Abstract
Purpose
The purpose of this study is to investigate and compare the surgical site infection (SSI) rates of children and adults after open tibia fracture at a single medical centre.
Methods
A retrospective study was performed on patients who sustained open tibia fractures and who received treatment at our hospital from 2012 to 2016. Data on age, gender, fracture site, Gustilo-Anderson grade, treatment management, and culture results from the infection site were recorded.
Results
Overall, 37 children with a mean age of 7.19 ± 2.28 years and 89 adults with a mean age of 40.38 ± 13.53 years were enrolled. The rate of SSIs was 13.5% (6/37) in children, which was significantly lower than the 21.3% (19/89) rate in adults (p < 0.001). The mean number of days to discharge was 12.86 ± 10.25 in children, which was significantly lower than the mean of 28.67 ± 16.92 days in adults (p < 0.001). Furthermore, the average waiting time for soft tissue recovery before definitive surgery was 1.41 ± 1.79 and 8.42 ± 4.38 days in children and in adults, respectively, and the difference was significant (p < 0.001). Early infection occurred more frequently in adults (5/19) than in children (0/6). Staphylococcus aureus was the most commonly found pathogen in both groups.
Conclusion
The SSI rate of paediatric patients after open tibia fracture fixation is significantly lower than that of adults, and the prognosis of the former is superior. The results indicate a superior ability of soft tissue recovery and infection resistance after open tibia fracture fixation among children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of their weaker and immature immune system, children are more susceptible to many pathogenic viruses and bacteria compared with adults [1]. The risk of surgical site infection (SSI) after fracture fixation in children is considered to be higher than that in adults. However, a recent study from Nandra (2017) showed that the infection rate of children (aged 2–16 years) with open tibia fractures (Gustilo-Anderson grades I–III) was lower than that of adults and that such pediatric infections had a better prognosis [2]. However, the data on adults were cited from other reports.
In regard to some other diseases, paediatric patients also showed better prognosis than adults. Researchers have proved that the prevalence of acute lung injury (ALI) in children with critical diseases was lower than that of adults with the same conditions [3,4,5,6,7]. Simarmata and Sebastian reported that after infection with Chikungunya virus, symptoms among children usually resolved during the early and acute phase of the disease and they healed better compared to adults [8, 9]. Zingarelli also demonstrated that the severity of ALI was age-dependent in a haemorrhagic shock-induced ALI and systemic inflammatory response syndrome (SIRS) animal model, with adult animals more severely affected than young animals [10]. However, the difference in the rate of SSI after open fracture fixation between children and adults from the same medical centre has never been studied before.
Due to the differences in physiological conditions and the response to diseases between children and adults, we hypothesized that the SSI rates after open tibia fracture fixation should demonstrate disparities between children and adults. We assessed and compared the infection rate and the time to discharge between paediatric and adult patients who sustained open tibia fractures at a major orthopaedic hospital in a city with a population of seven million inhabitants over a five year observation period. In this study, we aimed to improve the understanding of the difference in the rates of SSI between children and adults, which may provide guidance for distinguishing treatments for children and adults in clinical practice.
Patients and methods
In this retrospective study from January 2012 to December 2016, the records of patients with traumatic open tibia fractures were retrieved from the database of Fuzhou Second Hospital Affiliated to Xiamen University. The eligible age of children was set from five to 16 years and that of adults from 16 to 65 years according to Nandra [2]. All files of the patients were reviewed with the approval of the hospital.
The following data were extracted from the database: age, gender, fracture site, the Gustilo-Anderson grade, the classification and initial management of the fracture, time to debridement, soft tissue procedures, definitive management, the in-hospital days’ cost, complications, associated comorbidity, and the results of bacterial cultures. The inclusion criteria were as follows:
-
1.
Age from five to 65 years
-
2.
Open tibia fracture
-
3.
Debridement performed within six hours after trauma
-
4.
Fracture fixed in our hospital.
The exclusion criteria included the following:
-
1.
Diabetes mellitus
-
2.
Smoking history
-
3.
Peripheral vascular disease
-
4.
Neuromuscular disease
-
5.
Metabolic bone disorders
-
6.
Pathological fracture
For infection prophylaxis, cefazolin sodium was conventionally used as soon as possible after admission and was used once again within 24 hours after operation in both groups of patients.
In the present study, treatment management included emergency debridement followed by temporary external fixation, K-wire placement, plaster casting, calcaneal traction, and, in some cases, alternative definitive fixations (such as intramedullary nail/plate/elastic intramedullary nail) according to the soft tissue conditions. All patients had continuous follow-up records. Once the diagnosis of infection was confirmed, “superficial infection” or “deep infection” was specified according to the US CDC guidelines [11]. An important test that helps diagnose SSI is a positive bacterial culture from the infection site. For bacterial identification, cultures for pathogenic microorganisms are obtained by incisional drainage or needle aspiration. The collected material should be immediately sealed and sent to the laboratory within one hour. According to the classification suggested by Metsemakers [12], SSI is divided into three types. Early infection (< 2 weeks) involves classic signs of infection and is accompanied by systemic signs of infection. The second type is delayed infection (2–10 weeks), which involves persistent signs of early infection with signs of late infection such as a fistula. The third type is late infection (> 10 weeks).
Statistical analysis
The SPSS 22.0 software was used for all statistical analysis. Descriptive statistics were conducted for continuous variables using mean ± standard deviation (SD). A test of comparison between two independent or more than two groups was performed using a two-sided Student t test or one-way analysis of variance at a 5% level of significance (2.5% at each end). Descriptive statistics of categorical variables were represented as the frequency and percentage. A chi-square test was employed to compare the differences in rates among different groups at a 5% level of significance (2.5% at each end).
Results
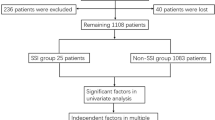
Infection rates of SSI
A total of 37 children (25 boys and 12 girls) aged 7.19 ± 2.28 years on average (range from 5 to 13) and 89 adults (68 males and 21 females) aged 40.38 ± 13.53 years on average (range from 17 to 65) were enrolled in this study. There were no significant differences in terms of gender and Gustilo-Anderson grade classification between the groups; however, there was a significant difference in age. All patients had achieved bone healing at the last follow-up. The Gustilo-Anderson grades are shown in Table 1. Seventeen children and eight adults subsequently accepted initial definitive external fixation. Another 20 children and 81 adults accepted plaster/temporary mono-lateral fixator/calcaneal traction after debridement; once the injuries were well controlled, further definitive fixations, such as definitive external fixation/intramedullary nail/elastic nail/K-wire/plate were chosen accordingly. The mean number of days to discharge was 12.86 ± 10.25 (3–46) in children, which was significantly less than the mean of 28.67 ± 16.92 (9–87) days in adults (p < 0.001) (Fig. 1a). The mean duration time from fracture occurrence to definitive fixation surgery was 1.41 ± 1.79 (0–7) days in children and 8.42 ± 4.38 (0–19) days in adults (Fig. 1b).
The SSI rate in the pediatric group (13.5%, 6/37) was significantly lower than that of adults (21.3%, 19/89) (p < 0.001). The mean number of days to discharge of the infected patients was 25.33 ± 13.08 (8–46) in children and 36.79 ± 25.89 (10–95) in adults (p > 0.05) (Fig. 1c).
Moreover, four cases were recorded as “superficial infection” and two cases as “deep infection” in children. These two kinds of cases were recorded for 14 and five adults, respectively (Table 1). Deep infection was observed in two patients in the paediatric group; both were Gustilo-Anderson grade III and both were healed through regular bandage changes and antibiotic treatment. However, their in-hospital stays were longer than those of the superficially infected patients. Deep infection was observed in five cases among the adult patients. Two of them were Gustilo-Anderson grade II and both were treated with internal plate fixation after early debridement and days of calcaneal traction or plaster casting; three cases among them underwent a second debridement and negative pressure wound treatment, and one of the three cases was debrided three times. However, none of the children who were classified as Gustilo-Anderson grade II developed a deep infection. In addition, all wounds healed well, and flap transfer technology was not used in any children, although it was used in two adults.
Seventeen children and eight adult patients were treated with initial definitive fixation devices after emergency debridement, of whom five children and four adults developed infections (Table 2). All of the infected patients were fixated with external devices and were successfully healed by intravenous antibiotics and debridement surgeries. Another case of an infected child and 15 cases of infected adults were treated with delayed definitive fixation after emergency debridement and days of calcaneal traction or plaster casting. The child was also treated with an external fixator, while seven of the 15 adults with infections were treated by an external fixator; another six adults were treated using an internal plate, with one adult treated using K-wires and one by intramedullary nailing. None of the pediatric patients who were initially treated with a plaster cast or elastic intramedullary nail fixation developed an infection.
Further analysis showed that among 19 adults with SSI, five were diagnosed within two weeks (early onset), 13 showed delayed infections, and one was diagnosed with late infection after internal fixation surgery. In contrast, all of the six children with SSI were diagnosed as having delayed infections. The relative infection numbers for each classification are shown in Fig. 2.
The numbers of patients classified according to Metsemakers [12]
Bacteriological analysis
In our study, the positive bacterial culture rate from incision secretions was 100% (6/6) in children. Of these, 2/6 were Staphylococcus aureus, 2/6 were Pseudomonas aeruginosa, and 1/6 was Enterococcus faecalis; the other 1/6 was a mixed infection of Pseudomonas aeruginosa and Acinetobacter baumanii. In adults, the positive bacterial culture rate was also 100% (19/19), of which 8/19 were Staphylococcus aureus, followed by 3/19 Enterobacter cloacae and 2/19 Staphylococcus haemolyticus (Table 3). Staphylococcus aureus was predominantly isolated in infected children and adults.
Discussion
In this study, we found that after open tibia fractures, the infection rate in children (13.5%, 6/37) was significantly lower than that in adults (21.3%, 19/89). According to previous studies, the immune system response to infections in children is significantly different from that in adults [8, 9, 13]. The difference of the SSI rate in the current study could be due to distinct immune responses between children and adults. However, some studies attributed such differences either to the relatively low-energy trauma associated with fractures in children compared with that of adults or to the different fixation devices used between children and adults [14, 15].
Studies reported SSI rates after open fractures in children of 7.69 [16] and 7.14% [17], which were lower than those of adults with similar injuries, i.e., 15.33 [18] and 22.62% [19] in separate studies. Our results were in accord with the previous reports and were consistent with the results of a recent study [2], which reported that the rate of infection in children with open tibia fractures was lower than that of adults and that the prognosis of children was superior to that of adults.
Our analysis of patients with open tibia fractures demonstrated that the average number of days to discharge was significantly lower in children compared with adults (12.86 ± 10.25 vs 28.67 ± 16.92) (p < 0.001) (Fig. 1a). Although the days to discharge in this study was longer than that in a previous report [2], this result was partly due to the fact that many patients were treated with delayed definitive fixation after debridement, which required many days of hospitalization to obtain soft tissue recovery before the final surgery. This finding also may be related to our physicians’ preferences. We tend to use traction, plaster casting, and a temporary mono-lateral fixator (20/37 in children and 81/89 in adults) as an initial treatment after debridement, which allows the condition of the soft tissue to improve for the definitive fixation surgery. Moreover, the time elapsed in preparation for definitive surgery for children (1.41 ± 1.79 days) was significantly less than that of adults (8.42 ± 4.38 days), which also demonstrated the faster recovery in children than in adults.
In the patients with infection, further analysis showed that all of the children with SSI (n = 6) presented delayed infections. Whereas only 13/19 showed delayed infection in adults, 5/19 cases were early onset, and 1/19 presented late infection. Adult patients were more susceptible to early infection than children (Fig. 2). However, none of the children with SSI developed early infection.
Further, among the 19 infected adult patients, 15 were treated with delayed definitive fixation after emergency debridement, while only four adults were treated with initial definitive external fixation, suggesting that emergency debridement combined with initial definitive external fixation may reduce the risk of infection in adults. This observation may also be related to the use of a locking plate in some of the patients with delayed definitive fixation. This finding was consistent with the results of previous reports. The patients treated with external fixation were more prone to infection, both among children and adults, probably because of the more serious injuries and worse soft tissue conditions in those patients.
Hospitalization days in children (25.33 ± 13.08) after infection were apparently fewer than those of adults (36.79 ± 25.89); however, the difference was not comparable, likely because the guardians of children were often required to be in the hospital until they were completely healed, whereas adults were usually discharged for outpatient treatment once they had recovered to a certain extent.
We focused on open tibia fractures because these fractures are usually caused by high-energy trauma both in children and adults. Furthermore, the treatments for children and adults with open tibia fractures are similar. Generally, emergency debridement should be considered within six hours after trauma, followed by initially definitive external fixation, or by plaster casting/temporary external fixation/bone traction and then alternative-method fixation devices (permanent external fixation/intramedullary nail/locking plate).
Children are in a period of rapid physical growth, and the biology of fracture repair procedures is different from that of adults. Because of the exuberant metabolism and vascular regeneration, children have excellent healing capacity in soft tissue and bone, which benefits the recovery after trauma and surgery. Moreover, it has been widely reported that the immune system response to infections in children is significantly different from that in adults, and the expression levels of inflammatory mediators (such as IL-10 and IL-12) after infection in children are significantly different from those of adults [8, 9, 13]. The difference in the SSI rate in the current study could have been due to the distinct immune responses between children and adults. These findings indicate that determining the different mechanisms of immune responses to infections between children and adults may be an important endeavor.
This study is noteworthy since many previous studies focused only on the prevalence of infection individually in children or adults. Few reports have compared the difference of SSI rates in the paediatric population with that of adults. Moreover, this is a single-centre retrospective study, which ensures the use of similar techniques in the treatments. Because of these factors, these study findings present valid comparisons.
Some limitations also existed in this study. It was a retrospective study and the number of cases was limited, especially in the paediatric group. We compared the infection rate after open tibia fracture in children and adults; however, we did not discuss other risk factors for post-operative infection, such as the characteristics of the trauma, the instrument of fixation, the duration of surgery, and whether and what kinds of antibiotics were used to prevent/treat infection. There were no Gustilo-Anderson grade IIIC fractures in this study because patients with blood vessel or nerve damage were treated by the Hand Surgery Department, which may affect the results. Nevertheless, we believe this study is still of great importance. It proves that the infection rate after open tibia fracture in children is significantly lower than that of adults, and the time to discharge was much less. We hope it will remind other researchers to focus on the different mechanisms of the immune response to infections between children and adults.
Conclusion
SSI is one of the most common and serious complications of orthopaedic trauma surgery. The rate of SSIs after open tibia fracture fixation was lower in children than in adults, and the prognosis of the children was superior to that of the adults. Early infection is more common in adult patients, which indicates that children have a superior capacity for soft tissue recovery and infection resistance after open tibia fracture. There might be some protective mechanisms in terms of innate immunity that protects children from infection, and further research is required in this field.
References
Simon AK, Hollander GA, McMichael A (2015) Evolution of the immune system in humans from infancy to old age. Proc Biol Sci 282(1821):20143085. https://doi.org/10.1098/rspb.2014.3085
Nandra RS, Wu F, Gaffey A, Bache CE (2017) The management of open tibial fractures in children: a retrospective case series of eight years’ experience of 61 cases at a paediatric specialist centre. Bone Joint J 99-B(4):544–553. https://doi.org/10.1302/0301-620X.99B4.37855
Acute Respiratory Distress Syndrome N, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342(18):1301–1308. https://doi.org/10.1056/NEJM200005043421801
Dahlem P, van Aalderen WM, Hamaker ME, Dijkgraaf MG, Bos AP (2003) Incidence and short-term outcome of acute lung injury in mechanically ventilated children. Eur Respir J 22(6):980–985
Flori HR, Glidden DV, Rutherford GW, Matthay MA (2005) Pediatric acute lung injury: prospective evaluation of risk factors associated with mortality. Am J Respir Crit Care Med 171(9):995–1001. https://doi.org/10.1164/rccm.200404-544OC
Wood JH, Partrick DA, Johnston RB Jr (2010) The inflammatory response to injury in children. Curr Opin Pediatr 22(3):315–320. https://doi.org/10.1097/MOP.0b013e328338da48
Zimmerman JJ, Akhtar SR, Caldwell E, Rubenfeld GD (2009) Incidence and outcomes of pediatric acute lung injury. Pediatrics 124(1):87–95. https://doi.org/10.1542/peds.2007-2462
Sebastian MR, Lodha R, Kabra SK (2009) Chikungunya infection in children. Indian J Pediatr 76(2):185–189. https://doi.org/10.1007/s12098-009-0049-6
Simarmata D, Ng DC, Kam YW, Lee B, Sum MS, Her Z, Chow A, Leo YS, Cardosa J, Perera D, Ooi MH, Ng LF (2016) Early clearance of Chikungunya virus in children is associated with a strong innate immune response. Sci Rep 6:26097. https://doi.org/10.1038/srep26097
Zingarelli B, Hake PW, O'Connor M, Burroughs TJ, Wong HR, Solomkin JS, Lentsch AB (2009) Lung injury after hemorrhage is age dependent: role of peroxisome proliferator-activated receptor gamma. Crit Care Med 37(6):1978–1987. https://doi.org/10.1097/CCM.0b013e31819feb4d
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27(2):97–132
Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MH, Borens O, Kates S, Morgenstern M (2016) Infection after fracture fixation: current surgical and microbiological concepts. Injury. https://doi.org/10.1016/j.injury.2016.09.019
Razavi A, Bagheri N, Azadegan-Dehkordi F, Shirzad M, Rahimian G, Rafieian-Kopaei M, Shirzad H (2015) Comparative immune response in children and adults with H. pylori infection. J Immunol Res 2015:315957. https://doi.org/10.1155/2015/315957
Chen W, Lv H, Liu S, Liu B, Zhu Y, Chen X, Yang G, Liu L, Zhang T, Wang H, Yin B, Guo J, Zhang X, Li Y, Smith D, Hu P, Sun J, Zhang Y (2017) National incidence of traumatic fractures in China: a retrospective survey of 512 187 individuals. Lancet Glob Health 5(8):e807–e817. https://doi.org/10.1016/S2214-109X(17)30222-X
Mayranpaa MK, Makitie O, Kallio PE (2010) Decreasing incidence and changing pattern of childhood fractures: a population-based study. J Bone Miner Res 25(12):2752–2759. https://doi.org/10.1002/jbmr.155
Vallamshetla VR, De Silva U, Bache CE, Gibbons PJ (2006) Flexible intramedullary nails for unstable fractures of the tibia in children. An eight-year experience. J Bone Joint Surg Br 88(4):536–540. https://doi.org/10.1302/0301-620X.88B4.17363
Srivastava AK, Mehlman CT, Wall EJ, Do TT (2008) Elastic stable intramedullary nailing of tibial shaft fractures in children. J Pediatr Orthop 28(2):152–158. https://doi.org/10.1097/BPO.0b013e318165210d
Southeast Fracture C (2016) LCP versus LISS in the treatment of open and closed distal femur fractures: does it make a difference? J Orthop Trauma 30(6):e212–e216. https://doi.org/10.1097/BOT.0000000000000507
Momaya AM, Hlavacek J, Etier B, Johannesmeyer D, Oladeji LO, Niemeier TE, Herrera N, Lowe JA (2016) Risk factors for infection after operative fixation of tibial plateau fractures. Injury 47(7):1501–1505. https://doi.org/10.1016/j.injury.2016.04.011
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, H., Chen, S., Shi, Y. et al. Children with open tibial fractures show significantly lower infection rates than adults: clinical comparative study. International Orthopaedics (SICOT) 43, 713–718 (2019). https://doi.org/10.1007/s00264-018-3996-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3996-6