Abstract
Background
The ideal treatment of acute anterior shoulder dislocation remains one of the topics that spark debate over the value of primary repair for the first-time anterior shoulder dislocation. The high rate of complications especially in young adults, such as recurrent instability, residual pain, and inability to return to sports, has led to the quest for an ideal management of such injuries.
Objective
In this meta-analysis, we compare between the immediate arthroscopic repair and conservative treatment of primary anterior shoulder dislocation as well as arthroscopic reconstruction of recurrent anterior shoulder dislocation. Outcome measures were failure rate (dislocation, subluxation, and instability) and revision rates.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we searched several database including PubMed, MEDLINE, EMBASE, Web of Science, Cochrane Library, and ClinicalTrials.gov through August 2017 to identify observational and experimental randomized controlled trials comparing the outcomes of immediate arthroscopic repair and conservative treatment of primary shoulder dislocations as well as arthroscopic reconstruction of recurrent dislocation. The primary outcome was failure rate, whereas, secondary outcomes were revision rate and functional outcomes.
Results
Out of the 710 studies identified, 12 were eligible for meta-analysis. The estimated pooled failure rate was 13.7% (7.7%–19.6%), whereas, the pooled revision rate was 7.1% (3.8%–10.4%) in immediate arthroscopic repair of primary shoulder dislocation. The odd ratio (OR) of failure and revision rates were significantly lower in arthroscopic repair of primary shoulder dislocation compared to conservative treatment (OR 0.103, 95% CI [0.052, 0.201]), (OR 0.217, 95% CI [0.078, 0.607]), respectively. The odd ratio (OD) of failure and revision rates were lower in arthroscopic repair of primary shoulder dislocation compared to arthroscopic reconstruction of the recurrent shoulder dislocation; however, the difference was statistically insignificant (OR 0.423, 95% CI [0.117, 1.522]) and (OR 0.358, 95% CI [0.044, 2.920]) respectively.
Conclusion
The outcome of immediate arthroscopic repair of primary anterior shoulder dislocation is superior and encouraging with significant reduction in failure and revision rates compared to conservative treatment. Nevertheless, the failure and revision rates are statistically insignificant compared to arthroscopic reconstruction of recurrent dislocation. Hence, there is evidence to support immediate arthroscopic repair option for primary anterior shoulder dislocations over conservative treatment in young active patients, in order to reduce the risk of failure and revision rates. However, the evidence is inconclusive compared to arthroscopic reconstruction of recurrent dislocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute anterior dislocation of the shoulder joint is a relatively common injury with an estimated lifetime incidence of 2% in the general population [1,2,3]. The shoulder is a complex joint where stability has been sacrificed in favour of range of motion and makes the joint most liable for dislocation following the injury of the anterior labrum which is the main stabilizer of the glenohumeral joint [2, 4]. Failure of the healing of labral tear in conservatively treated shoulder dislocation might explain the high recurrence rate up to 75% in some studies [5]. The risk is especially high in young athletic individuals with variable rates of return to sports [2, 4,5,6,7].
There is relatively high rate of complications associated with shoulder dislocation such as pain, recurrent instability, compromise of quality of life, and ability to return to sports. This is evident in patients treated conservatively with immobilization and rehabilitation. However, these complications also occurred with surgical repair of recurrent dislocations [5, 8,9,10].
The unsatisfactory outcomes of non-surgical management and less than optimal outcomes of surgical repair of recurrent dislocation have led to the quest for an optimal strategy of management of such injuries [11,12,13,14,15,16]. Many authors have proposed early arthroscopic Bankart repair of acute shoulder dislocations with reported significant improvement of functional outcomes [17,18,19]. They also reported decreased dislocation and instability rates in 75 and 84%, respectively [20]. Others reported decreased rates of medium term osteoarthritis [7].
This systematic review and meta-analysis aims to present the evidence-based failure and revision rates of immediate arthroscopic repair of primary anterior shoulder dislocation in comparison to conservative management and arthroscopic repair of recurrent dislocation.
Methods
This meta-analysis was conducted with guidance of the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement.
Literature search strategy
PubMed, MEDLINE, EMBASE, Web of Science, Cochrane Library, and ClinicalTrials.gov were searched up to August 2017 using the following key words with their synonyms: “Shoulder dislocation” AND “glenohumeral instability” AND “recurrent shoulder dislocation “AND “shoulder instability” AND “Bankart lesion” AND “surgical repair” AND “conservative treatment” AND “randomised controlled trial”. Additionally, the reference lists for previous meta-analyses, systemic reviews, and review articles were searched manually in orthopedics and sport journals (Arthroscopy, Journal of Shoulder and Elbow Surgery, American Journal of Sport Medicine, British Journal of Sport Medicine, Journal of Bone and Joint Surgery) to find eligible studies.
Eligibility criteria
The studies were reviewed by two authors (M.A. and A.K.) independently. The inclusion criteria for selection was (1) subjects were 14 years or older and sustained shoulder dislocation either as first time (primary) or recurrent; (2) the intervention was done through the arthroscopic approach, (3) the studies reporting at least one of the following outcome measures: (failure rate, revision rate, or functional outcome); and (4) patients were followed up at least one year after surgery.
Non-comparative studies were included as the primary outcome is a failure rate of arthroscopic approach as one arm meta-analysis.
Exclusion criteria was as the following: studies with patients less than 14 years old; studies reporting maximum follow-up less than one year; studies not reporting the outcomes of interest; open methods of treatment and inability to access the full text.
The eligible studies were selected according to the inclusion and exclusion criteria. Any conflict between the two authors on whether a study is eligible was resolved by the senior author (G.A.).
The primary outcome was failure rate, whereas, the secondary outcomes were (1) revision rate and (2) functional outcomes.
Risk of Bias assessment
Using the “Checklist for Measuring Quality” (Downs and Black, 1998), two independent co-authors assessed the quality and bias of the publications. The “Checklist for Measuring Quality” is discussed in a three-page article and contains 27 “yes”-or-“no” questions across five sections. The tool is easy to use and provides both an overall score for study quality and a numeric score out of a possible 30 points. The five sections include questions about (1) study quality, (2) external validity (3 items), (3) study bias (7 items), (4) confounding and selection bias (6 items), and (5) power of the study (1 items).
Data collection
Data collection process and data items: The data within selected studies were extracted independently by two authors (M.A. and A.K.). Any conflict between the two authors was resolved by the senior author (G.A.).
We extracted the following data:
-
The characteristics of the studies (name, year, level of evidence, follow-up)
-
Subject characteristics (sample size, age, male/female ratio)
-
Disease characteristics
-
Surgical characteristics
-
Primary and secondary outcome parameters as mentioned in the inclusion criteria.
Data analysis
The data analysis was done by open meta-analysis software using the random-effect model and SPSS 22. The researcher determined the mean difference or standardized mean difference and 95% confidence intervals for continuous variables, while for dichotomous data analysis was conducted using the odds ratio and 95% confidence interval. Statistical heterogeneity across the studies was tested using I2, and the level of evidence was assessed according to the Cochrane Back Review Group.
Results
Study selection
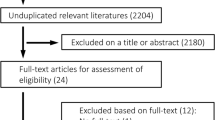
The result of our initial databases search identified 935 articles. Seven hundred ten articles that did not fit our search selection criteria were excluded by title and reading the abstracts. Two hundred twenty-five full-text articles were reviewed with 212 articles being excluded due to the absence of reported outcomes, thus we had a final number 12 articles meet the inclusion criteria and included in quantitative analysis (Fig. 1). The characteristics of the included articles are reported in Table 1.
Twelve studies were included in the meta-analysis with a total of 799 shoulders, 518 in the primary dislocation group, 121 in the recurrent dislocation group, and 165 in the conservative group. The average age was 21.3 years, with 404 males and 54 females. The mean follow-up was 39.2 months.
Study characteristics and risk of bias assessment
Meta-analysis results
Twelve studies reported the failure rate of arthrosc opic repair of primary shoulder dislocation, with the estimated pooled failure rate of 13.7% (7.7%–19.6%) Fig. 2. Ten studies reported the revision rate of arthroscopic repair of primary shoulder dislocation with the estimated pooled revision rate of 7.1% (3.8%–10.4%) Fig. 3.
Two studies compared the failure and revision rates between the arthroscopic repair of primary and recurrent shoulder dislocation. The failure rate was less in primary dislocation repair compared to the recurrent dislocation repair, however the difference was statistically insignificant (OR 0.423, 95% CI [0.117, 1.522]) and the same for the revision rate (OR 0.358, 95% CI [0.044, 2.920]) Fig. 4.
Six studies compared the failure rate between the arthroscopic repair of primary shoulder dislocation and conservative management. The failure rate was significantly less in arthroscopic group (OR 0.103, 95% CI [0.052, 0.201], whereas, only four studies compared the revision rate between the arthroscopic repair and conservative treatment of primary shoulder dislocation, with less revision rate in arthroscopic repair group (OR 0.217, 95% CI [0.078, 0.607]) Fig. 5.
We were unable to report the difference in functional outcome of arthroscopic repair of primary shoulder dislocation because of using different functional outcome score in the included studies.
Discussion
At the time of writing this meta-analysis manuscript, 12 articles reported the failure rate of primary arthroscopic repair and ten articles reported the revision rate. The failure rate was the highest in Chapus et al. [7] and lowest in Kim et al. [21]. The mean pooled failure rate was 13.7% (range 7.7–19.6%). More detailed discussion is necessary to understand the factors that might have caused this variability of reported outcomes. However, most of the patients in these 12 studies had satisfactory outcomes. Most of the studies reported a significant superiority of primary arthroscopic repair to conservative management.
Chapus et al. conducted a prospective study that included 21 patients who were under the age of 25 years with anterior shoulder dislocation. Five patients sustained recurrence and two had sense of instability due to seven failed surgeries (35%). Except for one patient; violent trauma, epilepsy, or premature return to sport was associated with failure. Moreover, the rate of osteoarthritis was 15% and recurrence did not correlate with shoulder osteoarthritis.
Two articles studied primary arthroscopic repair in adolescents. Nixon et al. [22] retrospectively reviewed 61 shoulders in 57 adolescents who underwent primary arthroscopic shoulder stabilization for labral tears. The mean age of their patients was 16.8 years (13–18). They reported a recurrent dislocation rate in 19 (31%) shoulders. They concluded that adolescents are at high risk for recurrence following arthroscopic stabilization and the patients should be counseled regarding this complication. They also concluded that sex, type of sport, hyper-laxity, and tear morphology were not significantly related to recurrence.
Another article that studied adolescents was done by Gigis et al. [23]. They conducted a prospective study comparing the arthroscopic repair and conservative management of first-time shoulder dislocation in patients 15–18 years of age. Five patients (13.1%) suffered recurrent instability in arthroscopic repair group compared to the 70% of recurrence in the conservative group. The authors attributed the high rate of recurrence in conservatively managed group to immobilization in internal rotation rather than external rotation.
A lower recurrence rate was reported by Law et al. [24] in a retrospective series of 38 young patients with mean age of 21 years who had immediate Bankart arthroscopic repair within one month (6–25 days) of first anterior shoulder dislocation. There were two cases of post-traumatic re-dislocation (5.2%), both were due to forceful hyper-abduction movement. The first case had apprehension while playing contact sport with recurrence at one year with 20% glenoid bone loss and refused revision surgery. The other re-dislocation occurred at two years due to misplacement of anchor on the glenoid and was revised.
Kirkley et al. [2] did compare arthroscopic stabilization and conservative management in first-time shoulder dislocation in skeletally mature young adults. They conducted a single blinded randomized clinical trial on 40 patients, 20 in each group. Outcomes were reported an average follow-up of 32 months. They reported a recurrence rate of 15.9 and 47% in arthroscopic repair and conservative groups, respectively. All of the three patients who had re-dislocation in the arthroscopic repair group have not opted for further surgery. All had experienced instability during sports activities followed by dislocation later. Two patients in the arthroscopic group developed instability. One went for open capsular shift procedure while the other had normal arthroscopic evaluation with no further procedure was done. On the other hand, seven out of the 19 patients treated conservatively had a Bankart repair at a later stage.
Kirkley et al. [4] recontacted the subjects of their previous study to report long-term outcomes at an average follow-up of 79 months. Seventy-seven percent of the original subjects returned Western Ontario Shoulder Instability Index (WOSI), American Shoulder and Elbow Surgeons (ASES), and Disabilities of the Arm, Shoulder and Hand (DASH) questionnaires. Interestingly, the difference in WOSI score in the initial study has lessened to become statistically insignificant. Differences in all other scores were statistically insignificant in long term. There have been no additional recurrences of dislocation in either group. Argument can be made that immediate repair does not provide long-term functional outcomes improvement over conservative management and immediate repair of first-time anterior dislocation should be tailored to specific patient population.
Another randomized clinical trial was conducted by Bottoni et al. [5] comparing primary repair of anterior shoulder dislocation with conservative management in active military personnel. Failure rate in the conservative group reached 75% compared to 11.1% in the arthroscopy group. Those who failed ended up with open Bankart reconstruction. SANE and L’Insalata functional scores were used and showed statistically significant superiority of arthrocopic reconstruction to conservative management. Range of motion was similar in both groups.
An earlier study on active military personnel was done by Arceiro et al. [6]. They prospectively compared arthroscopic stabilization to conservative management of acute shoulder dislocation. They reported 14% failure rate in arthroscopy group compared to 80% in conservative treatment group. One limitation of this study that most of the patients who choose conservative management were involved in more traumatic sports activities compared to those who choose arthroscopic repair. Moreover, there was no randomization of treatment groups due to the investigational nature of arthroscopic repair technique at that time.
Both studies on military personnel have a limitation that their subjects are highly trained athletes with high-demand activities that could not be adjusted.
Larrain et al. [25] conducted prospective comparative study on 46 patients; most injuries were rugby related with the average age was 21 years. Eighteen were treated nonoperatively while 28 patients underwent primary arthroscopic repair; 22 patients using trans-glenoid suture and 6 with bone anchor suture fixation. Interestingly, they reported an extreme difference in favor of arthroscopic repair over non-operative management with the highest rate of re-dislocation after conservative management (94.5%) compared to (4%) in arthroscopic repair group among all studies.
Robinson et al. [20] conducted a comprehensive double-blinded randomized controlled clinical trial with 42 patients in each group, all under the age of 35 years and comparing primary arthroscopic Bankart repair and arthroscopic lavage alone. They sought to find out if the favorable outcomes of surgery were due to stabilization of the shoulder or can be attributed to joint lavage. They demonstrated 82% reduction of instability and 76% reduction of dislocation in the arthroscopic Bankart repair group.
Primary versus recurrent dislocation
At the time of writing this manuscript, there are only two published studies that compared the outcomes of arthroscopic repair of primary anterior shoulder dislocation and arthroscopic reconstruction of recurrent shoulder dislocation. Both concluded superior outcomes of arthroscopic Bankart repair of primary anterior shoulder dislocation.
Marshal et al. [19] performed a retrospective chart review with follow-up survey on 173 patients at eight different facilities. They compared the outcomes of those who underwent arthroscopic repair for primary anterior shoulder dislocation and those for recurrent dislocation. The mean age was 19.2 ± 3.9 years. They reported that the odds of having post-operative instability were four times higher for patients with recurrent dislocation compared to those with primary anterior shoulder dislocation. Moreover, the odds of needing additional surgery were six times higher in the recurrent dislocation group compared to primary anterior shoulder dislocation group. The number of anchors, smoking status of the patient, age, and sex did not affect the rate of instability or need for revision. They concluded that young patients should be offered surgical repair after their first episode of dislocation.
Their study had substantial limitations that have addressed by the authors. It was a retrospective study with only 70% follow-up with the performance bias in surgical technique across the eight participating facilities might be a concern. Moreover, the charts reviewed the patients from 2003 to 2013 and with advances in arthroscopic technique over the last ten years might have affected the study results.
Kim et al. [21] also compared outcomes of repair of first-time dislocations to those with recurrent dislocation. Their study included 110 subjects, 42 in primary group and 68 in recurrent group. They failed to demonstrate any statistical difference in the instability and recurrence of dislocation rates between the two groups. One drawback of this study is that only the SLAP type V lesions were included. It is unclear if their finding can be generalized to other types of lesions.
From those two studies, it can be concluded that primary repair has similar or superior outcomes compared to recurrent dislocation repair. In our meta-analysis, the failure and revision rates were less in primary dislocation repair compared to the recurrent dislocation repair. However, the difference was statistically insignificant.
Arthroscopic versus conservative management of primary shoulder dislocation
Six studies compared the outcomes of arthroscopic and conservative management of primary anterior shoulder dislocations. All studies reported statistically significant difference of failure rate in the favour of arthroscopic repair. Three of studies also reported the revision rate, however, only Robinson et al. [20] reported a statistically significant difference of revision rate in the favour of arthroscopic repair.
Revision rate of primary repair was reported in 10 studies. The highest revision rate was reported by Kirkely et al. and lowest reported by Law et al. and Kim et al. It is worth mentioning that many patients who suffered from failed surgery have refused surgery and had a favourable outcome. This explains the different rates of failure and revisions. A common mechanism of failure was related to violent sport trauma, young age, and technical errors. Failures were treated in various ways including revision of fixation, coracoid bone block, Latarjet procedure (8) and conservative option in many occasions.
In our meta-analysis, both the failure and revision rates were less in the arthroscopic repair of primary dislocation compared to the conservative treatment of primary shoulder dislocation failure and revision rates reduction were statistically significant.
Limitations
Despite the authors’ best efforts, a few limitations exist to conclusions of this meta-analysis. First, functional outcomes comparative conclusions could not be drawn due to the variability of outcome measures used by different studies. However, most of the studies demonstrated superiority of arthroscopic repair of primary anterior shoulder dislocation to conservative management.
Another limitation is the different follow-up lengths among studies. Longer follow-up could possibly change the outcomes as evident in Kirkely.
Finally, and importantly, there are only two studies comparing primary versus recurrent shoulder dislocation arthroscopic repair and only Marshal et al. demonstrated a statistically significant difference in favour of primary repair. Moreover, the latter was a retrospective chart review with substantial limitations discussed previously. With the later limitation in mind, the authors recognize that this meta-analysis did not arrive at a solid conclusion to justify the repair of primary dislocation rather than waiting for recurrent dislocation to occur. This is attributed to the paucity of comparative studies in the literature and hence the question which intervention is superior remains unanswered.
Conclusion
The outcome of immediate arthroscopic repair of primary anterior shoulder dislocation is superior and encouraging with significant reduction in failure and revision rates compared to conservative treatment. Nevertheless, the failure and revision rates are statistically insignificant compared to arthroscopic reconstruction of recurrent dislocation. Hence, there is some evidence to support immediate arthroscopic repair option for primary anterior shoulder dislocations compared to conservative treatment in young active patients, in order to reduce the risk of failure and revision rates but there is inconclusive evidence compared to arthroscopic reconstruction of recurrent dislocation.
References
Hovelius L (1982) Incidence of shoulder dislocation in Sweden. Clin Orthop Relat Res 127–131
Kirkley A, Griffin S, Richards C et al (1999) Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy 15:507–514. https://doi.org/10.1053/ar.1999.v15.015050
Owens BD, Duffey ML, Nelson BJ et al (2007) The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 35:1168–1173. https://doi.org/10.1177/0363546506295179
Kirkley A, Werstine R, Ratjek A, Griffin S (2005) Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy 21:55–63. https://doi.org/10.1016/j.arthro.2004.09.018
Bottoni CR, Wilckens JH, DeBerardino TM et al (2002) A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med 30:576–580. https://doi.org/10.1177/03635465020300041801
Arciero RA, Wheeler JH, Ryan JB, McBride JT (1994) Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med 22:589–594. https://doi.org/10.1177/036354659402200504
Chapus V, Rochcongar G, Pineau V et al (2015) Ten-year follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocation in young patients. Orthop Traumatol Surg Res 101:889–893. https://doi.org/10.1016/j.otsr.2015.09.029
Hovelius L, Saeboe M (2009) Neer Award 2008: Arthropathy after primary anterior shoulder dislocation--223 shoulders prospectively followed up for twenty-five years. J Shoulder Elb Surg 18:339–347. https://doi.org/10.1016/j.jse.2008.11.004
Hovelius L, Olofsson A, Sandström B et al (2008) Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. a prospective twenty-five-year follow-up. J Bone Joint Surg Am 90:945–952. https://doi.org/10.2106/JBJS.G.00070
Rowe CR (1956) Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 38–A:957–977
Kordasiewicz B, Małachowski K, Kicinski M et al (2017) Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)-clinical results at short term follow-up. Int Orthop 41:1023–1033. https://doi.org/10.1007/s00264-016-3372-3
Itoi E, Hatakeyama Y, Sato T et al (2007) Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence: a randomized controlled trial. J Bone Joint Surg Am 89:2124–2131. https://doi.org/10.2106/JBJS.F.00654
Porcellini G, Campi F, Pegreffi F et al (2009) Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am 91:2537–2542. https://doi.org/10.2106/JBJS.H.01126
Dickens JF, Owens BD, Cameron KL et al (2014) Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med 42:2842–2850. https://doi.org/10.1177/0363546514553181
Longo UG, van der Linde JA, Loppini M et al (2016) Surgical versus nonoperative treatment in patients up to 18 years old with traumatic shoulder instability: a systematic review and quantitative synthesis of the literature. Arthroscopy 32:944–952. https://doi.org/10.1016/j.arthro.2015.10.020
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging. Hill-Sachs lesion Arthroscopy 16:677–694
Rhee YG, Ha JH, Cho NS (2006) Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med 34:979–985. https://doi.org/10.1177/0363546505283267
Lenters TR, Franta AK, Wolf FM et al (2007) Arthroscopic compared with open repairs for recurrent anterior shoulder instability A systematic review and meta-analysis of the literature. J Bone Joint Surg Am 89:244–254. https://doi.org/10.2106/JBJS.E.01139
Marshall T, Vega J, Siqueira M et al (2017) Outcomes after arthroscopic Bankart repair: patients with first-time versus recurrent dislocations. Am J Sports Med 45:1776–1782. https://doi.org/10.1177/0363546517698692
Robinson CM, Jenkins PJ, White TO et al (2008) Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, double-blind trial. J Bone Joint Surg Am 90:708–721. https://doi.org/10.2106/JBJS.G.00679
Kim D-S, Yi C-H, Yoon Y-S (2011) Arthroscopic repair for combined Bankart and superior labral anterior posterior lesions: a comparative study between primary and recurrent anterior dislocation in the shoulder. Int Orthop 35:1187–1195. https://doi.org/10.1007/s00264-011-1229-3
Nixon MF, Keenan O, Funk L (2015) High recurrence of instability in adolescents playing contact sports after arthroscopic shoulder stabilization. J Pediatr Orthop B 24:173–177. https://doi.org/10.1097/BPB.0000000000000135
Gigis I, Heikenfeld R, Kapinas A et al (2014) Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Pediatr Orthop 34:421–425. https://doi.org/10.1097/BPO.0000000000000108
Law BK-Y, Yung PS-H, Ho EP-Y et al (2008) The surgical outcome of immediate arthroscopic Bankart repair for first time anterior shoulder dislocation in young active patients. Knee Surg Sports Traumatol Arthrosc 16:188–193. https://doi.org/10.1007/s00167-007-0453-2
Larrain MV, Botto GJ, Montenegro HJ, Mauas DM (2001) Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy 17:373–377
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Adam, M., Attia, A.K., Alhammoud, A. et al. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: systematic review and meta-analysis. International Orthopaedics (SICOT) 42, 2413–2422 (2018). https://doi.org/10.1007/s00264-018-4046-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4046-0