Abstract
Purpose
Glenoid loosening after total shoulder arthroplasty (TSA) is influenced by the position of the glenoid component. 3D planning software and patient-specific guides seem to improve positioning accuracy, but their respective individual application and role are yet to be defined. The aim of this study was to evaluate the accuracy of freehand implantation after 3D pre-operative planning and to compare its accuracy to that of a targeting guide.
Method
Seventeen patients scheduled for TSA for primary glenohumeral arthritis were enrolled in this prospective study. Every patient had pre-operative planning, based on a CT scan. Glenoid component implantation was performed freehand, guided by 3D views displayed in the operating room. The position of the glenoid component was determined by manual segmentation of post-operative CT scans and compared to the planned position. The results were compared to those obtained in a previous work with the use of a patient-specific guide.
Results
The mean error for the central point was 2.89 mm (SD ± 1.36) with the freehand method versus 2.1 mm (SD ± 0.86) with use of a targeting guide (p = 0.05). The observed difference was more significant (p = 0.03) for more severely retroverted glenoids (> 10°). The mean errors for version and inclination were respectively 4.82° (SD ± 3.12) and 4.2° (SD ± 2.14) with freehand method, compared to 4.87° (SD ± 3.61) and 4.39° (SD ± 3.36) with a targeting guide (p = 0.97 and 0.85, respectively).
Conclusion
3D pre-operative planning allowed accurate glenoid component positioning with a freehand method. Compared to the freehand method, patient-specific guides slightly improved the position of the central point, especially for severely retroverted glenoids, but not the orientation of the component.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total shoulder arthroplasty is the preferred treatment for glenohumeral primary osteoarthritis, with good short- and long-term functional results [1, 2]. Despite these reliable outcomes, glenoid loosening has been reported to be a serious concern. Though exceptional prior five years post-operative, radiographic loosening approximates 50% at ten years follow-up [2, 3]. Improving glenoid implant survivorship over time is one of the more crucial elements of research relating to shoulder arthroplasty [4]. Over the past ten years, much attention has been paid to improve the accuracy of glenoid implant positioning. The shoulder is a highly mobile joint, and stability of this joint is a delicate combination of multiple factors, including bone orientation, ligamentous restrains, and peri-articular muscle balance. With respect to shoulder arthroplasty, malpositioning of the implant, defined by excessive retroversion or inclination (over 10°), may be responsible for increased shear forces and higher loosening rate after years [4,5,6,7,8,9]. Moreover, reported surgeon’s accuracy for glenoid implant positioning is relatively poor, mostly because of lack of pre-operative planning and difficulty with intra-operative landmarks [10,11,12,13,14,15].
Ideal component positioning requires determining precisely the optimal position of the implant for each patient. This equates to minimal retroversion and inclination, as well as minimal bone reaming in order to preserve subchondral bone and provide sufficient implant-on-bone seating [4,5,6,7,8,9]. Glenosys planning software (Imascap, Plouzané, France) allows fast automatic 3D modeling of the scapula, reliable 3D measurements of scapular parameters, and virtual implantation of the glenoid component prior to surgery, compatible with the surgeon’s routine practice [16, 17]. Recently, patient-specific guides (PSG) have been proposed to aim and recreate the planned position intra-operatively. Several of these systems, based on 3D imaging and 3D printing, are currently utilized with promising results, but what is not clear are the respective benefits of each component of this process, that is, the pre-operative planning and then the utility of the specific targeting guides [10, 11, 13, 15,16,17,18,19].
Our hypothesis was that pre-operative planning, even without PSG, could optimize glenoid component positioning. The aim of this study was to evaluate the accuracy of glenoid implant position after isolated 3D pre-operative planning with Glenosys Software (Imascap, Plouzané, France) using a freehand implantation method. Secondarily, we compared our results to those obtained in another published series, using the same software, but with the use of a PSG for glenoid implantation and thus evaluated the proper role of this device in improving the surgeon’s accuracy.
Patient and method
Population
Seventeen patients, scheduled for a total shoulder arthroplasty (TSA) for primary glenohumeral osteoarthritis, were enrolled in this prospective, single centre study between April 2014 and October 2015. All the patients had a pre-operative CT scan of the entire shoulder (including medial border and inferior angle of the scapula), performed in the supine position, with the arm at side and with the shoulder in neutral rotation, with specific acquisition parameters (Fig. 1). The native DICOM axial views were used for pre-operative planning with Glenosys Software (Imascap, Plouzané, France). There were 14 women and three men, with mean age of 68 ± 12 years (range 48–87). All the subjects were provided clear information and gave written consent for a post-operative CT scan, before inclusion. This study received an Institutional Review Board agreement (Centre Orthopédique Santy, IRB 20.1611).
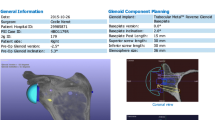
Pre-operative planning
Using specific validated algorithms, Glenosys Software performs automatic 3D reconstruction of the scapula and precisely determines glenoid version, inclination, and humeral head subluxation, with respect to the scapular plane [20, 21]. This software was used by the surgeons to analyze glenoid deformity and to virtually implant the glenoid component for each patient before surgery. All the pre-operative shoulder parameters (version, inclination, humeral head subluxation, and glenoid type according to Walch classification [22]) were recorded for analysis (Table 1). The surgeon had to choose component size and radius of curvature, as well as the optimal position with respect to orientation (< 10° superior inclination, < 15° retroversion), implant-on-bone seating (min. 80%), subchondral bone preservation, and avoiding glenoid vault perforation, based on previously published data [4,5,6,7,8,9]. The virtual component parameters (type, position, orientation) were created by 3D models saved in a Standard Tessellation Language (.STL) file format, as well as the 3D pre-operative scapula. These two .STL files (“pre-op scapula” and “pre-op implant”) were subsequently used for comparison with post-operative real position of the implant.
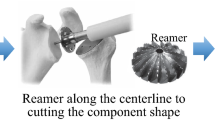
Surgical technique
All the procedures were performed in one centre, by two surgeons with significant experience level in shoulder arthroplasty (AJ, DM). Planning parameters and 3D views of the scapula, the implant, and the virtual guidewire were printed and displayed in the operating room (Fig. 2). For all the patients, the humeral implant was an ASCEND FLEX short uncemented stem (Tornier SAS, Montbonnot Saint Martin, France) and glenoid component was a PerFORM polyethylene keeled cemented component (Tornier SAS, Montbonnot Saint Martin, France). After residual cartilage removal, guidewire positioning and reaming were performed freehand, based on planning parameters and displayed 3D views, without any specific guide. Then, glenoid preparation was performed using a standard compacted autograft technique [23] and low viscosity cement.
3D segmentation
A CT scan was performed within two months after surgery, with a specific metallic artifact reduction protocol (Fig. 3). Because of metallic components, automatic segmentation was not possible at this step. Axial views were used for manual 3D segmentation of the scapula (Fig. 3) using Amira Software (Visage Imaging, Inc), according to a previously validated technique (Thesis, Jean Chaoui PhD, unpublished work). The two metallic markers inside the glenoid component were also segmented in a different file (Fig. 3). Thus, 2 .STL files (“post-op scapula” and “metallic markers”) were obtained for each patient, recreating the post-operative scapula and the position of the implanted glenoid component.
Manual 3D segmentation steps. a Standard post-operative CT scan with metallic artifact reduction protocol. b Manual contouring of the scapular body on every slice. c 3D segmentation. d Segmentation of the metallic markers/superposition of a 3D implant model/control of the position of the markers on 2D CT scan slices
Matching and comparison
As the “pre-op scapula” and the “post-op scapula” were not in the same position within the 3D space, manual 3D matching between them had to be performed (Fig. 4). The matching procedure was done with Amira software, by moving “post-op scapula” 3D model onto the “pre-op scapula.” The precision of this overlapping was evaluated by the mean distance between each corresponding points of the two scapulae, which was on average 0.4 ± 0.1 mm (range 0.3–0.6) for the entire series. The same translation matrix was then applied to the “metallic markers” 3D model. Then, a standard 3D model of Perform glenoid component (“post-op implant”) was matched on these metallic markers. The two 3D components (“pre-op implant” and “post-op implant”) were then in the same 3D referential and could be compared, regarding position and orientation.
Matching protocol. a “Pre-op scapula” (blue) and “post-op scapula”/“markers” (red and yellow) were not natively in the same 3D referential. b Superimposition of “post-op scapula” (red) onto “pre-op scapula” (blue). c The same translation matrix was applied to the metallic markers (yellow). d Superimposition of the 3D implant model onto the metallic markers in the new referential. e Final view of “post-op implant” (green) in the new referential, which can be compared to the planned “pre-op implant”
For each patient, implanted component (“post-op implant”) was compared to planned component (“pre-op implant”) using specific software (Imascap, Plouzané, France), delivering absolute errors for 3D position of the central point of the implant (“3D offset”, expressed in millimeters), version (degrees), inclination (degrees), and rotation/rolling (degrees). Offsets represented the distance (millimeters) between the theoretical planned position and the real position of the implanted component. The “3D offset” was derived from anteroposterior offset and superoinferior offset in the sagittal plane, and mediolateral offset in the axial plane, which were analyzed separately. Malposition criteria, according to Throckmorton et al. [15], corresponded to a 3D offset > 4 mm or a > 10° error for version or inclination.
Comparison with a published series using PSG
Finally, all the values of the freehand study were compared to those obtained in a previous published series of 17 patients, using the same protocol but with the use of a polyamide 3D-printed patient-specific guide, for glenoid component implantation [17]. The two series were comparable for the demographic data (age and sex) and for the characteristics of the pre-operative glenoids (Table 1).
Statistical analysis
Statistical analysis was performed with MedCalc Statistical Software (MedCalc Software bvba, Ostend, Belgium). A Student’s t test was used to compare the quantitative data (3D offset, version, inclination) between our “freehand” series and the series of Gauci et al. with PSG [17]. A chi-square test was used for qualitative values or a Fisher exact test utilized when the population of the subgroups was < 5. A p value < 0.05 was considered significant.
Results
All the pre-operative measurements are shown in Table 1. In our series, there were seven type A and ten type B glenoids (Walch classification).
In our series (Table 2), the mean error for 3D position of the central point of the glenoid component was 2.9 ± 1.4 mm (1.2–4.8). The mean errors for version and inclination were respectively 4.8° ± 3.1° (0.4–13.3) and 4.2° ± 2.1° (0.7–7.8). Rolling mean error was 8.8° ± 5.8 (1.7–20.1). Seven cases (41%) in our series met the criteria for malposition, according to Throckmorton et al. [15] (> 4 mm or > 10° error), largely because of a 3D offset > 4 mm (six cases).
In the PSG series [17] (Table 2), the accuracy was significantly higher for the 3D position of the central point (2.1 ± 0.9 mm, p = 0.05) but not for version or inclination. Rolling was not reported. Only two cases (12%) were malpositioned (p = 0.11), but no case had a 3D offset greater than 4 mm (p < 0.01). Sagittal and frontal 2D offset for the two series are represented in Fig. 5.
2D offsets (position of the central point) with the two compared methods. a 2D offsets with the freehand method (our series) in the sagittal plane and in the frontal plane. b 2D offsets with the PSG method (Gauci et al. [17]) in the sagittal plane and in the frontal plane
We focused on the influence of pre-operative glenoid deformity on the final position of the glenoid component. Results of this comparative analysis are shown in Table 3. In our series with the freehand technique, the position of the central point was significantly less accurate when pre-operative glenoid version was ≥ 10° (p = 0.04), whereas there was no influence of glenoid deformity in the PSG series. Thus, 3D offset was significantly higher for high deformities (≥ 10°) with freehand technique than with PSG (p = 0.02), whereas there were no differences between the two techniques when pre-operative version was < 10°. Pre-operative glenoid deformity did not influence the mean error of version or inclination in the two series.
Discussion
Pre-operative 3D planning allowed determination of the ideal glenoid component position for each patient and provided 3D landmarks to the surgeon for accurate freehand implant positioning, close to that obtained with patient-specific guides, underlining the importance of 3D planning before any shoulder replacement. The benefit of PSG was clear for complex and severely retroverted glenoids but not for simpler cases (type A, < 10° retroversion).
In our series, the freehand accuracy of the surgeon was ± 2.9 mm for the position of the central point of the implant and between 4° and 5° for version and inclination. Previous published in vitro and in vivo series reported similar results after 3D planning and freehand technique [11, 13, 18]. Similarly to us, in an in vivo study, Iannotti et al. reported a mean deviation of 1.5 to 1.7 mm for 2D offsets (3D offset not reported), 4.1° for inclination, and 4.3° for version [18], using 3D planning and freehand implantation. Some authors evaluated the mean errors committed by surgeons with a standard technique without planning [10, 11, 13,14,15, 18] and reported mean deviations were 3 mm for the central point and 7–11° for version and inclination. But in these studies, the mean errors have been calculated by reference to a constant and theoretical objective of 0° version and 0° inclination, which is not necessarily the ideal position for each patient. To correctly assess the ability of a surgeon to precisely reach freehand the ideal position without 3D planning, a study should include shoulders with TSA implanted freehand without any planning and compare the position of the implanted component to the virtual position obtained in a 3D planning performed after the surgery. But there is no such study published in the literature, and benefit of 3D planning cannot be proven. Our results being close to those obtained with a PSG and visually better than those published without 3D planning (at least for orientation), we may hypothesize that 3D planning is useful for glenoid implantation, especially since the software could be used by the surgeon himself in routine practice, thanks to a validated automatic algorithm for 3D segmentation and measurements [20, 21].
With a mean error of 2.1 mm for the central point, 4.9° for version, and 4.4° for inclination, the use of a PSG showed a significant (but slight) improvement only for the position of the central point, compared to our freehand method. Moreover, this difference was only significant for severely retroverted glenoids (> 10°) but not for simpler cases (< 10°). To our knowledge, only three studies [11, 13, 18] reported comparative accuracy between PSG method and planning/freehand method. Lewis et al. [13], in a study based on polymer models, found a significant improvement with a PSG, with a mean error of 3° for version and 3° for inclination (compared to 8° and 9°, respectively, with a planning/freehand method). Iannotti et al. [11], in a sawbone study, reported similar results with 3.1° mean error for version, 2.8° for inclination, and 1.2 mm for central point (compared to 6.7°, 9.3°, and 2.4 mm, respectively, with a planning/freehand method) and a strongly minimized risk of having a > 5° or > 3 mm error. These studies were not in vivo studies. Iannotti et al. [18] published recently a similar study, involving patients, and their conclusions were different. In their study, PSG did not significantly improve accuracy for version, inclination, or central point, compared to a planning/freehand method (3.1° vs 4.1° mean error for inclination, 4° vs 4.3° for version, 0.9 to 1.1 vs 1.5 to 1.7 mm for 2D offsets). In fact, in vivo conditions imply soft tissue contractures and difficulty of exposure and guide positioning, secondary to humeral head obstruction and glenoid retroversion, that do not exist in sawbone studies and that probably explain the observed differences between these studies.
One possible explanation for the errors could be related to imprecise and/or unstable positioning of the guide on the glenoid. One hypothesis could be that polyamide guides are too smooth and not stable enough on the glenoid rim. A decision has been already undertaken to move towards use of metallic guides, with the expectation of being more stable. Another possible explanation is that PSG only control the position of the guidewire, and slight errors could also be related to the next steps, such as reaming, determining rotation, or cementing the implant, as reported by Nguyen et al. [14]. Walch et al. reported much better accuracy with the same planning software and a PSG, in a sawbone study considering only the position of the guidewire, not the implant, and thus negating all the subsequent steps of implantation and the potential related errors [16]. In order to demonstrate a real superiority of the PSG method over planning/freehand method, optimization of these PSG should be made to improve stability on the glenoid and include control of reaming (orientation and depth) and rotation.
Nevertheless, PSG method was much more reliable than the freehand method, with only 12% glenoid component considered malpositioned (compared to 44% with freehand method). This point is important and can be considered a real potential benefit of the PSG in routine daily practice, as surgeons may not always be as focused on positioning accuracy as we were in the context of a scientific study. Moreover, it has been reported that more than 70% of shoulder prostheses in the USA are performed by low-volume surgeons (< 10 arthroplasty per year) [24], and it is known that the lack of experience strongly influences the quality of implantation and the outcomes of shoulder arthroplasty [11, 24, 25]. In our series, prostheses were only implanted by high-volume surgeons (> 50 arthroplasties per year). This could explain the lack of strong differences between our series and the PSG series. Patient-specific guides may be of real interest for low-volume surgeons, who are not familiar with glenoid implant positioning, but this would also imply a learning curve for 3D pre-operative planning, as well as for the use of the PSG intra-operatively. Finally, the benefit of using a PSG may be clearer for complex and severely retroverted glenoids, regardless of the surgeon’s experience.
Our work has some limitations. The first is the small number of patients that could affect the statistical comparison. Moreover, our series involved consecutive cases of shoulder arthroplasty, and there were 41% of type A non-retroverted glenoids, for which the use of a PSG was not clearly beneficial. Accuracy of our freehand method could have been lower in a series with a higher number of retroverted glenoids.
Determination of the mean errors of positioning was based on a manual process, with successive steps such as scapula segmentation, metallic markers segmentation, and scapula matching, as previously described. Although all these steps have been previously validated, and the precision controlled at each step of the process, slight errors could have affected the final measurements.
Finally, we had no control group with a standard method without pre-operative planning, to prove the superiority of 3D pre-operative planning over a standard method. Another study with standard implantation without 3D planning, followed by a “post-operative” planning as a reference, could be of interest.
Conclusion
3D pre-operative planning seemed to be useful before total shoulder replacement, to determine the optimal position of glenoid component and give 3D views and landmarks to the surgeon to correctly perform the surgery, with a good expected accuracy. The use of a PSG made the positioning a little more precise, and more reliable, especially for complex and severely retroverted glenoids. Our results could limit the actual enthusiasm towards PSG under this current preliminary form, and should lead to optimizations, so that their benefits become clearer. Additionally, long-term studies would be needed to show if a gain of a very few millimeters or degrees is relevant and could seriously affect long-term outcomes of total shoulder arthroplasty.
References
Carter MJ, Mikuls TR, Nayak S et al (2012) Impact of total shoulder arthroplasty on generic and shoulder-specific health-related quality-of-life measures: a systematic literature review and meta-analysis. J Bone Joint Surg Am 94:e127. https://doi.org/10.2106/JBJS.K.00204
Walch G, Young AA, Melis B et al (2011) Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: multicenter study with a follow-up greater than 5 years. J Shoulder Elb Surg 20:385–394. https://doi.org/10.1016/j.jse.2010.07.011
Torchia ME, Cofield RH, Settergren CR (1997) Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elb Surg 6:495–505. https://doi.org/10.1016/S1058-2746(97)90081-1
Walch G, Young AA, Boileau P et al (2012) Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Jt Surg Am 94. https://doi.org/10.2106/JBJS.J.00699
Farron A, Terrier A, Büchler P (2006) Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elb Surg 15:521–526. https://doi.org/10.1016/j.jse.2005.10.003
Hopkins AR, Hansen UN, Amis AA, Emery R (2004) The effects of glenoid component alignment variations on cement mantle stresses in total shoulder arthroplasty. J Shoulder Elb Surg 13:668–675. https://doi.org/10.1016/j.jse.2004.04.008
Iannotti JP, Spencer EE, Winter U et al (2005) Prosthetic positioning in total shoulder arthroplasty. J Shoulder Elb Surg Am Shoulder Elb Surg Al 14:111S–121S. https://doi.org/10.1016/j.jse.2004.09.026
Nyffeler RW, Sheikh R, Atkinson TS et al (2006) Effects of glenoid component version on humeral head displacement and joint reaction forces: an experimental study. J Shoulder Elb Surg Am Shoulder Elb Surg Al 15:625–629. https://doi.org/10.1016/j.jse.2005.09.016
Shapiro TA, McGarry MH, Gupta R et al (2007) Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elb Surg 16:S90–S95. https://doi.org/10.1016/j.jse.2006.07.010
Hendel MD, Bryan JA, Barsoum WK et al (2012) Comparison of patient-specific instruments with standard surgical instruments in determining glenoid component position: a randomized prospective clinical trial. J Bone Joint Surg Am 94:2167–2175. https://doi.org/10.2106/JBJS.K.01209
Iannotti J, Baker J, Rodriguez E et al (2014) Three-dimensional preoperative planning software and a novel information transfer technology improve glenoid component positioning. J Bone Joint Surg Am 96:e71. https://doi.org/10.2106/JBJS.L.01346
Iannotti JP, Greeson C, Downing D et al (2012) Effect of glenoid deformity on glenoid component placement in primary shoulder arthroplasty. J Shoulder Elb Surg Am Shoulder Elb Surg Al 21:48–55. https://doi.org/10.1016/j.jse.2011.02.011
Lewis GS, Stevens NM, Armstrong AD (2015) Testing of a novel pin array guide for accurate three-dimensional glenoid component positioning. J Shoulder Elb Surg Am Shoulder Elb Surg Al 24:1939–1947. https://doi.org/10.1016/j.jse.2015.06.022
Nguyen D, Ferreira LM, Brownhill JR et al (2009) Improved accuracy of computer assisted glenoid implantation in total shoulder arthroplasty: an in-vitro randomized controlled trial. J Shoulder Elb Surg Am Shoulder Elb Surg Al 18:907–914. https://doi.org/10.1016/j.jse.2009.02.022
Throckmorton TW, Gulotta LV, Bonnarens FO et al (2015) Patient-specific targeting guides compared with traditional instrumentation for glenoid component placement in shoulder arthroplasty: a multi-surgeon study in 70 arthritic cadaver specimens. J Shoulder Elb Surg Am Shoulder Elb Surg Al 24:965–971. https://doi.org/10.1016/j.jse.2014.10.013
Walch G, Vezeridis PS, Boileau P et al (2015) Three-dimensional planning and use of patient-specific guides improve glenoid component position: an in vitro study. J Shoulder Elb Surg Am Shoulder Elb Surg Al 24:302–309. https://doi.org/10.1016/j.jse.2014.05.029
Gauci MO, Boileau P, Baba M et al (2016) Patient-specific glenoid guides provide accuracy and reproducibility in total shoulder arthroplasty. Bone Jt J 98-B:1080–1085. https://doi.org/10.1302/0301-620X.98B8.37257
Iannotti JP, Weiner S, Rodriguez E et al (2015) Three-dimensional imaging and templating improve glenoid implant positioning. J Bone Joint Surg Am 97:651–658. https://doi.org/10.2106/JBJS.N.00493
Suero EM, Citak M, Lo D et al (2013) Use of a custom alignment guide to improve glenoid component position in total shoulder arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 21:2860–2866. https://doi.org/10.1007/s00167-012-2177-1
Chaoui J, Hamitouche C, Stindel E, Roux C (2011) Recognition-based segmentation and registration method for image guided shoulder surgery. Conf Proc Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf 2011:6212–6215. https://doi.org/10.1109/IEMBS.2011.6091534
Moineau G, Levigne C, Boileau P et al (2012) Three-dimensional measurement method of arthritic glenoid cavity morphology: feasibility and reproducibility. Orthop Traumatol Surg Res OTSR 98:S139–S145. https://doi.org/10.1016/j.otsr.2012.06.007
Walch G, Badet R, Boulahia A, Khoury A (1999) Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplast 14:756–760
Molé D, Roche O, Riand N, et al (1999) Cemented glenoid component: results in osteoarthritis and rheumatoid arthritis. In: Walch G, Boileau P (eds) Shoulder arthroplasty. Springer, Berlin, Heidelberg, pp 163–171
Jain N, Pietrobon R, Hocker S et al (2004) The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am 86-A:496–505
Singh A, Yian EH, Dillon MT et al (2014) The effect of surgeon and hospital volume on shoulder arthroplasty perioperative quality metrics. J Shoulder Elb Surg Am Shoulder Elb Surg Al 23:1187–1194. https://doi.org/10.1016/j.jse.2013.11.017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Adrien Jacquot is a consultant for Tornier-Wright Medical and for Smith and Nephew Company.
M. Jean Chaoui is an employee of Imascap and owns stock equity in Imascap.
M. Pierric Deransart is an employee of Imascap.
Pr. Daniel Mole receives royalties from Tornier-Wright Medical and is a consultant for Tornier-Wright Medical.
Pr. Pascal Boileau and Dr. Gilles Walch receive royalties from Tornier/Wright Company and equity from Imascap.
Dr. Marc-Olivier Gauci and Dr. Mohammed Baba have no conflict of interest.
Disclaimer
None
Ethics approval
The Institutional Review Board of the ethical committee of the Hôpital Privé Jean Mermoz and the Centre Orthopédique Santy approved this project (Study 20.1611).
Electronic supplementary material
ESM 1
(XLSX 31 kb)
Rights and permissions
About this article
Cite this article
Jacquot, A., Gauci, MO., Chaoui, J. et al. Proper benefit of a three dimensional pre-operative planning software for glenoid component positioning in total shoulder arthroplasty. International Orthopaedics (SICOT) 42, 2897–2906 (2018). https://doi.org/10.1007/s00264-018-4037-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4037-1