Abstract
Purpose
The medial plica (MP) is a normal anatomic structure consisting of a fold in the synovial layer of the joint. Arthroscopic resection is currently used as a gold standard procedure in patients with medial plica syndrome (MPS), but there are few prospective studies that analyze the long-term functional outcomes of plica resection.
Methods
The purpose of this prospective study was to evaluate the long-term results of arthroscopic resection of the medial plicae of the knee. Between 1999 and 2014 we included 267 patients that showed MRI evidence of MP out of the 5682 knee arthroscopies that we performed. We recorded pre and post-operative Tegner Lysholm knee scale scores (TLKSS) for up to 36 (3, 6, 12, 24, 36) months. The EQ-5D questionnaire was used to measure the patients’ generic health status.
Results
The mean values of the TLKSS were 68 (61–82) pre-operative, 87 (81–94) at the 3-month follow-up and 94 (92–97) at the 6-month follow-up. The long term results (TLKSS at 12, 24, and 36 months post-operatively) were 94.8 (91–98), 94.8 (90–97), and 94.5 (92–97) respectively. The EQ-5D and EQ-VAS showed significant improvement between each of the first three data registering moments (pre-operative, 3 and 6 month follow-up).
Conclusion
The quality of the treatment and the final functional result is directly influenced by the type of plica that creates the symptomatology. We have achieved good overall results for our patients, the ones with less cartilage damage having the fastest recovery time. The arthroscopic resection is a very good option for medial plicae that do not respond to conservative treatment, and it must be initiated as a first option when cartilage damage is suspected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
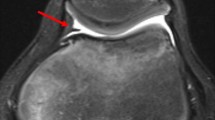
Medial knee pain is one of the pain syndromes most often encountered in patients with knee problems. This can be associated with a wide variety of knee pathologies such as a torn medial meniscus, inflammation, osteoarthritis (OA) of the knee or a medial plica. The medial plica (MP) is a normal anatomic structure consisting of a fold in the synovial layer of the joint (Fig. 1). It usually stretches out from the medial proximal part of the joint up until the infra-patellar fat pad (Hoffa pad). Its etiology is thought to date back to being a remnant of the fetal knee’s development [1]. Essentially, plicae are remnants of the compartment-separating membranes that have not been reabsorbed. The medial plica is the most common of all plicae, being present in autopsies in one out of every three or four knees [1], reported incidence rates range from 22 to 72 % [2, 3].
The pain mechanism in the medial plica syndrome (MPS) is often caused by a femoral condyle impingement during the flexion of the knee. This impingement causes irritation, thus creating an inflammatory reaction inside the knee, also known as the pathological synovial plica syndrome (PSPS). This repetitive impingement of the plica causes it to change its structure, becoming thicker and losing its elasticity [4]. MPS can often be found in young athletes that tend to overuse their joints, thus causing an inflammation in the medial compartment of the knee [5]. The diagnosis of MPS can be a rather difficult one due to the lack of symptom specificity. One of the first complaints of the patient is a “clacking” noise that often accompanies knee flexion. Some clinical tests have been described for MPS diagnosis but their sensitivity is rather low in the hands of a non-experienced specialist [6, 7].
Magnetic resonance imaging (MRI) is the most common method of imagistic diagnosis regarding internal knee structures. Plicae appear as bands on MRI, having low signal intensity in contrast with the joint fluid which has high signal intensity. The most valuable MRI protocols for visualizing plicae are the fat-suppressed T2-weighted and the T2-weighted images. In order to evaluate the clinical significance of a plica, the specialist must correlate its existence with other associated pathologies such as synovitis or cartilage damage and an increased plica in size. For special cases when patients lack synovial fluid, an MR arthrography may be performed. Joint distension and joint surface highlighting are induced by the contrast agent, which allows for an adequate visualization of the plica. Sakakibara performed an arthroscopic study in 1974 concerning the MP, and he classified them into four types regarding their size [8]. This classification has an important clinical significance because types A and B are considered to have a low chance of rendering pain, while types C and D, which are larger in size can often cause impingement on the medial condyle.
Arthroscopic resection is currently used as a gold standard procedure in patients with MPS, but there are few prospective studies that analyze the long-term functional outcomes of plica resection. The relatively low incidence of this pathology and the high chance of misdiagnosis have made it very hard to properly design and complete a good study regarding MP resection. The reliability of arthroscopic resection has been studied by some authors, but most of the publications are out-dated and did not allow for such a long-term follow up [9, 10].
Materials and methods
The purpose of this prospective study was to evaluate the long-term results of arthroscopic resection of the medial plicae of the knee. Between 1999 and 2014 we included 267 patients that showed MRI evidence of MP out of the 5682 knee arthroscopies that we performed. All procedures performed in this study were in accordance with the ethical standards of the SCJU Pius Brânzeu Research Committee and with the 1964 Helsinki declaration and its later amendments. For this retrospective study formal consent was not required. We excluded patients with concomitant procedures involving the menisci or cartilage (67 patients). All of the arthroscopies were performed by the same surgeon, with the patient in supine position and the knee flexed at 90° with an inflated tourniquet, as well as standard anteromedial and anterolateral portals being used.
We recorded age, gender, sport activity, laterality, period from start of symptoms until surgery, type of plicae (Sakakibara classification), cartilage degeneration (according to the modified Outerbridge classification), pre and post-operative Tegner Lysholm knee scale scores (TLKSS) for up to 36 (3, 6, 12, 24, 36) months. All patients complained of chronic knee pain that had not been relieved by non-steroidal anti-inflammatory drugs and benefited from quadriceps exercises for at least three months before operation. The level of sport activity was a subjective parameter and the patients chose between “n” (no type of sport), “o” (occasional sport activities), “m” (moderate sport activities), and “p” (professional sporting activities). The EQ-5D questionnaire was used to measure the patients’ generic health status. This included a description part made up of five different topics (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) with a 1 to 3 grading, 1 meaning no problems and 3 meaning extreme problems regarding the issue in case, and another part which allowed the patients to approximate their overall health status by using the visual analogue scale (EQ-VAS). Arthroscopic resection with the shaver was performed in all patients. The arthroscopic resection was performed either with a punch, a shaver or cauterization. Statistical evaluation of Lysholm knee scores was done using the paired t-test.
Results
Our mean age range was 28.2 (15–58) years old, our gender distribution was 92 males to 108 females, and our sport activity levels were n (25), o (86), m (65), p (24). The mean time from symptom onset to surgery was 12.8 (8–18) months and the mean post-operative follow-up period was 10.6 (6–36) months. The arthroscopic staging of our plicae according to the Sakakibara classification was type A – 3 (1.5 %) patients, B – 28 (14 %) patients, C – 105 (52.5 %) patients and D – 64 (32 %) patients. The cartilage quality of the medial condyle as seen during arthroscopy was 0 – 28 (14 %) patients, I – 120 (60 %) patients, II – 41 (20.5 %) patients and III – 11 (5.5 %) patients, according to the modified Outerbridge classification (Table 1).
The mean values and the standard deviations (sd) of the TLKSS were 68 (61–82, sd-4.42) pre-operative, 87 (81–94, sd-3.73) at the three month follow-up and 94 (92–97, sd-1.88) at the six month follow-up (Table 2). The EQ-5D results were displayed as a number made up from five figures (from 1 to 3), each of them corresponding to the appropriate parameter (e.g., 12231, 33212), and the results were organized in frequencies of reported problems out of all 200 patients regarding each of the five items. The EQ-VAS showed significant improvement between the first three data registering moments (pre-operative, 3 and 6 month follow-up), as seen in Table 2, and almost no improvement past the six month follow-up.
The most significant difference between pre-op and post-op parameters was registered at the first follow-up (at 3 months) when we saw a 19 point (approx. 28 %) increase in mean TLKSS values and a 16.6 point (approx. 23 %) increase in mean EQ-VAS. The next visit showed an 8 % increase in mean TLKSS values and a 5.9 % increase in mean EQ-VAS scores (Table 2). The drop-out rate was higher in patients with better functional scores and they mostly overlapped with type A and B plicae and grade 0 and I cartilage damage. Patients that showed a slower recovery pace were the ones that attended the 12, 24, and 36 month follow-up visits, including all of the patients that were professional athletes (sport level “p”). The long-term follow up meetings (12, 24, and 36 months) did not show further significant improvement when compared to the six month follow-up. The mean TLKSS and EQ-VAS values for those visits were 94.8 (91–98, sd-1.99) and 94.6 (90–96, sd-1.93) after 12 months, 94.8 (90–97, sd-2.02) and 94.9 (92–96, sd-1.49) after 24 months, and 94.5 (92–97, sd-1.81) and 94.2 (92–96, sd-1.52) after 36 months.
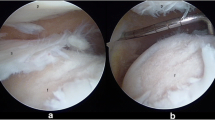
Regarding the surgical procedure, the plica resection was executed either by using a punch, a shaver or cauterization (Fig. 2). Either way, the duration of the procedure was recorded between 15 and 25 minutes with a mean duration of 18 minutes. All of the patients were discharged the next day and received indication for anti-inflammatory treatment for seven days. The sutures were removed after ten days from surgery and patients started the active recovery protocol 14 days after surgery. We had eight patients which reported contralateral MPS within the study period, but the secondary knee was not included in our data.
Discussion
The medial plicae are encountered in a high number (64–84 %) of normal knees, as reported by Dandy et al. [11], although it seems that most of the painful symptomatology (84.5 % of patients) is given by the type C and D plicae. Type A and B rarely create pain, and even when they do, the response to conservative treatment and physiotherapy is much better than type C and D plicae. Physical exercises that strengthen the hamstrings and quadriceps muscles have been proven to show benefits in MPS patients [12, 13].
The data we collected showed that we achieved better results in patients with a younger age, better cartilage status, and type A and B plicae. These findings are in concordance with the current state of literature, which shows significantly lower results in patients with cartilage damage ICRS 2 or higher [14]. However, literature also tells us that the success of plicae resection in MPS patients is also directly influenced by any other additional intra-articular pathology [15], which our study excluded. This may have a direct influence on the good results we found, compared to other studies regarding the MPS.
The time from pain onset until surgery was determined by the intensity of the clinical symptoms. When we reviewed our data we came to the conclusion that patients with A, B, and some C type plicae had a longer period of time until surgical treatment was recommended, while type D and some type C plicae patients had a shorter waiting time. So depending on the plicae type we can elaborate on the symptomatology and degree of cartilage damage, as well as compliance level to conservative ways of treatment. Prolonged impingement of a large and stiff type D plicae can cause fast and relatively high condral damage on the anteromedial aspect of the femur, together with articular effusion, inducing intense symptomatology.
If left untreated, the MPS can cause localized grade IV Outerbridge lesions, which are very hard to treat subsequently. This is why chronic knee pain must be looked into carefully especially when there is no obvious clinical finding such as in meniscal lesions. Medial plicae must be identified and properly graded as soon as possible in order to allow a favorable treatment with as few lesions as possible to the joint cartilage. Studies regarding MRI sensitivity (77–93 %) and specificity (58–81 %) in detecting MP are somewhat contradictory and suggest that the imagistic diagnosis is highly dependent on the radiologist and not on the investigation or the lesion itself [16, 17].
Conclusion
The quality of the treatment and the final functional result is directly influenced by the type of plica that creates the symptomatology. We have achieved good overall results for our patients, the ones with less cartilage damage having the fastest recovery time. When it comes to type C and D plicae the problem must be identified as soon as possible in order to prevent advanced cartilage destruction. Good and hasty TLKSS and VAS values improvement were observed especially in the first three months after the surgery. Our results indicated that the long term follow-up visits showed functional values similar to the three and six month check-ups. The arthroscopic resection is a very good option for medial plicae that do not respond to conservative treatment, and it should be initiated as a first option when cartilage damage is suspected. We believe that a latter multi-centered study with control groups would have an even bigger impact regarding this topic.
References
Dupont JY (1997) Synovial plicae of the knee. Controversies and review. Clin Sports Med 16:87–122
Kim SJ, Choe WS (1997) Arthroscopic findings of the synovial plicae of the knee. Arthroscopy 13(1):33–41
Jackson RW, Marshall DJ, Fujisawa Y (1982) The pathologic medial shelf. Orthop Clin N Am 13(2):307–312
Nigam A, Shetty V (2012) The medial plica: a clinical perspective. Eur J Orthop Surg Traumatol 22:97–102
Blok A, Weiss W, Dolata T, Szczepaniec M (2005) Medial synovial plica. Ortop Traumatol Rehabil 7:397–400
Pipkin G (1971) Knee injury: the role of the suprapatellar plica and suprapatellar bursa in simulating internal derangements. Clin Orthop 74:161–176
Kim SJ, Jeong JH, Cheon YM, Ryu SW (2004) MPP test in the diagnosis of medial patellar plica syndrome. Arthroscopy 20(10):1101–1103
Sakakibara J (1974) Arthroscopic study on Iino’s band (plica synovialis mediopatellaris). J Jpn Orthop Assoc 50:513–522
Hardaker WT, Whipple TL, Bassett FH 3rd (1980) Diagnosis and treatment of the plica syndrome of the knee. J Bone Joint Surg Am 62:221–225
Flanagan JP, Trakru S, Meyer M, Mullaji AB, Krappel F (1994) Arthroscopic excision of symptomatic medial plica. A study of 118 knees with 1–4 year follow-up. Acta Orthop Scand 65:408–411
Dandy DJ (1990) Anatomy of the medial suprapatellar plica and medial synovial shelf. Arthroscopy 6(2):79–85
Fulkerson JP (2002) Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med 30(3):447–456
Amatuzzi MM, Fazzi A, Varella MH (1990) Pathologic synovial plica of the knee. Results of conservative treatment. Am J Sports Med 18(5):466–469
Kan H, Arai Y, Nakagawa S, Inoue H, Hara K, Minami G, Inoue A, Kanamura H, Ikoma K, Fujiwara H, Kubo T (2015) Characteristics of medial plica syndrome complicated with cartilage damage. Int Orthop 39(12):2489–2494
Schindler OS (2014) The Sneaky Plica’ revisited: morphology pathophysiology and treatment of synovial plicae of the knee. Knee Surg Sports Traumatol Arthrosc 22(2):247–262
Stubbings N, Smith T (2014) Diagnostic test accuracy of clinical and radiological assessments for medial patella plica syndrome: a systematic review and meta-analysis. Knee 21(2):486–490
Nakanishi K, Inoue M, Ishida T, Murakami T, Tsuda K, Ikezoe J, Nakamura H (1996) MR evaluation of mediopatellar plica. Acta Radiol 37(4):567–571
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Radu Prejbeanu, Dan V. Poenaru, Andrei Dan Balanescu, and Mihail-Lazar Mioc declare that they have no conflicts of interest.
Funding
There is no funding source.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the SCJU Pius Brânzeu Research Committee and with the 1964 Helsinki declaration and its later amendments.
Rights and permissions
About this article
Cite this article
Prejbeanu, R., Poenaru, D.V., Balanescu, A.D. et al. Long term results after arthroscopic resection of medial plicae of the knee—a prospective study. International Orthopaedics (SICOT) 41, 121–125 (2017). https://doi.org/10.1007/s00264-016-3313-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3313-1