Abstract
Background
Metaphyseal-diaphyseal junction (MDJ) fractures of the distal humerus are problematic to reduce and more susceptible to post-operative complications. This biomechanical study was designed to compare Kirschner wires (KW), lateral external fixation, and elastic stable intramedullary nails (ESIN) in simulated transverse MDJ fractures of various heights.
Method
Sagittally oblique, transverse MDJ fractures were created in fourth-generation composite bone models at three levels: high, mid, and low fractures, respectively, and then fixed with either Kirschner wires, lateral external fixation (EF), or ESIN respectively and tested in extension, flexion, valgus, varus, internal, and external rotations.
Results
In the high fractures, ESIN had better overall stiffness than the other techniques. In the mid groups, three crossed pinning (1-medial and 2-lateral pins) had the best overall stiffness, followed by two crossed pinning (1-medial and 1-lateral pins). In the low fractures, three crossed pinning was superior to all other techniques. Two crossed pinning and three -lateral pinning techniques yielded comparable stiffness in the low fracture model.
Conclusions
From a biomechanical perspective, ESIN provides the best overall stability for fractures located in the upper region of the MDJ, while percutaneous pinning is superior in stabilizing fractures of the lower region. Two lateral and one medial pins make the most stable crossed pinning construct for these fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Supracondylar humeral fracture (SHF) is a common fracture in the paediatric population. It primarily occurs within the metaphyseal region of the distal humerus without intercondylar involvement [1]. Despite the abundant experience of the orthopaedic society in coping with them, some special cases of SHF remain challenging. SHF with a high fracture line, as classified by Bahk, is one of them [1]. Fayssoux RS et al. referred to this type of fracture as metaphyseal-diaphyseal junction (MDJ) fracture [2]. Distal humeral MDJ fractures which account for only about 3% of SHFs are not only hard to reduce but are also more susceptible to post-operative complications such as cubital varus and loss of reduction [1,2,3].
Currently, percutaneous pinning is widely used for managing displaced supracondylar humeral fractures in children, irrespective of the severity of fracture or the method of reduction used. Percutaneous pinning may be technically challenging in MDJ fractures due to the difficulties encountered in reducing and fixing these fractures [1, 2]. Fayssoux RS et al. found that for MDJ fractures, the more transverse the fracture lines were, the more difficult it was to reduce them [2]. Even though achieved, percutaneous pinning may not yield the best stiffness. For this reason, other fixation techniques such as lateral external fixation and elastic stable intramedullary nails have also been used in treating SHFs, many with acceptable outcomes [4,5,6,7]. However, despite the numerous biomechanical studies comparing the efficacy of the various techniques, none have really focused on the more problematic transverse MDJ fracture.
This biomechanical study was designed to compare fixation techniques using Kirschner wires, lateral external fixation, and elastic stable intramedullary nailing system in simulated transverse MDJ fractures of the distal humerus, using composite bone models. Different locations of the fracture lines were analyzed respectively in order to best simulate clinical circumstances. The purpose of this study was to find out the most suitable fixation technique for various heights of transverse MDJ fractures.
Materials and methods
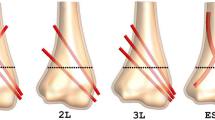
Thirty-six fourth-generation composite humeri (Model # 3404, Sawbones, Pacific Research Laboratories, Vashon Island, WA) were used in this study. The composite humeri had a canal diameter of 9.0 mm and tapered distally. The distal humeral MDJ region was determined according to Fayssoux RS et al. [2]. The lower border of the MDJ region was a horizontal line drawn tangentially to the top of the upper border of the olecranon fossa, while the upper border was a transverse line drawn along the width of the humeral shaft at the point where the diameter of the metaphysis was 10% wider than that of the diaphysis. The lower and upper borders served as surface markings for the low and high MDJ fracture lines respectively. A third line was drawn midway between these two lines, which marked the mid fracture line. A transverse osteotomy with a 10° sagittal obliquity was performed along these lines to simulate a type III, transverse supracondylar fracture in the MDJ region (Fig. 1). For consistency of pin orientations, holes for pin trajectories were predrilled using a 1.5-mm pin through a custom made pin guide before the osteotomy was performed.
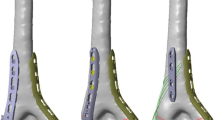
The fractures were fixated with either 2.0-mm Kirschner wires (K-wires) (Double Medical Technology Inc., Xiamen, China), lateral external fixation (EF, Wuhan Constant Technology Inc., Wuhan, China), or 3.0-mm elastic stable intramedullary nails (ESIN, Double Medical Technology Inc., Xiamen, China). EF and ESIN were applied according to the methods previously described [4, 7]. The lateral external fixation comprised of two 3.0-mm threaded half pins, one 4.0-mm stainless steel connecting rod, two connectors plus one free lateral entry 2.0-mm K-wire. The fixation techniques for each fracture group are shown in Fig. 2. For the high fractures, it was technically impossible to insert two K-wires from the lateral part of the epiphysis due to the sharp angle that the one pin made with the fracture line, so we only tested two crossed pinning (1-medial and 1-lateral pins) in this group. For the middle fractures, it became possible to insert two pins but impossible to insert three, so we also included three crossed pinning (1-medial and 2-lateral pins). When it came to the low fractures, three lateral pinning was also feasible and thus included. The lateral pins were placed directly from the radial side in a divergent configuration.
a Fixation techniques for the high fracture group. 2C: 2-crossed pins (1-medial and 1-lateral K-wires); EF: lateral external fixation (2 half pins, 1 lateral K-wire); ESIN: elastic stable intramedullary nails. b Fixation techniques for the mid fracture group. 2C: 2-crossed pins (1-medial and 1-lateral K-wires); 3C: 3-crossed pins (1-medial and 2-lateral K-wires); EF: lateral external fixation (2 half pins, 1 lateral K-wire); ESIN: elastic stable intramedullary nails. c Fixation techniques for the low fracture group. 2C: 2-crossed pins (1-medial and 1-lateral K-wires); 3C: 3-crossed pins (1-medial and 2-lateral K-wires); 3L: 3-lateral pins; EF: lateral external fixation (2 half pins, 1 lateral K-wire); ESIN: elastic stable intramedullary nails
Prior to testing, each fixation was fluoroscopically imaged to ensure consistency among techniques and pin orientations. Humeri were then horizontally mounted to a custom made metal testing table attached to a microcomputer controlled universal testing machine (WDW-100E, Jinan, China) and tested in extension, flexion, valgus, and varus and then to an electromechanical torsion testing machine (CTT 1202, MTS systems (China) Co., Ltd., China) and tested in internal and external rotations. Loads were applied to the distal fragment at a rate of 0.5 mm/s to a maximum of 5 mm of displacement in the compression tests and at 0.5 degrees/s to a maximum of 10 degrees in the rotational tests. Each biomechanical testing was sampled at 10 Hz [8, 9].
Stiffness data for the models were recorded as mean ± standard deviation. The data were analyzed using multivariate analysis of variance (MANOVA) on SPSS 22 (IBM Corp., USA) to assess the differences in stiffness for each technique among groups. A pair-wise comparison was further done when general differences were detected. Statistical significance was determined as p < 0.05.
Results
For the high fractures, ESIN yielded the best stiffness in all directions. Significant difference existed in all groups in the models for all loading directions except in internal and external rotations. Two crossed pinning (1-medial and 1-lateral pins, 2C) and EF had comparable stiffness (Fig. 3).
Stiffness data for the high fracture group. a Stiffness in flexion, extension, valgus, and varus. b Torque in internal and external rotations. 2C: two crossed pins (1-medial and 1-lateral pins); EF: lateral external fixation; ESIN: elastic stable intramedullary nails; IR: internal rotation; ER: external rotation
Three crossed pinning (1-medial and 2-lateral pins, 3C) had the best overall stiffness for the middle fractures, followed by 2C. EF and ESIN had comparable but inferior stiffness. Three crossed pins were significantly better than 2C in flexion, extension, and valgus and insignificantly better in varus and rotations (Fig. 4).
Stiffness data for the mid fracture group. a Stiffness in flexion, extension, valgus and varus. b Torque in internal and external rotations. 2C: two crossed pins (1-medial and 1-lateral pins); 3C: three crossed pins (1-medial and 2-lateral pins); EF: lateral external fixation; ESIN: elastic stable intramedullary nails; IR: internal rotation; ER: external rotation
For the low fractures, 3C still had the best overall stiffness, followed by 2C and 3-lateral pins (3L). There was however no significant difference between 2C and 3C in all directions in the pair-wise comparison. EF remained the weakest overall in the low fracture group (Fig. 5).
Stiffness data for the low fracture group. a Stiffness in flexion, extension, valgus and varus. b Torque in internal and external rotations. 2C: two crossed pins (1-medial and 1-lateral pins);3C: three crossed pins (1-medial and 2-lateral pins); 3L: three lateral pins; EF: lateral external fixation; ESIN: elastic stable intramedullary nails; IR: internal rotation; ER: external rotation
When 2C, ESIN, and EF were compared across the three fracture models, they all had the greatest stiffness in the low fracture models in compression loadings. However, for rotational loadings, 2C was stiffest in the low fracture model, while ESIN and EF were stiffest in the high fracture model.
Discussion
In recent years, MDJ fractures are gaining more and more attention, either as one subtype of supracondylar humeral fracture or as a distinct type of injury. In MDJ fractures, due to the angles the metaphyseal flare of the distal humerus makes with the humeral shaft and the higher location of the fracture line, percutaneous pinning may be technically demanding and do not guarantee adequate fixation [2]. Despite those concerns, pinning remains the mainstream treatment for these fractures. Other techniques such asEF and ESIN have also been proposed as an alternative option for displaced high SHFs and yielded satisfactory outcomes [4,5,6,7, 10].
MDJ fractures had been classified as traverse and oblique fractures [2], and a third type named comminuted fracture was proposed later [11]. The traverse type was most challenging because of the difficulty in achieving and maintaining stability [2]. Therefore, our study utilized a model of traverse fracture to simulate the most challenging clinical circumstance. The shape of the humerus changed dramatically in the MDJ region, so we further divided the region into two parts—the upper and the lower region, with a line that went midway between the upper and the lower border of the MDJ region. Since the morphology of a bone was a decisive factor to the selection and effect of fixation techniques, the most suitable fixation might vary according to the fracture site.
According to the fixation models, ESIN showed the best overall stabilizing capability in the high fractures, which coincided with the recent advocacy of ESIN in MDJ fractures [5, 12]. In these fractures, the fracture line went very close to the crossing point of the crossed pins, drawing the rotation center very close to the fracture line. Therefore, the anti-rotation capability of crossed pinning was largely diminished, leaving the fractures prone to rotatory forces. Besides, the higher the fracture line was, the more technically demanding crossed pinning became in the composite bone model fixations. However, despite the recent advocacy of ESIN in the treatment of SHFs [4, 5], its stiffness decreased significantly with the lowering of the fracture site in our MDJ fracture model. In lower fracture sites, the nails engaged in the distal fragment would be shorter, especially in the case of a sagittal oblique fracture. This would mean that, the more oblique the fracture line is in the sagittal plane the less stable it will be with ESIN. Also, ESIN is typically indicated for diaphyseal fractures of long bones. Although good clinical results have been reported with the technique in the fixation of “non-typical ESIN procedure” distal humeral fractures [4, 5, 12,13,14,15], fractures located in the MDJ region, that are far away from the bent portions of the nails, do not abide by the three point fragment fixation principle of ESIN [13]. In typical diaphyseal fractures, bends placed in the mid portion of the nails at the level of the fracture site produce a spring effect that adds to the stability of the fracture fixation [16]. The opposite bends of the nails also significantly increase resistance to sagittal and rotational forces [17]. As a result, fractures that were located in the lower region of the MDJ were not tightly held by the short distal portion of the nails. We believed this was the main reason why the high fractures that were located closer to the bent portions of the nails were more stable than those in the lower region.
Pinning demonstrated sufficient stiffness and resistance to rotation in all directions in the mid and low fractures. Crossed pinning had better overall stiffness than ESIN and EF. This advantage increased with the decrease of fracture height. In other words, in the lower region, crossed pinning demonstrated superior stiffness compared to ESIN. Because of the impractical sharp angle that the pins must make to cross the fracture line in mid and high fractures, we only performed lateral pinning in the low group. Lateral pinning was significantly inferior to crossed pinning except in valgus, where crossed pinning was comparable to lateral pinning.
Torsional migration was said to be the most important factor for development of cubital varus [18], and ulnar pinning was an important anti-torsion device. However, as reported in classical SHFs, lateral pinning was often preferred to avoid iatrogenic ulnar nerve injury [3, 19, 20]. Since most reported iatrogenic ulnar nerve injury resolved spontaneously and left no permanent sequelae, we believed that crossed pinning remained the choice of thumb in MDJ fractures of the lower region. For cases in which crossed pinning are hard to perform, lateral pinning remains a good substitute of fixation.
Increased pin numbers, however, did not significantly increase stiffness. There were no significant difference between two crossed pins (1-medial and 1-lateral pins) and three crossed pins (1-medial and 2-lateral pins) in all directions. Feng et al. also reported similar findings in SHFs with lateral obliquity [9]. Maximizing pin number alone may not contribute much to the overall stability. Factors like fracture patterns, pin size and entry points should also be taken into consideration [21]. A study by Jaeblon, however, held the opposite opinion by stating that three lateral pins yielded better stiffness than two lateral pins or two crossed pins in the “high” type SHF, which was similar to our MDJ fracture [22]. Their usage of sawbones, rather than composite bone models, may partly explain the difference [23].
Since it was first reported by Slongo in 2008, EF had been used in SHFs that were hard to achieve or maintain stability [7]. Hohloch found that EF was more stable than crossed pinning, and an ulnar Kirschner wire, instead of a radial one, would further enhance the anti-torsion capability [24]. However, in our study, EF did not show any advantage over pinnings in all fracture sites in both models. The relatively higher fracture line of MDJ fractures and the usage of a radial K-wire rather than an ulnar one might explain the difference.
Despite the above results, our study had several limitations. Firstly, owing to the difficulty in obtaining paediatric cadaver bones, adult size synthetic bones were used instead. Also, the results obtained were purely simulated and were not experimentally tested in real clinical patients. However, since our ultimate goal was to compare fixation techniques across the three fracture heights, we believe the results obtained would be similar even if paediatric models were used. Secondly, our study only included traverse fractures which clinically are more challenging to reduce and maintain fixation than the other oblique and comminuted types, which may have higher incidences in clinical practice. Also, similar to most previous biomechanical tests, each fixation technique in our study was randomly tested in each of the six directions until the fixation technique was completely tested. This may also affect the overall stability of the fixated models. For this reason, we chose the endpoints of 5 mm and 10 degrees to avoid damage to the models after each loading [9, 25].
Conclusion
This study demonstrated the most suitable fixation technique for MDJ fractures from a biomechanical point of view. ESIN yielded the best overall stiffness for fractures in the upper region of the distal MDJ, while percutaneous pinning yielded the best overall stiffness in the lower region. Two lateral and one medial pins make the most stable construct and is recommended as the pinning technique of choice for these lower MDJ fractures. These findings may be helpful to the selection of fixations in clinical practice.
References
Bahk MS, Srikumaran U, Ain MC, Erkula G, Leet AI, Sargent MC, Sponseller PD (2008) Patterns of pediatric supracondylar humerus fractures. J Pediatr Orthop 28(5):493–499. https://doi.org/10.1097/BPO.0b013e31817bb860
Fayssoux RS, Stankovits L, Domzalski ME, Guille JT (2008) Fractures of the distal humeral metaphyseal-diaphyseal junction in children. J Pediatr Orthop 28:142–146. https://doi.org/10.1097/BPO.0b013e3181653af3
Dekker AE, Krijnen P, Schipper IB (2016) Results of crossed versus lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: a systematic review and meta-analysis. Injury 47:2391–2398. https://doi.org/10.1016/j.injury.2016.08.022
Lacher M, Schaeffer K, Boehm R, Dietz HG (2011) The treatment of supracondylar humeral fractures with elastic stable intramedullary nailing (ESIN) in children. J Pediatr Orthop 31:33–38. https://doi.org/10.1097/BPO.0b013e3181ff64c0
Marengo L, Canavese F, Cravino M, De Rosa V, Rousset M, Samba A, Mansour M, Andreacchio A (2015) Outcome of displaced fractures of the distal metaphyseal-diaphyseal junction of the humerus in children treated with elastic stable intramedullary nails. J Pediatr Orthop 35:611–616. https://doi.org/10.1097/BPO.0000000000000340
Sénès FM, Catena N (2012) Intramedullary osteosynthesis for metaphyseal and diaphyseal humeral fractures in developmental age. J Pediatr Orthop B 21:300–304. https://doi.org/10.1097/BPB.0b013e328353d96d
Slongo T, Schmid T, Wilkins K, Joeris A (2008) Lateral external fixation—a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am 90:1690–1697. https://doi.org/10.2106/JBJS.G.00528
Hamdi A, Poitras P, Louati H, Dagenais S, Masquijo JJ, Kontio K (2010) Biomechanical analysis of lateral pin placements for pediatric supracondylar humerus fractures. J Pediatr Orthop 30:135–139. https://doi.org/10.1097/BPO.0b013e3181cfcd14
Feng C, Guo Y, Zhu Z, Zhang J, Wang Y (2012) Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J Pediatr Orthop 32:196–200. https://doi.org/10.1097/BPO.0b013e318242a99a
Wagner FC, Strohm PC, Südkamp NP, Reising K (2015) Biomechanical evaluation of a new technique for external fixation of unstable supracondylar humerus fractures in children. Technol Health Care 23:453–461. https://doi.org/10.3233/THC-150905
Sen RK, Tripathy SK, Kumar A, Agarwal A, Aggarwal S, Dhatt S (2012) Metaphyseo-diaphyseal junction fracture of distal humerus in children. J Pediatr Orthop B 21:109–114. https://doi.org/10.1097/BPB.0b013e32834ba9d6
Ge YH, Wang ZG, Cai HQ, Yang J, Xu YL, Li YC (2014) Flexible intramedullary nailing had better outcomes than Kirschner wire fixation in children with distal humeral metaphyseal-diaphyseal junction fracture: a retrospective observational analysis. Int J Clin Exp Med 7:3568–3572
Havránek P, Pesl T (2002) Use of the elastic stable intramedullary nailing technique in non-typical pediatric fractures. Acta Chir Orthop Traumatol Cechoslov 69(2):73–78
Schäffer K, Böhm R, Dietz HG (2007) Elastic stable intramedullary nailing (ESIN) of supracondylar fractures of the humerus in children. Unfallchirurg 110(10):852–858
Cosma D, Vasilescu DE (2014) Elastic stable intramedullary nailing for fractures in children—specific applications. Clujul Med 87(3):147–151. https://doi.org/10.15386/cjmed-275
Ligier JN, Metaizeau JP, Prévot J, Lascombes P (1988) Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br 70(1):74–77
Flynn JM, Skaggs DL (2010) Femoral shaft fractures. In: Beaty JH, Kasser JR (eds) Rockwood and Wilkins fractures in children, 7th edn. Lippincott Williams & Wilkins, Philadelphia, p 812
Weinberg AM, Castellani C, Arzdorf M, Schneider E, Gasser B, Linke B (2007) Osteosynthesis of supracondylar humerus fractures in children: a biomechanical comparison of four techniques. Clin Biomech (Bristol, Avon) 22:502–509
Prashant K, Lakhotia D, Bhattacharyya TD, Mahanta AK, Ravoof A (2016) A comparative study of two percutaneous pinning techniques (lateral vs medial-lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J Orthop Traumatol 17:223–229. https://doi.org/10.1007/s10195-016-0410-2
Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K (2010) Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop 30(5):430–436. https://doi.org/10.1097/BPO.0b013e3181e00c0d
Gottschalk HP, Sagoo D, Glaser D, Doan J, Edmonds EW, Schlechter J (2012) Biomechanical analysis of pin placement for pediatric supracondylar humerus fractures: does starting point, pin size, and number matter? J Pediatr Orthop 32:445–451. https://doi.org/10.1097/BPO.0b013e318257d1cd
Jaeblon T, Anthony S, Ogden A, Andary JJ (2016) Pediatric supracondylar fractures: variation in fracture patterns and the biomechanical effects of pin configuration. J Pediatr Orthop 36:787–792
Landsman AS, Chang TJ (1998) Can synthetic bone models approximate the mechanical properties of cadaveric first metatarsal bone? J Foot Ankle Surg 37:122–127
Hohloch L, Konstantinidis L, Wagner FC, Strohm PC, Südkamp NP, Reising K (2016) Biomechanical comparison of different external fixator configurations for stabilization of supracondylar humerus fractures in children. Clin Biomech (Bristol, Avon) 32:118–123. https://doi.org/10.1016/j.clinbiomech.2015.12.003
Lee SS, Mahar AT, Miesen D, Newton PO (2002) Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop 22(4):440–443
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kamara, A., Ji, X., Liu, T. et al. A comparative biomechanical study on different fixation techniques in the management of transverse metaphyseal-diaphyseal junction fractures of the distal humerus in children. International Orthopaedics (SICOT) 43, 411–416 (2019). https://doi.org/10.1007/s00264-018-3968-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3968-x