Abstract
Purpose
Rotational alignment of prosthetic components after total knee arthroplasty (TKA) is predominantly monitored with computer tomography (CT), for example by relating the anatomical transepicondylar axis (a-TEA) of the native femur to the posterior bicondylar axis of the prosthetic component (PBCA). The purpose of the present study was to portray a reliable, novel plain radiographic method that likewise enables the evaluation of rotational positioning of prosthetic components in TKA. Furthermore, it was intended to evaluate the prosthetic femoro-tibial functional behavior under loaded conditions.
Methods
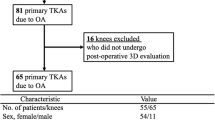
Modified plain axial radiographs under partial weight bearing (20 kg) were performed in 63 patients (63 knees) after TKA. On the obtained radiographs, all established, relevant anatomic, and prosthetic axis and angles reflecting the rotational position of the femoral (i.e., a-TEA/PBCA angle) and tibial component were detected twice by two independent examiners with an interval of one month. Additionally, in 14 cases with anterior knee pain after surgery, radiographic results were compared to obtained computer tomography images; intraclass coefficients (ICC’s) for intra- and inter-rater reliability were calculated.
Results
All pre-assigned axis and angles could be identified doubtlessly by both examiners in all investigated knees. For all measurements, ICC’s for intra-rater and inter-rater reliability ranged from 0.75 to 0.96. The comparison of the radiographic measurements with corresponding CT results (n = 14) revealed no significant differences (p > 0.05). Rotational alignment of the tibial tray in relation to the native tibial bone was not measurable due to display overlaying. Femoro-tibial behaviour of the prosthetic components under partial loading showed a high variability.
Conclusion
We were able to establish a new reliable radiographic technique that is able to show the most established and relevant anatomic landmarks and prosthetic axis after TKA to assess the rotational alignment of the prosthetic components in TKA in relation to the distal femur. The evaluation of the femoro-tibal behaviour instead shows a high variability and so far does not allow valid explanatory conclusions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Performing total knee arthroplasty (TKA) is a successful and common approach to treat severe and painful degenerative or post-traumatic osteoarthrosis of the knee. TKA can help to restore the resilience of the knee joint, relieve a patient’s pain and thus improve his mobility [1, 2]. However, one downside of TKA is the incidence of anterior knee pain, which has been reported to occur in up to 20-30 % of operated patients [2–5]. Thus, to ensure optimal knee kinematics in order to achieve the named amendments a correct rotational alignment of the prosthetic components in TKA is an indispensable keystone [6].
Possible causes for post-operative impairment are still controversial, but may often be due to a malrotation of the TKA components in relation to the anatomy of the distal femur, which is described to possibly result in subsequent paradoxal knee kinematics [5–13]. Certain authors have suggested that the rotational position of the femoral component in relation to the distal native femur, has a direct biomechanical influence regarding knee stability and patellofemoral kinematics [14–20]. Furthermore, it is described that the rotational alignment of the tibial component may have great influence on rotational stability and patellar tracking [21, 22].
Despite this clinical significance, beyond the known standard radiological projections (orthogonal X-ray, patella tangential and leg axis projections), a post-operative plain radiographic assessment of the rotational aspect of TKA has not yet gained widespread acceptance [23]. Mainly causative for this lack of popularity are reported difficulties to identify relevant bony landmarks properly [24]. Consequently, CT-scan is still presumed to be the actual gold standard to determine or exclude malrotation of the femoral and tibial components [7, 24, 25]. However, some reports likewise describe difficulties detecting all relevant bony landmarks in some cases [7, 23, 26]. Apart from that, CT-evaluation causes a higher radiation exposure, costs and may not always be available [7, 21, 26, 27].
Few individual studies so far describe plain radiographic methods only to determine the distal femur torsion (DFT) in osteoarthritic knees with axial radiographs in a patient with a flexed knee either kneeling [28] or seated [7, 23]. To our knowledge, only two investigations tried to replicate rotational alignment of TKA with plain radiography [7, 24]. Despite that all authors agree on promising results, the reproducibility and practicability of their method was only suitable for patients that were able to either kneel or flex their knee to 90°, and thus may not always be applicable directly post-operatively.
Therefore, the objective of the present study was to develop a new and easily feasible radiographic projection after TKA, which initially enables a reliable determination of the important rotational alignment of the femoral component. Furthermore, replicating a partially loaded situation in all patients intended to get an impression of the femoro-tibial flexion behavior of the prosthetic components by quantifying a conceivable lateral femoral rollback.
Materials and methods
This retrospective preliminary trial was conducted in 63 patients (63 knees) after total knee arthroplasty between March and October 2014. Except for meeting the following inclusion and exclusion criteria, no specific time frame for inclusion was purported.
Only inclusion criteria for the intended radiographic projection were: to have obtained a primary unconstrained TKA, to have given informed written consent to participate in the study and to be able to flex the knee to at least 70° at the time of investigation.
Exclusion criteria were: cases of revision TKA, having obtained a hinged TKA or an already pre-operatively detected severe osteoarthritic deformation of the knee joint.
In the final cohort we included 32 women and 31 men with a mean age of 70 years (SD ± 12, range: 44–89 years). All patients had previously underwent TKA for severe degenerative or post-traumatic osteorthrosis of the knee. A total of three different prosthesis designs were implanted. All three implanted prosthesis were unconstrained posterior cruciate retaining types: 45 Depuy PFC® (DePuy Synthes Joint Reconstruction, Warsaw, IN, USA), 11 Attune® (DePuy Synthes Joint Reconstruction, Warsaw, IN, USA) and seven ConforMIS ITotal® (ConforMIS, Bedford, MA, USA). Regarding the study goal there was no relevant difference in the specific design of the three different prosthesis.
All surgical procedures were performed by the same experienced senior surgeon (and co-author Beckmann J) using the standardized surgical protocol required by the particular type of prosthesis.
Direct post-operatively or whilst regular post-operative follow up after six weeks (depending on the patients capability to adequately flex his knee), a modified axial radiographic patella projection was performed according to the methods previously described especially by Laurin [29], Knutson [30], Takai [28] and Kanekasu [24].
The patients lay in decubiti supine position with 60 to 70 degrees of knee flexion, both feet positioned on a weight scale (Fig. 1). After positioning in a correct manner, the scale was gauged to zero in all patients to disregard the leg weight before replicating a loaded situation. Corresponding to the technique of Laurin et al. [29], during radiographic projection the patient was asked to hold the radiographic film vertically. In addition, all patients were requested to put load exclusively on the operated limb by performing a single leg press of 20 kilograms against the scale.
In 14 patients of the chosen cohort complaining about anterior knee pain CT-scans were obtained to determine the rotational alignment of the prosthetic components in relation to the native femur and tibia using the 3-dimensional helical CT system. Here, the patients were placed supine with the knees in full extension on the CT scanner. The CT was taken vertical to the long axis of the femur and tibia. Continuous 5 mm images were obtained, and the rotational alignment position of the prostheses components in relation to the distal femur was measured, using a single slice in which both epicondyles were identified most clearly.
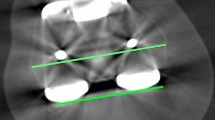
Using a DICOM image processor software (Osirix 7.0, Pixmeo SARL, Bernex, Switzerland) prosthetic positioning on the obtained radiographs (Fig. 2) as well as on the CT-scans (Fig. 3) was then assessed as follows:
-
1.
Femoral component
-
a)
The transepicondylar axis (TEA) was determined as described by Berger et al. [31]. Here, the anatomical TEA (a-TEA) reflects a line connecting the tip of the lateral epicondyle to the medial epicondylar ridge. The surgical TEA (s-TEA) runs between the lateral epicondyle and the medial epicondylar sulcus (Fig. 4).
Fig. 4 Subsequently, the particular two angles between the posterior bicondylar axis (PBCA) of the femoral component (PBCf-TKA) [21] and the anatomical and the surgical TEA respectively (Fig. 2) could be calculated—the anatomical posterior bicondylar angle (a-PBCA) and the surgical posterior bicondylar angle respectively (s-PBCA).
-
a)
-
2.
Tibial tray assessment:
-
a)
Corresponding to Berhouet et al. [21], we determined the angle between the a-TEA and the posterior marginal axis of the tibial prosthesis (PMAt-TKA), which reflect the rotation given to the tibial component with respect to the native femur (Fig. 2), named the a-TEA/PMAt-TKA angle.
-
b)
The angle between the posterior bicondylar axis of the femoral component (PBCf-TKA) and the posterior marginal axis of the tibial prosthesis (PMAt-TKA), which represents the rotational alignment of the tibial baseplate relative to the femoral component (Fig. 3) (PBCf-TKA/PMAt-TKA angle). According to Berhouet et al. [21] angle measurements were given the “—” sign when the tibial component was laterally rotated anteriorly relative to the femoral component (physiological femoral rollback) and the “+” sign otherwise (paradoxal femoral rollback).
-
a)
Coupled analysis of desired measurements and results were performed using SPSS software, version 23.0 (IBM SPSS Statistics, Ehningen, IBM Deutschland GmbH).
In order to assess our method’s reproducibility, the fundamental assessment of the most relevant a-PBCA and the s-PBCA were performed independently by two non-operator examiners (examiner 1: E1, examiner 2: E2). Both observers were blinded to any previous measurements at the time. Furthermore one examiner (E1) repeated the measurements of the a-PBCA, the s-PBCA, CT a-PBCA and the CT s-PBCA with an interval of one month (time of first assessment: T1, time of second assessment: T2).
Intraclass correlation coefficients (ICC) were calculated for inter-observer reliability (E1 versus E2) and intra-observer reliability (T1 versus T2) using SPSS software, version 23.0 (IBM SPSS Statistics, Ehningen, IBM Deutschland GmbH).
In order to get an impression of the validity of our radiographic projection, in 14 patients the particular measurements of the a-PBCA (Corr. - a-PBCA) and the s-PBCA (Corr. - s-PBCA) on our plain radiographic images were compared wih the particular CT a-PBCA and the CT s-PBCA of the same patients.
All patients gave their written and informed consent to participate in this study. The study was approved by the corresponding ethical review board (Approval number F-2014.047 - Ethics-committee Landesärztekammer Baden-Württemberg).
Results
On all 63 obtained radiographs the relevant anatomic landmarks as well as the prosthetic components, or their margins respectively, were clearly identifiable, allowing the measurement of all previously described axes and angles by both examiners.
Angle measurements
The mean angle between the anatomical transepicondylar axis and the posterior bicondylar axis (a-PBCA) was 3.2° (SD ± 1.8), the correspondent angle with respect to the surgical transepicondylar axis (s -PBCA) revealed 2.5° (SD ± 1.6). The mean a-TEA/PMAt-TKA angle, reflecting the rotational positioning of the tibial tray in relation to the native femur revealed 2.1° (SD ± 1.7). All values are summarized in Table 1.
Appropriate measurements in the CT control group (n = 14) showed 4.0° (SD ± 1.9) for the a-PBCA and 2.9° (SD ± 1.3) for the s-PBCA. No significant differences for the particular angles were detected between the corresponding 14 conventional radiographs (Corr.- a-PBCA: 3.7 (±1.8); Corr.- s –PBCA: 2.5 (±1.5)) and the named CT values ((p > 0.05) (Fig. 5).
The mean rotational relation between the femoral and the tibial component (PBCf-TKA/PMAt-TKA angle) was −1.2° (SD ±2.7). The obtained measurements did not show a normal distribution. The high variability of all single values of femoro-tibial rotational behaviour is shown in Fig. 6.
Reliability testing
Reproducibility assessing the rotational position of the femoral component (a-PBCA, s-PBCA, CT a-PBCA and CT s-PBCA) revealed an intrarater reliability between 0.77 (a-PBCA) and 0.96 (CT a-PBCA). ICC Inter-rater reliabilities assessing femoral rotational alignment was 0.83 for the a-PBCA and 0.75 for the s-PBCA. All reliability values are shown in Table 2.
Discussion
Post-operative pain and functional impairment after total knee arthroplasty is attributed to be strongly related to the rotational alignment of the prosthesis in relation to the anatomic native situation of the femur and tibia, and here especially its femoral component [7]. Computer tomography is commonly accepted to be the gold standard method to detect rotational deformities of the whole femur, i.e., in pre-operative planning as well as to evaluate rotational positioning of the femoral and tibial prosthetic components in relation to the distal femur and tibia post-operatively. However, CT machines are not available everywhere, and if so, waiting times, radiation exposure and costs are clearly higher than for conventional radiography [23]. Previous radiographic evaluation to assess rotational positioning after TKA has been inconsistently described, hence it has not yet earned widespread acceptance [23, 24].
With the presented method we were able to implement a reliable, accurate, plain radiographic projection whose post-operative performance in case of suspected femoral prosthesis component malrotation could easily be enabled in any hospital or medical practice. By means of the above named method, most relevant and scientifically established axis and angles [21] of the rotational position of the femoral component as well as the femoro-tibial behaviour under partial load can be detected.
Determining rotational aspects of the distal femur (DFT) or the femoral prosthetic component by standard radiographs has been previously described [7, 23, 24, 28]. Takai et al. [28] reported their posterior-anterior kneeling view to determine distal femur rotation of the native femur in 39 osteoarthritic and 19 normal knees. Furthermore, they addressed the transepicondylar axis, the posterior bicondylar line and the resulting angles and confirmed a significant correlation between this radiographic technique and CT images [28]. However, radiographic assessment after TKA was not performed and an 80° kneeling position was required—which is often difficult to perform in a patients’ direct post-operative period, with anterior knee pain or instability [22].
Consequently this method was modified by Kanekasu et al. [24] into an anterior-posterior axial radiograph in 32 patients (50 knees) after total knee arthroplasty in a sitting position with 90° flexed knees. In a recent sequel Viel et al. [23] performed the “seated AP view” in 79 patients (125 knees) to determine the DFT. Even though it also required a 90° knee flexion, such a sitting position is more feasible to obtain early after surgical procedures, in patients with pain, obesity or advanced age [23].
Either way, determining “solely” the DFT or assessing the rotation of the femoral component, both authors describing the standard radiographic seated AP view claim that their radiographic techniques for the most part revealed comparable results as computer tomography [23, 24]. On the other hand, these authors also limited this comparison due to difficulties identifying the medial sulcus and the surgical epicondylar axis (s-TEA). Deductively, Kanekasu et al. [24] did not use the s-TEA upon which Viel et al. [23] limited their good reliabilities for the anatomical posterior bicondylar angle, but not for the surgical posterior bicondylar angle.
Just recently Savin et al. [7] presented promising results after correlating pre-operative radiological DFT measurements with post-operative controls using the same radiological seated view in 20 patients before and after TKA. They also encourage further use of rotational radiological assessment in TKA in order to increase accuracy of prosthetic positioning [7].
Intra-observer and inter-observer reliability of the presented study was good to very good for all angles, both employing the a-TEA or the s-TEA respectively.
Nevertheless, comparing our a-PBCA with the appropriate mean twist angle on seated AP radiographs by Kanekasu et al. [24], our measurements reveal a slightly lower internal rotation of the femoral component (3.2° ± 1.8° vs. 6.9° ± 1.4°). Though the optimal value of femoral rotation component still remains unclear [7, 23], several previous studies evaluating CT images describe a mean a-PBCA of about 6° and a mean s-PBCA about 3° [15, 23, 24, 28]. Therefore, previous reports suggest a femoral component rotation of 3° external to the posterior condylar axis [25], which is consistent with our results.
Compared to computer tomography no significant discrepancies between our standard radiographic projection and the gold standard CT in the investigated knees could be detected. Furthermore several studies report about difficulties and pitfalls identifying bony landmarks on CT due to metallic artifacts and osteophyte remnants [21, 23]. Our radiographic evaluation could be a straightforward and reliable alternative not being affected by these limitations. Despite the named promising results it has to be acknowledged that anatomical deviations—i.e., in post-traumatic situations of the femur or the tibia—might clearly hinder a correct assignment of bony landmarks on a plain 2D radiograph. Here, CT allows the assessment of possible rotational deformities of the complete axis and thus, still has to be accepted as the irreplaceable method of choice.
Numerous methods or landmarks intended to achieve an accurate rotational assessment of the tibial base-plate in TKA. In a recent CT based study Berhouet et al. [21] assessed and validated the tibial component positioning by measuring the angles between the a-TEA and the posterior marginal axis of the tibial component (PMAt) as well as the angle between the posterior bicondylar line and the posterior marginal axis of the tibial tray (PBCf-TKA/PMAt-TKA angle). Here, the objective was 0° ± 2°.
We were also able to determine the PBCf-TKA/PMAt-TKA angle (−1.2 ± 2.7), revealing comparable values to those found by Berhouet et al. (0.96 ± 4.53) [21]. The slightly more negative values might be due to the loaded situation, in which this interpretation needs to be done with caution, as we did not contrast our measurements to an unloaded situation. However, despite that the position of the tibial tray could not be aligned to the native tibia, at least it could be measured to a reliable reference point [21]. The partially loaded situation moreover might allow a cautious impression of the femoro-tibial behaviour in terms of lateral femoral rollback, nevertheless without an unloaded control group this interpretation is not more then hypothetical. Finally, all measurements of a femoro-tibial behaviour itself as well as a possible correlation to the occurrence of anterior knee pain revealed too high a variability, at best allowing an impression rather than revealing the possibility to draw any explanatory conclusion.
There are some limitations that decrease the studies reach. First of all the sample size to compare and validate the radiographic method with CT was comparably small to achieve a concluding scientific power. The small discrepancies between the methods in the investigated subgroup simply caused a cut down of further radiation exposure in all patients. Therefore, the presented method is a promising preliminary concept for further developments, requiring prospective trials with adequate sample size calculations based on a priori power analysis. Nonetheless, the good accordance of the presented results with previous studies suggests the straightforwardness and reliability of our method.
Secondly, the evaluation of the tibial tray is limited to some extent, as the posterior marginal border of the base plate is overlapped by the femoral component and may be difficult to identify in some cases. Moreover, the presented radiographic method does not allow a rotational relation to the native bony landmarks of the tibia. Nevertheless, the interaction of the tibial tray with the femoral component under partially loaded conditions at least might give an impression of the femoro-tibial function itself, at which this hypothesis requires further investigations with a controlled setup.
Thirdly, the radiographic projection angle is not exactly perpendicular to the femoral component which might slightly influence the results of the detected angles [32]. However, all measurements revealed similar results to previous CT and radiographic studies as well as no significant differences in between our own controls, making this discussible point negligible.
Not least, performing our technique, the patient holds the radiographic film himself. This certainly implies a source of error as the projection might not always be accurate to a degree. Here, a prospective setup might benefit from a fixed guiding system, i.e., an attached mason’s level. However as the projection is adapted to the widespread tangential projection technique by Laurin et al. [29], we would not expect severely deviating measurements using a fixed system.
Finally, in regards to the radiation exposure, our caudo-cranial projection might be questionable because of an irradiation of the genitalia. Despite several experimental attempts of our projection setup, we could not realize a practicable cranio-caudal projection allowing the same visibility of the named axis and margins. In the end, we invoked the corresponding standardized methods of Laurin et al. [29] and Koike et al. [33], also using a caudo-cranial projection.
Overall, the presented new radiographic technique is an easy, reproducible and promising method that is able to clearly show the most relevant anatomic landmarks in order to assess the rotational alignment of the prosthesis components. The results by this radiographic view could be obtained with accuracy comparable to that of CT.
Furthermore, we were able to simulate a partially loaded situation which allowed a cautious assessment of the kinematic behavior of the operated knee joint as a complete biomechanical construct. Nonetheless, our promising results need to be interpreted with caution due to the above named limiting flaws. For practical reasons a consistent team of radiologists performing this new technique might even enhance the accuracy of measurable output.
References
Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB (2005) Does total knee replacement retsore normal knee function. Clin Orthop Relat Res 431:157–165
Petersen W, Rembitzki IV, Brüggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38(2):319–328
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Michalik R, Rath B, Springorum HR, Luering C, Tingart M (2016) Anterior knee pain after total knee arthroplasty: causes diagnosis and treatment. Orthopaede, Apr 28
Armstrong AD, Brien HJ, Dunning CE, King GJ, Johnson JA, Chess DG (2003) Patellar position after total knee arthroplasty: Influence of femoral component malposition. J Arthroplasty 18(4):458–465
Matsuzaki T, Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2013) Kinematic factors affecting postoperative knee flexion after cruciate-retaining total knee arthroplasty. Int Orthop 37(5):803–808
Savin L, Botez P, Mihailescu D, Predescu V, Grierosu C (2016) Pre-operative radiological measurement of femoral rotation for prosthetic positioning in total knee arthroplasty. Int Orthop, 2016 Jan 23
Konno T, Onodera T, Nishio Y, Kasahara Y, Iwasaki N, Majima T (2014) Correlation between knee kinematics and patellofemoral contact pressure in total knee arthroplasty. J Arthroplasty 29(12):2305–2308
Jilani A, Shirazi-Adl A, Bendjaballah M (1997) Biomechanics of human tibio-femoral joint in axial rotation. Knee 19:203–213
Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MA (2004) Does the femur roll-back with flexion? J Bone Joint Surg (Br) 86(6):925–931
Churchill D, Incavo SJ, Johnson CC, Beynnon DD (2001) The influence of femoral rollback on patellofemoral contact loads in total knee arthroplasty. J Arthroplasty 16(7):909–918
Freeman MA, Pinskerova V (2003) The movement of the knee studied by magnetic resonance imaging. Clin Orthop Relat Res 410:35–43
Johal P, Williams A, Wragg P, Hunt D, Gedroyc W (2005) Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech 38(2):269–276
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Eisenhuth SA, Saleh KJ, Cui Q, Clark CR, Brown TE (2006) Patellofemoral instability after total knee arthroplasty. Clin Orthop Relat Res 446:149–160
Briard JL, Hungerford DS (1989) Patellofemoral instability in total knee arthroplasty. J Arthroplasty 4(Suppl):S87–S97
Asano T, Akagi M, Koike K, Nakamura T (2003) Clin Orthop Relat Res 413:222–232
Abadie P, Galaud B, Michaut M, Fallet L, Boisrenoult P, Beaufils P (2009) Distal femur rotational alignment and patellar subluxation: a CT scan in vivo assessment. Orthop Traumatol Surg Res 95(4):267–271
Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N (2011) Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res 97(7):699–704
Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T (2007) Determining the rotational alignment of the tibial component at total knee replacement. J Bone Joint Surg (Br) 89:45–49
Viel T, Casin S, Ducellier F, Setiger V, Bigorre N, Bizot P (2013) Is radiographic measurement of distal femoral torsion reliable. Orthop Traumatol Surg Res 99:517–522
Kanekasu K, Kondo M, Kadoya Y (2005) Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 434:193–197
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg (Br) 93(5):629–633
Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J (2009) A common reference frame for describing rotation of the distal femur. A CT-based kinematic study unsing cadavers. J Bone Joint Surg (Br) 91:683–690
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5):365–372
Takai S, Yoshino N, Isshiki T, Hirasawa Y (2003) Kneeling view: new roentgenographic technique to assess rotational deformity and alignment of the distal femur. J Arthroplasty 18:478–483
Laurin C, Dussault R (1979) The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res 144:16–26
Knutson F (1941) Ueber die rontgenologie des femoropatellargelenkes sowie eine gute Projektion fur das Kniegelenk. Acta Radiol 22:371–376
Berger R, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Saramah SS, Patel S, Hossain FS, Haddad FS (2012) The radiological assessment of total and unicompartmental knee replacements. J Bone Joint Surg (Br) 94(10):1321–1329
Koike M, Nose H, Takagi S, Akimoto A, Kaji T (2015) A skyline-view imaging technique for axial projection of the patella: a clinical study. Radiol Phys Technol 8(2):174–177
Acknowledgments
The results of the present study represent a substantial content of the underlying doctoral thesis of the author Pedraza W.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedraza, W., Beckmann, J., Mayer, C. et al. Partially loaded plain radiographic measurement to evaluate rotational alignment in total knee arthroplasty. International Orthopaedics (SICOT) 40, 2519–2526 (2016). https://doi.org/10.1007/s00264-016-3247-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3247-7









 )
)