Abstract
Purpose
The linear penetration rate (LPR) has been used to estimate volumetric wear ever since metal-on-polyethylene bearings were first introduced. Annual volumetric wear and osteolysis are interrelated. The use of dual mobility cups has increased; however, the presence of two bearings needs paraclinical monitoring of wear to anticipate potential wear-related complications. Is LPR correlated to volumetric wear?
Methods
Ninety-eight dual mobility liner retrievals were mapped in three-dimensions (3D) with a fully automatic stripe light scanner. Martell’s method was applied to 3D maps of the explants to determine how much the centres of the inner and outer bearings had shifted in the three planes, and in particular, penetration of the femoral head in the “z” axis. The total, inner and outer wear volumes were then compared to the shift in the centres of rotation (COR) and the pre-operative X-rays.
Results
There was no relationship between wear and head penetration into the liner. There was a statistically significant relationship between the 3D centre of rotation shift and inner wear or total wear. Wear was multidirectional.
Conclusions
LPR is ineffective for estimating wear of dual mobility inserts, since its wear not two-dimensional. In the future, a 3D imaging method with very thin slices could be used to monitor the wear of dual mobility inserts by measuring the shift in the centres of rotation, once artifacts are overcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Background
Clinical follow-up for total hip replacement (THR) is essential, as it may help diagnose complications that are sub-clinical. This paraclinical monitoring must be non-invasive and cost effective, while maintaining a balance between risks and benefits. Dumbleton et al. [1] showed that a relationship exists between the annual wear of polyethylene liners and osteolysis. Wear of the metal-on-UHMWPE bearing in the Charnley prosthesis [2] was determined by measuring the linear penetration rate (LPR) [3]. The wear defined by Charnley was unidirectional [4], making use of polyethylene’s excellent composite properties. Although the wear is actually three-dimensional (3D), its unidirectional nature implies that it can be monitored with AP X-rays of the pelvis in a weight bearing patient. In this case, a two-dimensional parameter can be used to estimate a 3D value. The LPR is obtained by measuring the distance between the centre of the prosthetic head and the centre of the hemispheric cup. Several measurement methods have been described, from manual ones like Livermore’s method to Martell’s automated method, which is said to be the most accurate and reproducible. The software uses contrasting grey levels to determine the contours and to define circles. This wear analysis method was applied to the dual mobility THR [5–7] assuming that the two systems used the same bearing. To improve measurement accuracy, some teams have placed tantalum beads in the pelvis intra-operatively [8].
Rationale
Motion of the liner, which can cause multidirectional wear, and presence of two bearings and a retention collar, have led some researchers to question the applicability of this method. A 3D analysis of explanted components is the most reliable method for directly evaluating wear [9]. The 3D data describes the exact position of the centres of rotation (COR), making it possible to compare displacements and volumetric wear. The purpose of this study was to:
-
(1)
Evaluate the correlation between 3D COR displacement and volumetric wear, in particularly its penetration component (3D LPR)
-
(2)
Compare the 3D LPR and 3D COR displacement with X-ray LPR
Methods
This was a retrospective, exhaustive and continuous study of explants, designed as a case series. Components were explanted from 1990 to 2015 and formed a database of 500 explants. All implants were implanted from 1985 to 2014 and explanted in the same unit.
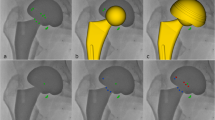
The 500+ dual mobility THA components explanted between 1990 and 2015 were examined. We selected 98 explants that best represented three phases in the history of dual mobility components: explants with more than 15 years in vivo use, explants from intra-prosthetic dislocations (IPD) and recent explants (i.e. components implanted after 2003, once the main changes to the design, materials and sterilisation method had been made). IPD is a rare but specific complication [10, 11] associated with dual mobility cups that occurs when the liner and prosthetic head separate. For each explant, we collected all of the clinical and material data, such as the diameter and material of the cup, prosthetic head and stem (Fig. 1).
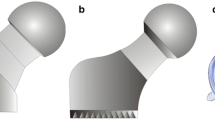
A Zfx Evolution stripe light scanner (Fig. 2) (ZFX-GMBH, Dachau, Germany) was used to generate a non-destructive 3D map of the explants. This device follows the VDI/VDE 2617 standard that validates the coordinate measuring machines. Its accuracy was defined as 9 μm. Only a few wear studies in the orthopaedic field have already been conducted [12], but its use in other fields [13, 14] allows to consider this technique reliable and accurate.
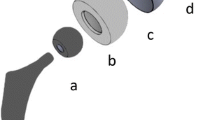
The total volume of the modelled explants was compared to the theoretical volume calculated from the original drawings of the liners. The total, inner and outer wear were determined by subtraction, taking into account manufacturing tolerances. As only liners with at least six years of functioning were measured, the manufacturing tolerances did not impact the validity of the measurements, being lower by at least an order of magnitude. The centre of the convexity is the centre of the outer bearing, while the centre of the concavity is the centre of the inner bearing. We defined a coordinate system [O; x,y,z] in which O is the initial centre of the concavity, x and y are the two horizontal dimensions on a slice of the liner, and z is the vertical dimension (Fig. 3). The reference axes were placed automatically on the 3D liner plan; the reconstructed centres of rotation of the explanted liner were determined with a multiple selection of points in the concave and convex zones, fitting virtual spheres.
We then carried out a second test of agreement between the actual values and the measured values by comparing the explant values to the data obtained on the X-rays. We measured the penetration of the head centre on an AP view of the pelvis using digital X-rays with the DICOMeasure™ software (ViewTec, Maisons Alfort, France). This software uses the Martell method to obtain LPR from the centres of the cup and the head. Thirty-two patients were randomly chosen to apply the method. Two independent investigators analysed the same radiographs (Fig. 4).
The x, y, z shifts were recorded along with the distance between the original centre (according to the drawings) and the centre measured on the explant. The position of the original centre helps us to avoid a bias in the displacement of the centre of the convexity due to asymmetric wear, which leads to a difference between the centre of the cup, measured on X-rays, and the centre of the convexity. The x, y displacements have no real meaning, given the lack of a reference position. The z dimension corresponds to femoral head penetration, hence the LPR value. We hypothesised that if LPR is a good wear estimation method, the wear is significantly correlated with penetration of the head centre, which is the z value of the centre’s shift. The real 3D COR shift was also measured, to compare it with the z value and the wear volumes. The shift in the centres on X-rays, representing the usual LPR, obtained via Martell method was then compared to the explant measurements.
The statistical analysis was performed with Minitab® 16 software (Minitab Inc., State College, Pennsylvania, USA). The Anderson-Darling test was used to determine if the data set was normally distributed. All tests were two-tailed. Comparisons between the various groups of quantitative variables were performed using Student’s t-test if they were normally distributed. If not, the non-parametric Mann–Whitney U and Kruskal-Wallis tests were used. The significance threshold was set at P < 0.05.
No human or animal was tested for this study, which was only based on anonymized explants or AP radiographs.
Results
The 3D models of the explants and the 3D drawings of the liners were compared to derive the volumetric wear measurements. Since the wear values were not normally distributed, the median value was used. The median total wear of the liners was 550 mm³ [346; 976]. The inner and outer wear were 276 mm³ [43; 449] and 347 mm³ [64; 852], respectively. Martell’s method was applied to the 3D drawings in order to compare the position of the centres of the concavity and convexity. The distance between the centre of the concavity and the centre of the convexity was measured, along with its components in the three planes. The resulting values were not normally distributed. The median of the z shift, which corresponds to a displacement in the base–apex axis of the liner, was 0 mm [−0.17; 0.10]. The x and y shifts were defined arbitrarily, since the liners had no fixed orientation in the plane perpendicular to the z axis, and could rotate freely in this plane. The x shift was −0.04 mm [−0.30; 0.26] and the y shift was −0.02 mm [−0.13; 0.10]. The distance between centres was defined as a value with no directionality. The resulting values were not normally distributed. The median of the distance between centres was 0.438 mm [0.28; 0.86]. We then sought to determine whether the centre shift values and wear were related. There was no statistically significant relationship between the z shift and liner wear. The x and y shifts were also not relevant. However, the distance between centres was significantly related to the total wear (P < 0.05) and inner wear (P < 0.001), but not the outer wear.
Each of the centre displacement values (x, y, z, and distance between centres) was compared to the LPR obtained on an AP view of the pelvis. The LPR was also not normally distributed. The median LPR was estimated at 0.1 mm [0; 0.6]. There was no statistical relationship between the LPR and the displacement in any of the three directions. In particular, there was no significant relationship (P > 0.4) between z displacement and LPR, or the distance between centres and LPR. The radiological penetration value was not significantly related to wear (P > 0.5).
Discussion
Finding simple ways of measuring wear is a crucial point in the follow up of metal-on-polyethylene THR. LPR is widely used for this purpose, due to its noninvasiveness and its precision when using Martell’s technique. Dual mobility wear evaluation with LPR had not been evaluated prior to this study. We compared wear data obtained by 3D scanning, head penetration measurements, center of rotation shifts and LPR measurements. There is no relationship between head penetration into a dual mobility liner and wear of the liner. On the contrary, the explanted components showed that liner wear can occur both in the direction of penetration and in the opposite direction, and that liner wear is truly three-dimensional. However, a shift in the CORs was found to be correlated significantly with wear, mainly with inner wear.
Our study has one bias that must be taken into account: we used explants, which by definition are failed components. These have more wear than the general population and may function differently. The 3D measurements were performed in a laboratory, without attempting to reproduce in vivo conditions, such as joint fluid, loading and temperature. Some authors have shown that loading can affect LPR values [4].
Our study does not provide answers about the transient linearity in the wear of the dual mobility prosthesis. While it has been shown on a walking simulator that implants made of conventional polyethylene undergo linear wear once the run-in phase has been completed [9, 15, 16], this has not been demonstrated with mobile liners. Since mobility is related to mechanical properties, we cannot be certain that they are maintained over time, particularly because of changes in the polyethylene’s oxidation. Explants, particularly in IPD cases [11, 17], have signs of delamination—mainly in the retaining collar—that suggests oxidation damage.
Lastly, the fact that there was no significant relationship between LPR and wear must not stop surgeons from being on alert when the head appears to have penetrated several millimetres in the cup—patients must continue to be monitored regularly. In addition, this study’s findings do not mean that regular X-ray follow-up is not necessary; these images are useful in determining the presence of radiolucent lines, osteolysis or even loosening [1, 2].
Conclusions
To conclude, standard analysis methods are not relevant for measuring wear of a dual mobility implant. Only the distance between centres of rotation was found to be correlated with wear, particularly inner bearing wear. A method still needs to be developed to estimate the shift in the COR of the two bearings in clinical practice. In addition to the exposure to ionising radiation induced by thin-slice CT scan, this modality has artifacts that must be eliminated to make it sufficiently accurate. Newer MRI units, although they are accurate and non-invasive, also have artifacts. It is important to have a paraclinical method that can be used in clinical practice to measure the wear of dual mobility implants, in order to diagnose at-risk patients. This non-invasive method could also be used in large patient populations over the long term to measure the effect of changes in design and materials made to this concept, which is now 40 years old.
References
Dumbleton JH, Manley MT, Edidin AA (2002) A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty 17:649–661
Devane PA, Horne JG, Martin K et al (1997) Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J Arthroplasty 12:256–266
Martell JM, Berdia S (1997) Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am 79:1635–1641
Martell JM, Leopold SS, Liu X (2000) The effect of joint loading on acetabular wear measurement in total hip arthroplasty. J Arthroplasty 15:512–518. doi:10.1054/arth.2000.4336
Boyer B, Philippot R, Geringer J, Farizon F (2012) Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 36:511–518. doi:10.1007/s00264-011-1289-4
Buford A, Goswami T (2004) Review of wear mechanisms in hip implants: paper I – general. Mater Des 25:385–393. doi:10.1016/j.matdes.2003.11.010
Farizon F, de Lavison R, Azoulai JJ, Bousquet G (1998) Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop 22:219–224
Pineau V, Lebel B, Gouzy S et al (2010) Dual mobility hip arthroplasty wear measurement: experimental accuracy assessment using radiostereometric analysis (RSA). Orthop Traumatol Surg Res 96(6):609–615. doi:10.1016/j.otsr.2010.04.007
Blunt L, Jiang XQ (2000) Three dimensional measurement of the surface topography of ceramic and metallic orthopaedic joint prostheses. J Mater Sci Mater Med 11:235–246
Lecuire F, Benareau I, Rubini J, Basso M (2004) Intra-prosthetic dislocation of the Bousquet dual mobility socket. Rev Chir Orthopédique Réparatrice Appar Mot 90:249–255
Philippot R, Boyer B, Farizon F (2013) Intraprosthetic dislocation: a specific complication of the dual-mobility system. Clin Orthop 471(3):965–970. doi:10.1007/s11999-012-2639-2
Boyer B, Neri T, Geringer J et al (2016) Understanding wear in dual mobility total hip replacement: first generation explant wear patterns. Int Orthop. doi:10.1007/s00264-016-3362-5
Gomes PF, Sesselmann M, Faria CDCM et al (2010) Measurement of scapular kinematics with the moiré fringe projection technique. J Biomech 43:1215–1219. doi:10.1016/j.jbiomech.2009.12.015
Jiang C, Jia S, Xu Y et al (2015) The application of multi-frequency fringe projection profilometry on the measurement of biological tissues. Biomed Mater Eng 26(Suppl 1):S395–S403. doi:10.3233/BME-151328
Affatato S, Spinelli M, Zavalloni M et al (2008) Tribology and total hip joint replacement: current concepts in mechanical simulation. Med Eng Phys 30:1305–1317. doi:10.1016/j.medengphy.2008.07.006
Charnley J, Kamangar A, Longfield MD (1969) The optimum size of prosthetic heads in relation to the wear of plastic sockets in total replacement of the hip. Med Biol Eng 7:31–39
Geringer J, Boyer B, Farizon F (2011) Understanding the dual mobility concept for total hip arthroplasty. Investigations on a multiscale analysis-highlighting the role of arthrofibrosis. Wear 271:2379–2385. doi:10.1016/j.wear.2011.02.027
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bertrand Boyer was a consultant for SERF (Décines, France).
Thomas Neri is a consultant for SERF (Décines, France).
Rémi Philippot and Frédéric Farizon receive royalties from SERF (Décines, France).
Alexandre Di Iorio and Jean Geringer have no conflict of interest concerning this study.
Ethical review committee statement
As this study involves only implant retrieval, anonymously collected, the Ethical Review Committee approval was not required for this study, according to the Ethical Review Committee from our institution.
Funding
No funding was necessary for this study.
Rights and permissions
About this article
Cite this article
Boyer, B., Neri, T., Di Iorio, A. et al. The linear penetration rate is not relevant for evaluating wear of dual mobility cups: an explant study. International Orthopaedics (SICOT) 41, 599–603 (2017). https://doi.org/10.1007/s00264-017-3406-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3406-5