Abstract
Purpose
Treatment of open tibial fractures with soft tissue and segmental bone defects is difficult. This study reports our results for treating these injuries with a combination of Papineau open bone grafting and vacuum-assisted wound closure (VAC).
Methods
The records of 19 patients with open tibial fractures with soft tissue and segmental bone defects treated with bone grafting and VAC from 2004 to 2010 were retrospectively reviewed. Outcomes included: time to complete granulation tissue coverage, wound healing, and bone union; length of hospitalization; frequency of debridement; number of deep tissue infections.
Results
Initial surgery was performed within 48 hours of injury. Ten fractures were Orthopaedic Trauma Association classification 41-A3, one was 41-C3, seven were 43-A3, and one was 43-C3. No surgical complications occurred, and the mean length of hospitalization was 11.0 ± 3.0 weeks (range, 7-18 weeks). The mean follow-up time was 59.35 ± 8.76 months. The mean time for complete wound healing was 7.76 ± 1.52 weeks (range, 6-11 weeks). Bone union was achieved in all patients at a mean of 33.88 ± 8.37 weeks (range, 23-53 weeks). Only one patient developed a deep tissue infection, which was treated with antibiotics and debridements, and complete bone union wound healing was achieved. Based on Paley grade, five outcomes were excellent, eight were good, and four were fair.
Conclusions
The combination of VAC and open bone grafting results in good outcome for patients with open tibial fractures and severe bone and soft-tissue defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in surgical techniques and antibiotic treatment, severe open fractures of the tibia with segmental bone defects (long-bone defect longer than 1.5 times the diameter of the bone) continue to be one of the most challenging problems for orthopaedic surgeons. Extensive bone and soft tissue defects always accompany high-energy open fractures, and as a result the injured bones lose their ability to heal and are prone to infection. Many techniques are used to treat these injuries, and there is currently no consensus on the best method [1,2,3]. Regardless of the method used, delayed and nonunions are common [4].
Papineau [5] introduced open bone grafting to treat these injuries, and the technique has been used for more than four decades with satisfactory results [6, 7]. Vacuum-assisted closure (VAC) is another technique that is widely used for the treatment of various soft-tissue defects, and again is associated with improved results over local wound care for infected wound and osteomyelitis [8,9,10,11]. While both techniques provide satisfactory outcomes in the majority of cases, studies of the long-term outcomes are lacking [12, 13]. Furthermore, there are few studies that have examined using the two techniques in combination.
At our institution, we have been using the Papineau technique of open bone grafting in combination with VAC to treat severe open tibial fractures with soft tissue and segmental bone defects. We hypothesized that using the two techniques in combination may improve the outcomes of either technique alone. The purpose of this report is to describe the combination technique, and our results.
Patients and methods
Patients
We retrospectively reviewed the records of patients with severe open tibial fractures with segmental bone defects who were treated by our team between March, 2004 and June, 2010.
Patients with diabetes mellitus, severe liver disease, or malignancies were excluded. All patients provided written informed consent for all of the surgical procedures performed. This study was approved by our Institutional Review Board, and patient informed consent for the study was not required as it was a retrospective review of medical records.
Surgery protocol
All surgeries were performed by the same senior orthopedic surgeon. Patients with cerebral trauma, thoracoabdominal trauma, or multiple injuries received general anaesthesia, and patients without these conditions received surgery under epidural anaesthesia. Debridement, including meticulous excision of local necrotic tissue, establishment of bone stability with single-sided external fixation with K-wires, and VAC were performed on all patients. Approximately 48–72 hours after the initial surgery, debridement was performed again to eliminate necrotic muscle, tendon, and fat, and detached ischemic bone. Haemostasis was achieved, followed by vacuum-assisted drainage. Cefazolin was used for antibiotic prophylaxis at the time of the primary intervention after tissue samples were collected for culture and sensitivity examination, and antibiotics were adjusted based on culture results. Subsequently, antibiotics were administered based on culture results. Further debridement followed by VAC was performed based on the appearance of the wound and bacterial culture results. Samples of wound excretions were sent for bacterial culture and antibiotic susceptibility testing prior to all additional debridements.
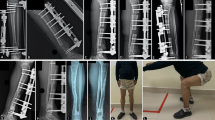
Once healthy granulation tissue was observed, and any infection controlled with antibiotics, all patients received open iliac bone autograft. Bone defects were packed to exceed the upper and lower fracture ends by 1 cm, and the wound cavity was fully filled with the bone particles. Vancomycin was added to the autograft in the case of infection. After haemostasis was achieved, post-operative negative-pressure VAC was maintained until the wound was covered with granulation tissue. If spontaneous epidermializaiton from the wound edge did not occur, split-thickness skin grafting was performed when the surface of the bone graft was completely covered by healthy granulation tissue. Intra-operative images of a representative case are shown in Fig. 1.
Case 12; a 47-year-old man with a severe open fracture of the tibia with segmental bone defect. a-c Debridement, external fixation of the bone fracture with K-wires, and vacuum-assisted closure were performed. d-f After 7 days, the bone defect was filled with iliac autograft bone. g Split-thickness skin grafting was performed 2 weeks after the initial surgery
Post-operative management
Antibiotics were administered based on bacterial culture results. As there is still controversy on whether prevention of thrombosis with low-molecular weight heparin (LMWH) may increase the wound exudation, it was not used. Instead, dextran-40 was administered (500 ml/day for 5 days) for the prevention of thrombosis. This was accompanied by functional exercise of the ankle and knee. During VAC, conventional dressing materials were changed every three days. Weight-bearing was allowed when a continuous callus was observed on radiographs. External fixation was removed after a visible callus and sufficient stability were achieved, and a brace was used until complete bone union had occurred.
Follow-up assessment
All patients were followed-up in the outpatient clinic. Data recorded included time to complete granulation tissue coverage, wound healing, and bone union, length of hospitalization, frequency of debridement, and number of deep tissue infections. The criteria for fracture union were no local tenderness or percussion pain, blurred fracture lines or the formation of a continuous callus, and the ability to walk three minutes without external fixation. Fracture radiographic union was defined as a bridging callus across three of four cortices on orthogonal radiographs evaluated by a research investigator, as previously described [14]. The Paley standard protocol was used to evaluate the outcomes of open bone fractures [15].
Data analysis
Continuous data were presented as mean ± standard deviations with range (minimum to maximum), and categorical data were presented as number (percentage).
Results
The study included 14 men and five women with a mean age of 38.47 ± 8.72 years (range, 25–57 years). All patients were seen in the emergency department within 24 hours of the injury, and all received surgery within 24 hours of admission to the emergency department. Injuries were due to traffic accidents (n = 7), crush (n = 8), and falls (n = 4), and 11 injuries were in the proximal tibia and eight in the distal tibia. Ten fractures were Orthopedic Trauma Association (OTA) classification 41-A3, one was 41-C3, seven were 43-A3, and one was 43-C3.
The mean bone defect length was 4.81 ± 1.25 cm (range, 2.5 to 7 cm), and the area of soft tissue defects ranged from 5 × 6 to 15 × 30 cm. The mean length of hospitalization was 11.0 ± 3.0 weeks (range, 7-18 weeks). Individual case data are presented in Tables 1 and 2, and summary data in Table 3.
Two patients were lost to follow-up, and the mean follow-up time for the 17 patients was 59.35 ± 8.76 months (range, 51-84 months). The mean time for full granulation tissue coverage was 15.41 ± 1.87 days (range, 14-21 days), and the mean time for complete wound healing was 7.76 ± 1.52 weeks (range, 6-11 weeks). Bone union was achieved at a mean time of 33.88 ± 8.37 weeks (range, 23-53 weeks). Only one patient (case 4) developed a deep tissue infection, and the organism was identified as Enterobacteria cloacae. The patient was treated with antibiotics, required two local debridements, and achieved complete bone union and healing of the wound. Patient 18 developed a pin tract infection, which resolved with local wound care and oral antibiotics. Based on Paley grade, five outcomes were excellent, eight were good, and four were fair. Follow-up images of a representative case are presented in Fig. 2.
Discussion
The results of this report with follow-up of five years indicate that a combination of the Papineau technique of open bone grafting and VAC can result in good outcomes for patients with severe open tibial fractures with bone and soft-tissue defects. Of the 19 patients studied, only one developed a deep tissue infection which was resolved with debridements and antibiotics. Based on Paley grade, five outcomes were excellent, eight were good, and four were fair. The advantage of this technique is the combined use of VAC and first stage bone grafting. VAC creates an environment that minimizes the possibility of infection, which is helpful for healing after bone grafting and also promotes the granulation tissue growth and wound healing. Compared with classic techniques (vascularized bone graft, bone transport, staged bone graft after wound closure), this technique is much simpler, easier to perform, and causes less tissue injury.
The three challenging problems with severe open tibial fractures are prevention of infection, bone union, and coverage of soft-tissue. Open bone grafting for the repair of infected bone defect can be divided into three stages: (1) complete debridement of all necrotic and infected tissue; (2) local wound care with dressing changes until complete coverage with granulation tissue; (3) bone grafting, and further local wound care until coverage with granulation tissue followed by skin grafting. The Papineau technique consists of two core procedures: complete debridement and reconstruction of bone stability with enough cancellous bone graft to fill the defect [6, 16, 17]. Compared with other methods for repair of bone defects, such as vascularized bone graft, bone transport, and staged bone graft after wound closure, the Papineau technique simplifies repair by avoiding coverage of the wound by flaps.
VAC is a relatively new method for facilitating wound healing [18]. In simplistic terms, a polyvinyl alcohol hydrated salt algae sponge dressing containing a drainage tube is used to cover the wound, and negative pressure is applied to seal the wound and remove exudates [18]. There are a number of advantages associated with VAC [11, 19, 20]. Unobstructed drainage reduces the aggregation of local exudates, and isolation of the wound reduces the possibility of infection. VAC promotes fibroblast proliferation through mechanical stress, consequently pushing the epithelium centrally and gradually shrinking the wound area, and facilitates microcirculation of the wound, which accelerates the growth of granulation tissue. Thus, suitable conditions for bone grafting are rapidly created. Compared with local wound care of dressing changes, the combination of open bone graft and VAC may solve the problem of protecting healing tissue and bone, and provide an improved technique in the cases of severe open tibial fractures.
A few other studies have described VAC and bone grafting for the treatment of tibial fractures. In 2006, Archdeacon and Messerschmitt [12] reported good outcomes from treating osteomyelitis of the tibia after open tibial fractures with debridement, Papineau bone grafting, and VAC. More recently, Karargyris et al. [13] reported the use of Papineau debridement, Ilizarov bone transport, and VAC for the treatment of septic bone defects of the tibia. Seven patients received single-stage extensive surgical debridement of necrotic bone, open bone grafting with cancellous bone autograft and bone transport, and postoperative negative-pressure wound care. The mean time from the initial injury was six months. Successful wound healing occurred at a mean of 29 days in all patients, and only one patient experienced delayed union, which was treated with autologous cancellous bone grafting. There were no recurrences of infection with a mean follow-up of 14 months. Six patients were able to return to their prior level of activity; one patient had a stiff ankle joint and because his job was strenuous he had to change work. Deng et al. [21] performed single-stage reconstruction with open bone grafting and VAC on 15 patients with infected tibial nonunion. All patients had sustained severe tibial fractures as a result of motor vehicle accidents, and had received primary treatment. The mean time from the onset of tibial infection was 9.1 months. Patients were follow-up up for an average of 22.6 months (range, 14-42 months). Bone union was achieved in 93.3% (14/15) of patients after a mean of 5.93 months (range, 3-10 months), and all wounds healed at an average of five weeks (range, 3-10 weeks). At the last follow-up, all patients considered the function and appearance of their limbs satisfactory.
Open tibial fractures are frequently characterized by heavy wound contamination, severe local soft tissue defects, and large amounts of necrotic tissue; treatment consists of repeated debridement until all necrotic tissue is removed, and the wound is completely covered by healthy granulation tissue [22,23,24]. Schlatterer et al. [18] recently reviewed the literature regarding the use of negative pressure wound therapy in the treatment of Gustilo-Anderson grade IIIB tibial fractures. The review conducted through September 1, 2013 identified one randomized controlled trial and 12 retrospective studies. While the individual study results were mixed, the evidence led the authors to conclude that negative pressure wound therapy is associated with lower infection rates than conventional wound care with gauze dressings. The results also suggested that negative pressure wound therapy beyond 72 hours is not associated with increased infection rates, and may be associated with a reduced necessity of treatment with flaps.
The results of this study with follow-up of five years suggest that VAC is useful for preventing further necrosis of the wound, allowing early bone grafting and improved healing. Application of the Papineau technique combined with VAC turns the open wound into an enclosed space, and thus helps to avoid further tissue necrosis. Furthermore, VAC ensures thorough drainage of the wound, promotes local blood supply, accelerates generation of granulation tissue, reduces the preparation time for bone grafting, and finally expedites healing of soft tissue. A feature of the traditional Papineau technique is open drainage with a wet/dry interface and regular dressing changes. However, this technique is reported to have a relatively high nosocomial infection rate [12, 25]. However, VAC isolates the wound and promotes healing, thus reducing the chance of infection. No nosocomial infections occurred in the 19 patients presented in this report, and there was only one case of deep tissue infection, which resolved promptly with debridement, antibiotics, and vacuum drainage.
The current study did not include a control group. While there is no standard widely accepted technique for the treatment of severe open tibial segmental bone defects, bone transport is the most commonly used strategy. Thus, we believe a comparison of our results with those of bone transport may be useful. Tong et al. [26] compared the Masquelet technique and Ilizarov bone transport for lower extremity bone defects following posttraumatic osteomyelitis. The Masquelet technique was associated with a shorter mean finite fixator time (10.15 months vs 17.21 months), and better functional outcomes [excellent (8 vs 3), good (9 vs 6), fair (3 vs 8) and poor (0 vs 2)] than bone transport, respectively. Bone outcomes, however, were similar between the Masquelet and Ilizarov groups [excellent (5 vs 7), good (10 vs 9), fair (4 vs 2) and poor (1 vs 1)], respectively. Sadek et al. [27] compared the results of two-stage reconstruction and Ilizarov ring external fixator in a single stage procedure for the management of resistant infected tibial diaphyseal nonunion with a gap. Time to union and the post-operative limb length discrepancy were not different between the groups. Patients that received two stage reconstruction had better preservation of the pre-operative range of motion of both ankle and subtalar joints, and had fewer complications and required fewer post-operative plastic reconstruction procedures than the patients that received the single stage surgery. Smith et al. [28] treated 11 patients with traumatic forearm bone loss with Ilizarov ring fixation and bone transport. The union rate of Ilizarov ring fixation and bone transport was 64%, with the other patients requiring compression plating. While nine patients described resulting function as excellent, three experienced marked limitations of wrist function.
No study is without limitations. The primary limitations of this study are the small number of patients and the retrospective analysis. As we have previously mentioned, the study design did not include a control group that received conventional care with which to compare the results. Randomized, prospective studies are required to validate the combined use of VAC and bone grafting for the treatment of open tibial fractures with bone and soft tissue defects.
Conclusions
The results of this retrospective review suggest that the combination of VAC and open bone grafting results in good outcome for patients with open tibial fractures and severe bone and soft-tissue defects.
References
Obremskey W, Molina C, Collinge C, Tornetta P 3rd, Sagi C, Schmidt A et al (2014) Current practice in the management of open fractures among Orthopaedic trauma surgeons. Part B: management of segmental long bone defects. A survey of Orthopaedic trauma association members. J Orthop Trauma 28:e203–e207. https://doi.org/10.1097/BOT.0000000000000034
Yazar S, Lin CH, Wei FC (2004) One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg 114:1457–1466
Koettstorfer J, Hofbauer M, Wozasek GE (2012) Successful limb salvage using the two-staged technique with internal fixation after osteodistraction in an effort to treat large segmental bone defects in the lower extremity. Arch Orthop Trauma Surg 132:1399–1405. https://doi.org/10.1007/s00402-012-1564-x
Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R et al (2014) Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury 45(Suppl 2):S3–S7. https://doi.org/10.1016/j.injury.2014.04.002
Papineau LJ (1973) Excision-graft with deliberately delayed closing in chronicos-teomyelitis. Nouv Press Med 2:2753–2775
Panda M, Ntungila N, Kalunda M, Hinsenkamp M (1988) Treatment of chronic osteomyelitis using the Papineau technique. Int Orthop 22:37–40
Tulner SA, Schaap GR, Strackee SD, Besselaar PP, Luitse JS, Marti RK (2004) Long-term results of multiple-stage treatment for posttraumatic osteomyelitis of the tibia. J Trauma 56:633–642
Stannard JP, Volgas DA, Stewart R, McGwin G Jr, Alonso JE (2009) Negative pressure wound therapy after severe open fractures: a prospective randomized study. J Orthop Trauma 23:552–557. https://doi.org/10.1097/BOT.0b013e3181a2e2b6
Braakenburg A, Obdeijn MC, Feitz R, van Rooij IA, van Griethuysen AJ, Klinkenbijl JH (2006) The clinical efficacy and cost effectiveness of the vacuum assisted closure technique in the management of acute and chronic wounds: a randomized controlled trial. Plast Reconstr Surg 118:390–397. https://doi.org/10.1097/01.prs.0000227675.63744.af
Vig S, Dowsett C, Berg L, Caravaggi C, Rome P, Birke-Sorensen H et al (2011) Evidence-based recommendations for the use of negative pressure wound therapy in chronic wounds: steps towards an international consensus. J Tissue Viability 20(Suppl 1):S1–S18. https://doi.org/10.1016/j.jtv.2011.07.002
Tan Y, Wang X, Li H, Zheng Q, Li J, Feng G, Pan Z (2011) The clinical efficacy of the vacuum-assisted closure therapy in the management of adult osteomyelitis. Arch Orthop Trauma Surg 131:255–259. https://doi.org/10.1007/s00402-010-1197-x
Archdeacon MT, Messerschmitt P (2006) Modern papineau technique with vacuum-assisted closure. J Orthop Trauma 2:134–137. https://doi.org/10.1097/01.bot.0000184147.82824.7c
Karargyris O, Polyzois VD, Karabinas P, Mavrogenis AF, Pneumaticos SG (2014) Papineau debridement, Ilizarov bone transport, and negative-pressure wound closure for septic bone defects of the tibia. Eur J Orthop Surg Traumatol 24:1013–1017. https://doi.org/10.1007/s00590-013-1279-x
Whelan DB, Bhandari M, MD MK, Guyatt GH, Kreder HJ, Stephen D, Schemitsch EH (2002) Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation. J Bone Joint Surg Br 1:15–18
Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R (1989) Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 241:146–165
Asomugha EU, Alexander IJ (2014) Papineau open cancellous bone grafting for chronic osteomyelitis and infected nonunions of the distal lower extremity. Tech Foot Ankle Surg 13:108–117. https://doi.org/10.1097/BTF.0000000000000033
Lei H, Yi L (1998) One-stage open cancellous bone grafting of infected fracture and nonunion. J Orthop Sci 3:318–323
Schlatterer DR, Hirschfeld AG, Webb LX (2015) Negative pressure wound therapy in grade IIIB tibial fractures: fewer infections and fewer flap procedures? Clin Orthop Relat Res 473:1802–1811
Bucalo B, Eaglstein WH, Falanga V (1993) Inhibition of cell proliferation by chronic wound fluid. Wound Repair Regen 3:181–186
Dedmond BT, Kortesis B, Punger K, Simpson J, Argenta J, Kulp B, Morykwas M, Webb LX (2007) The use of negative-pressure wound therapy (NPWT) in the temporary treatment of soft-tissue injuries associated with high-energy open tibial shaft fractures. J Orthop Trauma 21:11–17. https://doi.org/10.1097/BOT.0b013e31802cbc54
Deng Z, Cai L, Jin W, Ping A, Wei R (2014) One-stage reconstruction with open bone grafting and vacuum-assisted closure for infected tibial non-union. Arch Med Sci 10:764–772. https://doi.org/10.5114/aoms.2013.34411
Busse JW, Jacobs CL, Swiontkowski MF, Bosse MJ, Bhandari M, Evidence-Based Orthopaedic Trauma Working Group (2007) Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J Orthop Trauma 21:70–76. https://doi.org/10.1097/BOT.0b013e31802cbc43
Matos MA, Lima LG, de Oliveira LA (2015) Predisposing factors for early infection in patients with open fractures and proposal for a risk score. J Orthop Traumatol 16:195–201. https://doi.org/10.1007/s10195-015-0345-z
Gonzalez A, Suvà D, Dunkel N, Nicodème JD, Lomessy A, Lauper N, Rohner P, Hoffmeyer P, Uçkay I (2014) Are there clinical variables determining antibiotic prophylaxis-susceptible versus resistant infection in open fractures? Int Orthop 38:2323–2327. https://doi.org/10.1007/s00264-014-2395-x
Krug E, Berg L, Lee C, Hudson D, Birke-Sorensen H, Depoorter M et al (2011) Evidence-based recommendations for the use of negative pressure wound therapy in traumatic wounds and reconstructive surgery: steps towards an international consensus. Injury 42(Suppl 1):S1–S2. https://doi.org/10.1016/S0020-1383(11)00041-6
Tong K, Zhong Z, Peng Y, Lin C, Cao S, Yang Y et al (2017) Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury 48:1616–1622. https://doi.org/10.1016/j.injury.2017.03.042
Sadek AF, Laklok MA, Fouly EH, Elshafie M (2016) Two stage reconstruction versus bone transport in management of resistant infected tibial diaphyseal nonunion with a gap. Arch Orthop Trauma Surg 136:1233–1241. https://doi.org/10.1007/s00402-016-2523-8
Smith WR, Elbatrawy YA, Andreassen GS, Philips GC, Guerreschi F, Lovisetti L et al (2007) Treatment of traumatic forearm bone loss with Ilizarov ring fixation and bone transport. Int Orthop 31:165–170. https://doi.org/10.1007/s00264-006-0172-1
Acknowledgements
We thank the SciencePen group for their support in editing and proofreading the article.
Funding
This study is supported by the National Natural Science Foundation of China (General Program) [Grant No. 81572163] and the Wuhan Cultivation Program for Middle-aged and Young Medical Talents [Grant No. 2014–77].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure of potential conflicts of interest
All authors declare no conflicts of interest.
Research involving human participants
This study was approved by our Institutional Review Board, and patient informed consent for the study was not required as it was a retrospective review of medical records.
Rights and permissions
About this article
Cite this article
Bao, T., Han, F., Xu, F. et al. Papineau technique combined with vacuum-assisted closure for open tibial fractures: clinical outcomes at five years. International Orthopaedics (SICOT) 41, 2389–2396 (2017). https://doi.org/10.1007/s00264-017-3620-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3620-1