pallister I (2017) Induced membrane technique for treating tibial defects gives mixed results. Bone Joint J 99:680–685. https://doi.org/10.1302/0301-620X.99B5.BJJ-2016-0694.R2
Mühlhäusser J, Winkler J, Babst R, Beeres FJP (2017) Infected tibia defect fractures treated with the Masquelet technique. Medicine 96:1–7. https://doi.org/10.1097/MD.0000000000006948
Ronga M, Ferraro S, Fagetti A, Cherubino M, Valdatta L, Cherubino P (2014) Masquelet technique for the treatment of a severe acute tibial bone loss. Injury 45:S111–S115. https://doi.org/10.1016/j.injury.2014.10.033
Taylor BC, Hancock J, Zitzke R, Castaneda J (2015) Treatment of bone loss with the induced membrane technique. J Orthop Trauma 29:554–557. https://doi.org/10.1097/BOT.0000000000000338
Morelli I, Drago L, George DA, Gallazzi E, Scarponi S, Romanò CL (2016) Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury 47:68–76. https://doi.org/10.1016/S0020-1383(16)30842-7
Masquelet AC, Begue T (2010) The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 41:27–37. https://doi.org/10.1016/j.ocl.2009.07.011
Lasanianos NG, Kanakaris NK, Giannoudis PV (2010) Current management of long bone large segmental defects. Orthop Trauma 24(2):149–163. https://doi.org/10.1016/j.mporth.2009.10.003
Aurégan JC, Bégué T (2014) Induced membrane for treatment of critical sized bone defect: a review of experimental and clinical experiences. Int Orthop 38:1971–1978. https://doi.org/10.1007/s00264-014-2422-y
Masquelet AC (2017) Induced membrane technique: pearls and pitfalls. J Orthop Trauma 31(Suppl 5):S36–S38. https://doi.org/10.1097/BOT.0000000000000979
Metsemakers WJ, Onsea J, Neutjens E, Steffens E, Schuermans A, McNally M, Nijs S (2018) Prevention of fracture-related infection: a multidisciplinary care package. Int Orthop 41(12):2457–2469. https://doi.org/10.1007/s00264-017-3607-y
Rousset M, Walle M, Cambou L, Mansour M, Samba A, Pereira B, Ghanem I, Canavese F (2018) Chronic infection and infected non-union of the long bones in paediatric patients: preliminary results of bone versus beta-tricalcium phosphate grafting after induced membrane formation. Int Orthop 42(2):385–396. https://doi.org/10.1007/s00264-017-3693-x
Sasaki G, Watanabe Y, Miyamoto W, Yasui Y, Morimoto S, Kawano H (2018) Induced membrane technique using beta-tricalcium phosphate for reconstruction of femoral and tibial segmental bone loss due to infection: technical tips and preliminary clinical results. Int Orthop 42(1):17–24. https://doi.org/10.1007/s00264-017-3503-5
Ronga M, Fagetti A, Canton G, Paiusco E, Surace MF, Cherubino P (2013) Clinical applications of growth factors in bone injuries: experience with BMPs. Injury 44:S34–S39. https://doi.org/10.1016/S0020-1383(13)70008-1
Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV (2011) Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury 42:S3–S15. https://doi.org/10.1016/j.injury.2011.06.015
Li D, Hu Q, Kang P, Yang J, Zhou Z, Shen B, Pei F (2018) Reconstructed the bone stock after femoral bone loss in Vancouver B3 periprosthetic femoral fractures using cortical strut allograft and impacted cancellous allograft. Int Orthop. https://doi.org/10.1007/s00264-018-3997-5
Giannoudis PV, Einhorn TA, Marsh D (2007) Fracture healing: the diamond concept. Injury 38(Suppl):S3–S6
Dumic-Cule I, Pecina M, Jelic M, Jankolija M, Popek I, Grgurevic L, Vukicevic S (2015) Biological aspects of segmental bone defects management. Int Orthop 39:1005–1011. https://doi.org/10.1007/s00264-015-2728-4
Govender S, Csimma C, Genant HK et al (2002) Recombinant human bone morphogenetic protein-2 for treatment of open tibial fractures: a prospective, controlled, randomized study of four hundred and fifty patients. J Bone Joint Surg Am 84-A(12):2123–2134
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ronga, M., Cherubino, M., Corona, K. et al. Induced membrane technique for the treatment of severe acute tibial bone loss: preliminary experience at medium-term follow-up. International Orthopaedics (SICOT) 43, 209–215 (2019). https://doi.org/10.1007/s00264-018-4164-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4164-8