Abstract
Purpose
A correlation between soft tissue thickness and osteoporosis has been suggested. We aimed to estimate if a low body mass index (BMI) and/or a decrease of skin thickness could estimate the risk of contra-lateral hip fracture.
Methods
First, we performed a retrospective analysis of 1268 patients treated for a hip fracture. The 146 patients who had a contra-lateral hip fractures—study group—were compared with the 1078 patients who did not—control group. Four BMI categories were considered: obese, overweight, normal weight and low weight. Second, we enrolled prospectively 1000 consecutive patients in the emergency department. History of fractures, BMI, and skin aspect on the dorsum of both hands—classified as severe decrease thickness, moderate decrease thickness or normal—were recorded.
Results
pt?>In the first part, we found that patients with contra-lateral fractures had a significantly lower BMI than those in the control group (22.2 Vs 26.5 kg/m2, p = 0.01). In the second part, 48 on 1000 patients had a hip fracture. Among them, six had a contra-lateral fracture. BMI was 23.4 kg/m2 in bilateral hip fractures, 33.68 kg/m2 in the unilateral fracture group, and 28.04 kg/m2 in the non-fracture group (p = 0.04). Finally, patients with contra-lateral hip fractures had a severe decrease thickness of the skin.
Conclusion
A low BMI and a decreased skin thickness increase independently the risk of fractures by three times. When associated, they increase the risk of fracture risk by five times. This combination had a sensitivity at 71 % and a specificity at 90 % for predicting hip fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A contra-lateral hip fracture occurs in a patient who had previously sustained a hip fracture on the opposite side. It is an emerging problem in industrialized countries because of the progressive aging of the population. In fact, the incidence of contra-lateral hip fractures may be between 2 % at 18 months for the lowest estimation and 20 % at one year for the highest [1–6]. Given that the annual incidence of hip fractures in Europe is estimated around 250,000 per year, contra-lateral hip fractures could represent 25,000 patients each year [3].
For a first hip fracture, several risk factors have been suggested: gender, age, familial or personal history of fractures, alcohol intake, tobacco use and medications such as glucocorticoids for instance [7]. However, no risk factors that could predict subsequent contra-lateral hip fracture have been identified so far. In fact, Michelotti et al. failed to find a correlation between the anatomical aspect of proximal femur and a subsequent contra-lateral hip fracture [8]. Finally, bone mineral density (BMD) has been used to select the patients who were believed to have a higher risk of contra-lateral hip fracture [9]. However, the feasibility of a dual X-ray absorptiometry (DXA) remains questionable when the patient has a hip fracture that is not surgically fixed yet. Therefore, improving the estimation of the risk of contra-lateral hip fracture is still needed in order to select the patients at greater risk.
For some authors, obesity could provide a protection against fractures. However, the mechanisms for such an observation remain poorly understood. The different hypotheses include the role of adipose tissue in producing oestrogen, the role of the weight in increasing the mechanical stimulation of the bones and the bone remodeling, and the role of the thickness of the soft tissues around the hip that could cushion the hip in case of a fall. On the another hand, a low weight may be an indicator of debilitated health, which is a risk factor for falls and fractures. In fact, the decreased protection for hip fracture due to the decrease of soft tissue thickness may be related to a chronological alteration of several tissues that may overlap [10]. For all these reasons, measurement of skin and soft tissue thicknesses have been proposed as a method of predicting low bone BMD and the subsequent risk of osteoporotic fracture in post-menopausal women [11–17].
Therefore, we hypothesized that low BMI, soft tissue thickness and skin thickness could be correlated with a higher risk of contra-lateral hip fracture. To test that hypothesis, we designed a sequential study 1) first, we analyzed retrospectively all the patients hospitalized in our department between January 2008 and December 2013 for an osteoporotic hip fracture and compared those with a unilateral hip fracture to those with a contra-lateral one; 2) then, we enrolled prospectively 1000 consecutive patients from the emergency department and compared their history of fracture to BMI, the soft tissue thickness and skin thickness.
Material and methods
General setting
We conducted a sequential study. The first part of the study was a retrospective analysis of all the patients treated in our department for a unilateral hip fracture between January 2008 and December 2013. The second part of the study was a prospective study on consecutive 1000 patients who attended the emergency department since January 2014.
Retrospective analysis (contra-lateral hip fracture and BMI)
The first part of the study was a retrospective analysis of all the patients treated in our department for a unilateral hip fracture between January 2008 and December 2013. Inclusion criteria were every patient older than 50 years who sustained a hip fracture from a simple fall from his height. Exclusion criteria were a patient with a suspicion of pathologic fracture (history of neoplasia or radiographic aspect compatible with a neoplastic fracture) or with medical history and/or medications and/or habits competing with bone metabolism (rheumatoid arthritis, long-term corticotherapy, tobacco use, alcohol intake > 3 units/day) [18].
With these criteria, 1268 patients were included in the study. Among them, 146 patients (11.5 %) presented bilateral hip fractures: 54 patients had already had a previous contra-lateral hip fracture before the actual fracture occurring between January 2008 and December 2013, and 88 patients had both fractures during the inclusion dates. The mean age of these patients was 81.1 years (range, 65–96 years) and 74.7 % of them were female while 25.3 % were male. The mean time elapsed between the two fractures was 3.8 years (range, 1–203 months). Approximately 14 % of the contra-lateral fractures occurred in the first year after the first fracture and 35 % in the two years following the first fracture.
Finally, the 146 patients who had bilateral fractures—study group—were compared with the 1078 patients who did not have bilateral fractures—control group. Weight and height were obtained from the medical charts and BMI was obtained by dividing weight (in kilograms) by squared height (in meters2). All the patients were classified in four categories of BMI: obese (BMI > 30 kg/m 2); overweight (BMI between 25–30 kg/m 2); normal weight (BMI between 18.5–25 kg/m 2); and low weight (BMI <18.5 kg/m 2).
Prospective analysis (BMI, soft tissue, skin, and fractures)
The second part of the study was a prospective study on every patient admitted in the emergency department for a trauma related to a fall from a height since January 2014. The inclusion and exclusion criteria were the same as that for the retrospective study.
We decided to include the first 1000 patients who met the inclusion/exclusion criteria. Then, the patients were matched with the patients of the first part of the study for age—within a five years range—and gender. Then, we recorded the medical history of each patient based on the patients’ declarations and/or from patients’ medical charts concerning all the fractures they sustained.
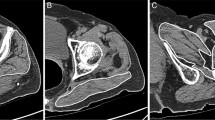
Then, the BMI of these patients was evaluated and we recorded whether these patients were hospitalized for hip fractures or had a previous hip fracture. Concomitantly, skin thickness of the included patients was assessed. A picture of the skin on the dorsum of the hand was taken for every patient. From this picture, the skin aspect was classified as severe decrease thickness, moderate decrease thickness, or normal. For the 30 first patients, the skin thickness was also assessed using a pachymeter as previously described [11]. From these first 30 patients, we correlated the classification derived from the picture to the actual measure of skin thickness. Then, we determined the inter-observer variability—accuracy—and the intra-observer variability—reliability—done by ten different examiners during three different sessions. We found that the skin thickness score was as reliable as the pachymeter technique. The assessment of skin thickness from the picture of the skin of the dorsum of the hand was therefore considered as sufficiently reproducible to be included as a measure (Fig 1, 2 and 3).
Statistical analysis
Data were analyzed with tables, graphs, and descriptive statistics. Chi-square test was used to research any significant association among the qualitative variables between the study group and the control group. Student’s t test was used to compare quantitative variables as mean age, height, weight, and BMI between the study group and the control group. The significance level taken was 5 %. Finally, we analyzed these variables as risks factors for a subsequent contra-lateral hip fracture with multivariate and logistic regression analyses.
Ethical statement
This study has been approved by our ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
Retrospective analysis (contra-lateral hip fracture and BMI)
We found that patients in the contra-lateral hip fracture group had a significantly lower BMI than those in the control group (22.2 Vs 26.5 kg/m2, p = 0.01). In fact, 15 % of the patients in the contra-lateral hip fracture group had a low weight, 62 % had a normal weight, 22 % were overweight, and 1 % were obese. On the contrary, only 3 % of the patients in the control group had a low weight, 54 % had a normal weight, 34 % were overweight, and 9 % were obese. Furthermore, we found that the difference was greater for weight than for height between the two groups. In fact, we found that the patients in the contra-lateral hip fracture group had a significantly lighter weight than those in the control group (respectively 65 kg, range 54–92 Vs 79 kg, range 64–128, p = 0.02). However, the difference was less important for height (mean 1.72 m, range 1.58-1.86, versus 1.73 m, range 1.61-1.85, p = 0.21). Finally, we found no significant differences in terms of age and gender between the two groups.
Prospective analysis (BMI, soft tissue, skin, and fractures)
Among the 1000 patients included in the prospective part of the study, mean age was 80,2 (64–95) years, 73.2 % of them were female while 26.8 % were male, and mean BMI was 30 (23–41) kg/m2. One hundred and thirty two patients had a previous fracture: 48 patients had a previous hip fracture and 84 patients had another type of fractures (radius, proximal humerus, pubic pelvic bone, etc.). Among the 48 patients who had a hip fractures, six had had a contra-lateral hip fracture.
Among the 1000 patients included in the study, 39 % were obese (BMI ≥30 kg/m2). The fracture prevalence among the obese patients was 1.12 % versus 2.07 % in the non-obese patients. The prevalence of obesity among the patients with fractures was 20.3 % versus 40.73 % among the patients without any fracture. Among the patients that presented at least one hip fracture, the BMI was 33.68 kg/m2 among the patients with only one hip fracture and 23.4 kg/m2 among the patients with contra-lateral hip fractures. For instance, BMI was 28.04 kg/m2 among the patients who did not have any fracture (p = 0.04). Among the patients who did not have any fracture, 4 % had a low weight, 72 % a normal weight, 15 % were overweight, and 9 % were obese. Among the 48 patients who had a hip fracture, 14 (29 %) had a low weight, 24 (50 %) a normal weight, eight (17 %) were overweight, and two (4 %) were obese. Among the six patients who had a contra-lateral hip fractures, four had low weight and two had a normal weight.
Among the patients without any fracture, 3 % had a severe decrease thickness on the dorsum of the hand, 12 % a moderate decrease thickness, and 85 % a normal thickness. Among the 48 patients who had a hip fracture, 16 (33 %) had a severe decrease thickness on the dorsum of the hand, 18 (29 %) a moderate decrease thickness, and 14 (28 %) a normal thickness. All six patients with a contra-lateral hip fracture had a severe decrease thickness of the skin.
Finally, we found a significant correlation between low skin thickness and low BMI (p <0.01). Both low BMI and decrease of skin thickness were found to increase the risk of hip fracture by three times. Moreover, when a low BMI and a severe decrease of skin thickness were associated, the risk of hip fracture was increased by five times. This combination of risk factors showed sensitivity of 71 % and specificity of 90 % for hip fracture.
Discussion
A contra-lateral hip fracture occurs in a patient who had previously sustained a hip fracture on the opposite side. It is an emerging problem in industrialized countries because of the progressive aging of the population. For some authors, low BMI, soft tissue thickness and skin thickness could be correlated with a higher risk of contra-lateral hip fracture. Our study confirmed the importance of contra-lateral hip fractures because we found that its overall incidence was 11.5 %. Furthermore, a multivariate analysis of several clinical factors found that a BMI < 22 kg/m2 was a statistically significant risk factor for contra-lateral hip fractures. To the best of our knowledge, only one other study analyzed BMI as a risk factor for the contra-lateral hip fracture but in a Korean population. In fact, Haeng Lee et al. studied the incidence of contra-lateral hip fractures in Korea and found that 233 of 2546 patients (9.2 %) had a contra-lateral hip fracture. Furthermore, they found that the risk factor of the subsequent contra-lateral hip fracture was a low BMI.
It is well known that body weight is influenced by many factors such as nutritional, hormonal, and environmental for instance. However, BMI has been related only recently to bone mineral density: an increased body weight and/or BMI could be correlated with an increased BMD [19]. On the other hand, low body weight and/or BMI may be correlated with a higher risk of hip fracture. The exact explanation of this association is unknown and some suggested a mechanical effect of the soft tissues during a traumatic impact. In fact, Tang and al. suggested that individuals with a greater fat mass may benefit from cushioning of their hip by adipose tissue, which could reduce the impact forces when they fall [20]. Furthermore, a decrease of trochanteric soft tissue thickness may be correlated to an increased risk of hip fracture. In fact, Bouxsein et al. assessed 63 postmenopausal women from the OFELY cohort (21 hip fractures and 42 controls) and they found that the patients with a decrease of trochanteric soft tissue thickness had more hip fractures [21].
Because both skin and bone are mainly comprised of type 1 collagen, some authors suggested that a decrease thickness of the skin—both the dermal and subcutis parts—could be correlated with osteoporosis. In fact, Patel et al. reported that patients with osteoporotic fractures had a reduced skin thickness when measured by ultrasound. Hence, they suggested that skin thickness could help in discriminating patients at higher risk for osteoporotic hip fracture [13]. In another study Yoneda et al. found that osteoporosis is inversely related to the thickness of the skin on the back of the hands [11]. Our study confirms this phenomenon, even if the evaluation, based on a visual scale analysis of the thickness of the skin, was simple.
On the other hand, Black et al. assessed the effect of stretching of the skin on its collagen content and its thickness in a group of patients with chronic obesity [22]. They found that despite an increase of skin surface in obesity, the thickness of the skin and the content of collagen were maintained. They concluded that skin stretching secondary to a prolonged obesity leads to a collagen hypertrophy that maintains skin thickness [22]. Finally, BMI and skin thickness measurements might be considered as a non-invasive method of evaluating risk of a contra-lateral fracture in osteoporotic patients, and may help to identify cases requiring preventive treatment on the contra-lateral side [11].
We acknowledge several limitations to our study. First, the clinical assessment of skin thickness was performed with a visual scale analysis. Other methods have been used such as the Rodnan score obtained by clinical palpation, a pachymeter or an echography. Second, despite a large number of patients included in the retrospective or prospective parts of our study, only a few contra-lateral hip fractures occurred during the period of observation. Third, we assessed only two risk factors of hip fractures in our study, which reduces the influence of random variation but does not take into consideration other risk factors such as gender, age, etc. Fourth, we identified BMI as a risk factor of contra-lateral hip factor but we were not able to precisely determine if it was the BMI or the weight loss secondary to the first fracture that was a risk factor of the contra-lateral fracture. In fact, the relationship between the loss of weight and the risk of hip fracture remains unknown. However, according to the association between decrease of skin thickness and decrease of BMI in patients with fractures, the loss of weight may be the main risk factor for contra-lateral hip fracture. In fact, a low BMI without decrease of skin thickness is not a real risk of fracture and an increase of weight could lower the risk of contra-lateral hip fracture. However, we did not have enough data to conclude on these points, even if we found a trend that skin thickness could be a better predictive tool than BMI for contra-lateral hip fracture.
In conclusion, this study assessed both BMI and skin thickness as risk factors for hip fractures in general, and contra-lateral hip fracture in particular. We confirmed their hip fracture predictive ability. These findings support the use of BMI and skin thickness as screening tools in a population with a first hip fracture in order to identify the patients with a higher risk of contra-lateral hip fracture. When combined, these two risk factors seem to identify even more precisely women at risk for contra-lateral hip fracture. This screening process could concentrate prevention on patients with a higher risk. This could lower prevention treatment costs and side effects of unnecessary prevention.
References
Müller F, Galler M, Zellner M et al (2015) The fate of proximal femoral fractures in the 10th decade of life: an analysis of 117 consecutive patients. Injury 46:1983–1987. doi:10.1016/j.injury.2015.06.048
Skála-Rosenbaum J, Džupa V, Bartoška R et al (2015) Subsequent contralateral hip fractures: can at-risk patients be identified? An observational study of 5,102 patients. Int Orthop 39:755–760. doi:10.1007/s00264-014-2646-x
Burgers PTPW, Zielinski SM, Mailuhu AKE et al (2014) Cumulative incidence and treatment of non-simultaneous bilateral femoral neck fractures in a cohort of one thousand two hundred and fifty patients. Int Orthop 38:2335–2342. doi:10.1007/s00264-014-2447-2
Kok LM, van der Steenhoven TJ, Nelissen RGHH (2010) A retrospective analysis of bilateral fractures over sixteen years: localisation and variation in treatment of second hip fractures. Int Orthop 35:1545–1551. doi:10.1007/s00264-010-1176-4
Dinah AF (2002) Sequential hip fractures in elderly patients. Injury 33:393–394
Schrøder HM, Petersen KK, Erlandsen M (1993) Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res 166–169
Hooven FH, Adachi JD, Adami S et al (2009) The global longitudinal study of osteoporosis in women (GLOW): rationale and study design. Osteoporos Int 20:1107–1116. doi:10.1007/s00198-009-0958-2
Michelotti J, Clark J (1999) Femoral neck length and hip fracture risk. J Bone Miner Res 14:1714–1720. doi:10.1359/jbmr.1999.14.10.1714
Giannini S, Luciani D, Chiarello E et al (2011) Osteosynthetic improvement of osteoporotic bone: prevention surgery. Clin Case Miner Bone Metab 8:51–54
Whitmore SE, Levine MA (1998) Risk factors for reduced skin thickness and bone density: possible clues regarding pathophysiology, prevention, and treatment. J Am Acad Dermatol 38:248–255. doi:10.1016/S0190-9622(98)70600-0
Yoneda Pde P, Biancolin SE, Gomes MSM, Miot HA (2011) Association between skin thickness and bone density in adult women. An Bras Dermatol 86:878–884. doi:10.1590/S0365-05962011000500003
Cagle PE, Dyson M, Gajewski B, Lukert B (2007) Can dermal thickness measured by ultrasound biomicroscopy assist in determining osteoporosis risk? Skin Res Technol 13:95–100. doi:10.1111/j.1600-0846.2007.00198.x
Patel R, Blake GM, Fogelman I (2007) Evaluation of osteoporosis using skin thickness measurements. Calcif Tissue Int 81:442–449. doi:10.1007/s00223-007-9081-6
Piérard GE, Piérard-Franchimont C, Vanderplaetsen S et al (2001) Relationship between bone mass density and tensile strength of the skin in women. Eur J Clin Investig 31:731–735
ORME SM, BELCHETZ PE (1994) Is a low skinfold thickness an indicator of osteoporosis. Clin Endocrinol 41:283–287. doi:10.1111/j.1365-2265.1994.tb02546.x
Chappard D, Alexandre C, Robert JM, Riffat G (1991) Relationships between bone and skin atrophies during aging. Acta Anat (Basel) 141:239–244
Brincat M, Kabalan S, STUDD JWW et al (1987) A study of the decrease of skin collagen content, skin thickness, and bone mass in the postmenopausal woman. Obstet Gynecol 70:840
Kanis JA, Johansson H, Oden A, McCloskey EV (2011) Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int 22:809–816. doi:10.1007/s00198-010-1524-7
Kim YM, Kim SH, Kim S et al (2016) Variations in fat mass contribution to bone mineral density by gender, age, and body mass index: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008–2011. Osteoporos Int 27:2543–2554. doi:10.1007/s00198-016-3566-y
Tang X, Liu G, Kang J et al (2013) Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLoS ONE 8:e55077. doi:10.1371/journal.pone.0055077
Bouxsein ML, Szulc P, Munoz F et al (2007) Contribution of trochanteric soft tissues to fall force estimates, the factor of risk, and prediction of hip fracture risk. J Bone Miner Res 22:825–831. doi:10.1359/jbmr.070309
Black MM, Bottoms E, Shuster S (1971) Skin collagen and thickness in simple obesity. Br Med J 4:149–150
Acknowledgments
The authors would like to thank Pr Philippe Hernigou for his constant help and support during the conduction of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Aurégan, JC., Frison, A., Bégué, T. et al. Contra-lateral hip fracture in the elderly: are decreased body mass index and skin thickness predictive factors?. International Orthopaedics (SICOT) 41, 247–252 (2017). https://doi.org/10.1007/s00264-016-3264-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3264-6