Abstract
Purpose
The aim of this study was to assess the effectiveness of reverse total shoulder arthroplasty (RTSA) with an all-polyethylene glenosphere in patients with failed hemiarthroplasty (HH) or the sequelae of proximal humeral fractures.
Methods
Thirty-six patients were assessed at a mean follow-up of 36 months using clinical scores and recording shoulder range of movement (ROM).
Results
Active anterior elevation (p < 0.001), lateral elevation (p < 0.001) and internal rotation (p < 0.0001) improved significantly, whereas improvement in external rotation was not significant. The mean Constant score rose significantly from 8.5 ± 7.6 to 40.7 ± 15.7 (p < 0.001) and the Simple Shoulder Test score from 0.42 ± 0.85 to 5.5 ± 2.6 (p < 0.001). Pain improved significantly from 8.7 ± 0.9 to 2.3 ± 1.2 (p < 0.001). Implant radiographic survivorship was 84.6 %. Scapular notching was detected in 7/36 patients (17.5 %). There were five complications: one (stiffness) among patients with fracture sequelae and four among those with failed HH (instability, n = 2; humeral component disassembly, n = 1; pain, n = 1). The two groups did not exhibit significant differences in pain, clinical scores or ROM.
Discussion
RTSA with an all-polyethylene glenosphere may have the potential to reduce the risk of biological notching due to polyethylene osteolysis. Further long-term studies are required to assess its efficacy.
Conclusions
The good clinical performance and reasonable rate of notching of the polyethylene glenosphere support its use in primary and revision shoulder arthroplasty.
Level of evidence: Level 4, retrospective therapeutic case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After the first report of reverse total shoulder arthroplasty (RTSA) for cuff-tear arthropathy (CTA) [1], its indications have been expanded to the revision setting to treat patients with failed anatomical prostheses and the sequelae of proximal humeral fractures (PHF) [1–6]. Despite continuously improving outcomes, primary and revision RTSA have been shown to be associated with the development of scapular notching [7]. Notching can be progressive and has the potential to induce implant failure due to loosening of the glenoid component [7].
Glenosphere design, positioning, diameter, and tilt are important predictors of post-operative scapular notching [7, 8]. Eccentricity and inferior placement of the glenosphere have been shown to improve shoulder adduction and may therefore reduce the risk of scapular notching. Lateralised offset has lowered the rate of scapular notching compared with medialised prostheses but has been associated with higher glenoid loosening rates and the need for revision surgery [7]. Most clinical studies assessing the effects of changes in geometry and positioning of prosthetic components on RTSA outcomes have regarded implants with a metal glenosphere [5, 8]. However, a 2012 biomechanical study exploring the effects of inverted bearing materials has shown that the polyethylene abrasion produced by mechanical notching in the configuration with a polyethylene inlay was significantly higher than that found with the metal inlay [9]. A recent two year prospective study using a polyethylene glenosphere in a group largely consisting of CTA patients showed good improvement in clinical scores and 20.5 % notching [10]; however, the authors did not specify the grade of notching in those with revised arthroplasty or the sequelae of PHF. To the best of our knowledge, the outcomes of revision RTSA with an eccentric all-polyethylene glenosphere have never been reported. This study was undertaken to describe the early clinical and radiological outcomes of RTSA using a 44-mm all-polyethylene glenosphere in treating patients with failed hemiarthroplasty (HH) and the sequelae of PHF.
Materials and methods
Study population
All 36 patients who underwent RTSA with an all-polyethylene glenosphere at our institution between June 2011 and October 2013 were available to be enrolled in the study, which was approved by the institutional review board (Prot. no. 2964/2014 1.5/20). All had a minimum follow-up of 24 months. Demographics and preoperative diagnosis are reported in Table 1. There were two pre-operative diagnoses: failed HH for PHF (failed HH group) and the sequelae of PHF (PHF sequelae group); the latter had initially been treated with internal fixation (n = 8) or closed fixation with K wires (n = 5). Mean follow-up duration was 38 months in the failed HH group and 31 months in patients with PHF sequelae. Mean interval from the primary procedure to revision RTSA was 22 (range 9–26) months. Three patients (one with failed HH for four-fragment PHF and two with closed fixation using K wires) had had deep infection after the primary operation and were treated with a two-stage procedure; six patients with failed HH required a bone allograft for glenoid augmentation.
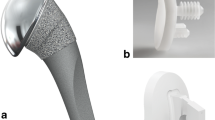
Implant design
A modular reverse shoulder prosthesis with a 44-mm, eccentric, high molecular weight all-polyethylene glenosphere (Lima, San Daniele del Friuli, Italy) was implanted in all patients (Fig. 1). Its glenoid baseplate has a superior to inferior length of 28 mm and a central peg that comes in three sizes (short, medium and long) fixed with two 6.5-mm variable-angle screws. The metal Morse taper is placed superior to the geometric spherical centre and has an inferiorised centre of rotation due to a 2-mm eccentric attachment (as opposed to the 4-mm eccentric attachment of the 36-mm eccentric glenosphere). The biomechanical features of the glenosphere are described in Fig. 2. The humeral component has a shaft-neck angle of 155° and consists of a hydroxyapatite-coated humeral body connected to the stem by means of a Morse taper and a cobalt/chromium/molybdenum (CoCrMo) alloy liner. The stem is available in three diameters (11–24 mm) and lengths (80, 150 and 180 mm). These features provide a highly versatile device that permits several matching options (between humeral body and stem), including inlays of different sizes and materials (metal, polyethylene and ceramic). Moreover, the baseplate is provided with a long trabecular titanium (TT) peg (Axioma™) that is very useful in the revision setting.
Biomechanical features of Lima reverse shoulder prosthesis with an eccentric, 44-mm, all-polyethylene glenosphere. D Glenosphere diameter; E eccentric glenosphere centre of rotation compared with the metal back axis; L lateralisation of the glenosphere centre of rotation with respect to the glenoid surface
Pre-operative radiological analysis
Pre-operative radiological analysis was with anteroposterior Grashey, Y lateral and axillary views. Glenoid bone loss, humeral bone loss and implant loosening and instability were assessed by established criteria [4, 11–13]. A case of failed and painful HH is described in Fig. 3. Fracture sequelae were classified using the criteria proposed by Boileau et al. [14]. Figure 4 describes one type of fracture sequelae. Computed tomography (CT) scan was performed to quantify glenoid bone loss [15] and to assess proximal humeral morphology in patients with PHF sequelae [16].
Glenoid erosion was concentric in 30 patients and eccentric (superior tilt) in six (all the latter were from the failed HH group). Glenoid bone loss was severe in six patients (17 %), moderate in 18 (50 %) and mild in 12 (33 %). All patients with severe glenoid deficiency belonged to the HH group and required an allograft for glenoid augmentation. Humeral loosening was found in two patients; average humeral bone loss was 37.8 mm (range 19–71). Superior prosthesis subluxation due to rotator cuff (RC) deficiency was seen in 16 patients (70 %) (Fig. 3) and anterior subluxation (>50 %) in two (8.7 %). PHF sequelae were type 1 (n = 9) (Fig. 4) and type 4 (n = 4).
Clinical evaluation and outcome measures
Clinical status was assessed before the procedure, at two months and at the last follow-up. Active range of motion (ROM), pain [visual analogue scale (VAS)], the Constant–Murley score (CS) [17] and the Simple Shoulder Test (SST) [18] score were evaluated. Active ROM was assessed in terms of anterior elevation (AAE), lateral elevation (ALE), external rotation (ER) with the patient standing using a goniometer and internal rotation (IR) as the ability to reach different levels of the spine with the thumb. Pain was graded from 0 to 10, where 0 was no pain. Patient satisfaction (PTSAT) was graded on a 10-point VAS scale similar to that used for pain [19]. ROM and clinical scores were separately assessed by two examiners who did not take part in the surgical procedures.
Surgical procedure
Each operation was performed by the same two surgeons (GP and GM) using a deltopectoral approach. The lesser tuberosity was osteotomised when the subscapularis was found intact, whereas tenotomy was done if it was retracted. In the HH group, when attempts to extract the stem failed, longitudinal humeral windows were made to remove the prosthesis with the cement mantle. The glenoid was then exposed, and the decision regarding the use of a bone graft was made by comparing the intra-operative findings to the pre-operative CT scans. The glenoid was reamed in neutral or slight inferior inclination, and a central hole was drilled for the central peg. The baseplate was impacted into place with or without the bone graft and secured with two screws in an attempt to position it flush to the inferior border of the glenoid fossa. When a bone graft was required, it was first secured behind the baseplate using the long TT Axioma™ peg. The all-polyethylene glenosphere was attached to the baseplate and fixed with a screw.
Thereafter, the humerus was hand reamed until a tight fit of the stem in the canal was obtained. The joint was reduced with the trial insert and assessed for stability. After achieving satisfactory tension and a good ROM with the trial stem and liner, the definitive press-fit or cemented humeral component of the appropriate size was secured in the canal. The definitive metal liner was secured in place and the joint was reduced. Patients with significant proximal humeral bone deficiency received a long stem [150 mm (no. 11) and 180 mm (no. 6)] without glenoid augmentation. The subscapularis was reattached, and the wound was closed in layers. Patients with infection were treated by a two-stage procedure using an antibiotic spacer. After surgery, the arm was immobilised in a sling for 4 weeks. Active mobilisations were allowed after one month. Strength exercises were begun after six weeks.
Post-operative radiographic analysis
Radiographs were obtained in the immediate post-operative period and at two months, as routinely performed in our unit, and at the last follow-up evaluation as per our study design. They were reviewed by two blinded raters who assessed stability, radiolucency, scapular notching, heterotopic ossifications and other possible complications [20]. Notching was graded according to the Sirveaux–Nerot classification [21] as follow:
-
Grade 0: No notching
-
Grade 1: Small notching confined to the pillar
-
Grade 2: Erosion up to inferior screw
-
Grade 3: Erosion beyond inferior screw
-
Grade 4: Erosion up to central peg and under baseplate
Statistical analysis
Differences between pre-operative and post-operative (delta) scores were assessed using the Wilcoxon signed-rank test and inter-rater agreement by Cohen’s kappa. Correlations between delta scores and variables [age, gender, body mass index (BMI), scapular notching] were evaluated with the Spearman, Mann–Whitney and Kruskal–Wallis tests. Implant survivorship was assessed with a Kaplan–Meier curve [95 % confidence interval (CI)], estimated as the cumulative probability of not requiring revision. The significance threshold was set at 0.05.
Results
Clinical assessment
A significant difference was found between pre-operative and post-operative ROM, with a mean change from baseline of 71.5° ± 39.4° for AAE (p < 0.001), 53.8° ± 35.6° for ALE (p < 0.001) and 2.7 ± 2.3 points for IR (p < 0.0001); ER also increased, but the change was not significant (Table 2). Pain improved significantly from 8.7 ± 0.9 to 2.3 ± 1.2 (p < 0.001).,CS increased from 8.5 ± 7.6 to 40.7 ± 15.7 (p < 0.001), the number of “yes” responses in the SST increased significantly from 0.42 ± 0.85 to 5.5 ± 2.6 (p < 0.001) and age, gender and BMI were not significantly associated either with post-operative clinical scores or with ROM.
The PTSAT score was 6.5 ± 1.7; 93 % of patients in the HH group and 92 % in the PHF sequelae group were satisfied or very satisfied. Two patients (one per group) who experienced infection after the first operation and were treated with a two-stage procedure were dissatisfied. Interobserver agreement for ROM and CS was satisfactory, with values of 0.81 and 0.86, respectively (Cohen’s kappa).
Clinical outcomes stratified by pre-operative diagnosis
At the last assessment, follow-up duration was 38 months in the HH group and 31 months in the PHF sequelae group. The two groups were not significantly different in age, gender, BMI, side dominance, clinical scores or ROM (Table 3).
Radiographic analysis at two months’ follow-up
Radiographs demonstrated implant stability and good positioning of all components. There were no cases of notching.
Latest radiographic follow-up
Notching was detected in 7/36 patients (17.5 %) by both raters; their grading according to the Sirveaux–Nerot classification [21] is reported in Table 4. There was no correlation among notching, clinical scores and ROM. Radiolucency (lines < 1.5 mm) was detected around the central peg and the inferior screw in eight patients (Fig. 5a–c), six of whom had received an allograft. The baseplate was placed with an inferior tilt in three cases (Fig. 6a–c). Radiolucency did not correlate with clinical scores. Heterotopic ossifications around the inferior glenoid rim were seen in three patients but did not affect functional outcome. Implant survivorship at the last follow-up was 84.6 % (range 47.3–96.3; Kaplan-Meier curve, 95 % CI).
a–c X-rays taken 24 months after revision reverse total shoulder arthroplasty for failed hemiarthroplasty. a Anteroposterior Grashey view, b outlet view, c axillary view. The severe proximal humeral bone loss required use of a long revision press-fitted humeral stem. Slight osteolysis around the central peg and the inferior screw was noted, but there were no signs of notching. The implant showed optimum stability (axillary view)
Complications
One patient with PHF sequelae had persistent stiffness but was pain free. Four complications arose in the HH group: severe anterior pain with irreparable subscapularis rupture (n = 1); implant dislocation at six months that was reduced under general anesthesia (n = 1); disassembly of the humeral component (humeral bone loss, 59 mm) at six months requiring implantation of a new humeral component and a metaphyseal spacer to improve prosthetic coupling and stability; instability at 24 months after a stroke, in which case the patient’s severe comorbidities precluded revision.
Discussion
Reverse shoulder prosthesis is a useful option to manage failed HH or the sequelae of PHF. Despite the higher complication rate of revision RTSA compared with primary implants for CTA and primary osteoarthritis with RC tears [22], the better post-operative clinical outcomes achieved in patients with severe shoulder impairment justify its judicious use [5, 23]. Poor outcomes of fractures managed by HH are related to multiple factors, such as retraction or malunion of the tuberosities [16, 24], component malpositioning or loosening [25], RC deficiency [26] and glenoid erosion [2]. Combinations of cuff deficiency, glenoid arthritis, tuberosity nonunion and proximal humeral bone loss can induce catastrophic consequences. When such conditions are complicated by infection around the prosthesis, a two-step surgical procedure may further impair shoulder function. On the other hand, patients with failed internal fixation for PHF may develop a variety of disabling sequelae, including humeral head collapse (type 1), locked dislocation or fracture-dislocation (type 2), nonunion of the surgical neck (type 3) and malunion of the tuberosities (type 4) [6]. Good clinical outcomes of RTSA have been reported in all types of sequelae [5, 23, 27], especially in the elderly, where poor bone quality, RC lesions and muscle atrophy prevent satisfactory outcomes with nonconstrained anatomical arthroplasty [28]. The development of modular systems and the exploration of new materials for the glenosphere and the inlay have the potential to improve outcomes [9]. The lower rate of abrasion found with a polyethylene glenosphere [9] has led some manufacturers to study and develop a prosthetic configuration with inverted bearing materials. This configuration, combined with inferior eccentricity of the glenosphere, is believed to reduce or even prevent biological notching; a recent study has demonstrated that an inferior eccentric glenosphere overhang >3.5 mm prevents notching [29]. Examination of retrieved humeral polyethylene components demonstrated inlay abrasion wear and metal debris in the inferior quadrant [30]. The eccentric polyethylene glenosphere assessed in this study provided good clinical outcomes with an acceptable rate of complications. These findings are consistent with published data regarding RTSA with a metal glenosphere [5, 23]. Radiographic survivorship in our patients was 84.6 %, and stratified data analysis found no correlation with pre-operative diagnosis. However, fenestration to extract the cemented humeral component clearly involves a greater risk of humeral weakening and periprosthetic infection. Another concern was proximal humeral bone loss and its effect on humeral component fixation. According to some authors, a loss >3 cm is critical for implant stability; they suggested using a monoblock stem component or a humeral bone allograft to prevent stress on the metaphyseal component [2, 3, 27]. Other options include using an implant where metal replaces the missing bone. Some researchers have obtained clinical benefit using RTSA for deficient humeral bone stock without allograft augmentation [13, 31]. In our study, a patient with bone loss >3 cm, complicated by component separation, was managed with a long press-fit modular stem (180 mm) and a metaphyseal spacer, without bone grafting, and achieved a good functional outcome with a pain-free and stable prosthesis. We do not view proximal humeral bone loss as critical for implant stability; we therefore use bone grafting in selected patients with severe diaphyseal bone loss associated with soft tissue disruption and poor deltoid tension. In addition, the large-diameter glenosphere (44 mm) implanted in all 36 patients in this study may have enhanced implant stability by increasing the joint contact area [32].
Interestingly, there was no sign of glenosphere wear or debris in the two patients who had to be reoperated on. Patients who received glenoid bone grafting showed radiolucent lines and signs of partial resorption around the graft; however, their clinical scores were in line with the mean values of the study population. These patients are (to be considered as being) at increased risk of developing notching and will require annual follow-up by standard X-rays. Wagner and coworkers [33] reported survival rates without radiographic glenoid loosening of 92 and 89 % at two and five years, respectively, in patients with revision RTSA and glenoid bone grafting, and were lower than the rates found in patients without glenoid bone grafting. However, bone grafting helped relieve pain and restore shoulder function and stability.
Our three patients with preoperative infection, who were managed by a two-step procedure, took longer to recover, but their post-operative clinical scores were comparable with those of the population. The outcomes of patients with PHF sequelae were good, despite the technically demanding procedure in those with a distorted proximal humeral anatomy, and are in line with those of Hussey and coworkers [34], who reported improved clinical scores and shoulder mobility after RTSA for failed internal fixation at 36 months; these authors recommend cautioning patients about the risk of complications (intra-operative and periprosthetic fracture, glenoid loosening).
The favourable clinical reports of the performance of the polyethylene glenosphere and its low risk of abrasion has led us to prefer this system in revision procedures. Glenoid notching was detected in 17.5 % of patients (15 % in the HH and 28.5 % in the PHF sequelae group) with high interrater agreement. A 2015 systematic review of the clinical and functional outcomes of RTSA reported a mean CS increase from 26.7 to 57.4 in patients with fracture sequelae (mean follow-up, 37 months) and from 21.2 to 52.8 in patients undergoing revision of anatomical prostheses (mean follow-up, 38 months) [5]. Another 2015 systematic review of the complications of RTSA described an incidence of notching of 16.8 and 28.9 % at a mean follow-up of 40 months in patients with revision of anatomical prostheses and fracture sequelae, respectively, and a 9 % rate of instability in both groups [23]. The rates of post-operative instability and notching found in our patients are in line with these data. We may speculate that a smaller amount of debris produced by a polyethylene glenosphere may help reduce the risk of notching over time, but long-term studies are clearly needed. The Australian Joint Register reports a higher rate of revision with the SMR primary reverse shoulder implant compared with other devices in the same class [35]. Although the reasons for such higher revision rates are unclear, these data concern primary implants and cannot be compared with results of the present study.
Irlenbusch and colleagues [10] described a different type of notching, with no sign of polyethylene-induced osteolysis in RTSA with inverted bearing materials and clinical results comparable with those obtained with other reverse prostheses. They reported that notching caused by metal humeral implants was found away from the baseplate, and appeared to be related to the shape of the humeral inlay. This type of notching was not found in our patients, likely due to the smooth border of the humeral inlay. Levy and coworkers found no glenoid notching in patients subjected to lateralised reverse arthroplasty and proximal humeral allograft implantation [2], even though this system is at greater risk for glenoid loosening [23]. Alternatively, an increased humeral shell offset would contribute to reduce the risk of notching, but it would produce a slight decrease in passive internal and external rotation [36].
Conclusions
Early results of RTSA with an eccentric polyethylene glenosphere in patients with failed HH and PHF sequelae were comparable with those of standard reverse implants and are promising, but long-term radiographic investigations are needed to document the potential benefits of the small amount of abrasion found with this implant, which may increase RTSA implant survivorship. Limitations of this study include its retrospective design, the absence of a control group, the small size of the two patient groups and the short follow-up. Studies comparing standard and inverted bearing RTSA should be conducted to gain additional information that can help assess the efficacy of new materials in a well-tested prosthetic system.
References
Abdel MP, Hattrup SJ, Sperling JW et al (2013) Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J 95-B:668–672. doi:10.1302/0301-620X.95B5.30964
Levy J, Frankle M, Mighell M, Pupello D (2007) The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am 89:292–300. doi:10.2106/JBJS.E.01310
Chacon A (2009) Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am 91:119. doi:10.2106/JBJS.H.00094
Antuna SA, Sperling JW, Cofield RH, Rowland CM (2001) Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elb Surg 10:217–224. doi:10.1067/mse.2001.113961
Samitier G, Alentorn-Geli E, Torrens C, Wright TW (2015) Reverse shoulder arthroplasty. Part 1: systematic review of clinical and functional outcomes. Int J Shoulder Surg 9:24–31. doi:10.4103/0973-6042.150226
Wieser K, Borbas P, Ek ET et al (2015) Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res 473:651–660. doi:10.1007/s11999-014-3985-z
Nicholson GP, Strauss EJ, Sherman SL (2011) Scapular notching: recognition and strategies to minimize clinical impact. Clin Orthop Relat Res 469:2521–2530. doi:10.1007/s11999-010-1720-y
Berliner JL, Regalado-Magdos A, Ma CB, Feeley BT (2014) Biomechanics of reverse total shoulder arthroplasty. J Shoulder Elb Surg 24:150–160. doi:10.1016/j.jse.2014.08.003
Kohut G, Dallmann F, Irlenbusch U (2012) Wear-induced loss of mass in reversed total shoulder arthroplasty with conventional and inverted bearing materials. J Biomech 45:469–473. doi:10.1016/j.jbiomech.2011.11.055
Irlenbusch U, Kääb MJ, Kohut G et al (2015) Reversed shoulder arthroplasty with inversed bearing materials: 2-year clinical and radiographic results in 101 patients. Arch Orthop Trauma Surg 135:161–169. doi:10.1007/s00402-014-2135-0
Sperling JW, Cofield RH, O’Driscoll SW et al (2000) Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elb Surg 9:507–513
Sperling JW, Cofield RH, Rowland CM (2004) Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elb Surg 13:604–613. doi:10.1016/S1058274604001296
Budge MD, Moravek JE, Zimel MN et al (2013) Reverse total shoulder arthroplasty for the management of failed shoulder arthroplasty with proximal humeral bone loss: is allograft augmentation necessary? J Shoulder Elb Surg 22:739–744. doi:10.1016/j.jse.2012.08.008
Boileau P, Trojani C, Walch G et al (2001) Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elb Surg 10:299–308. doi:10.1067/mse.2001.115985
Merolla G, Campi F, Paladini P et al (2010) Multichannel computed tomography (MCCT) analysis of glenoid erosion in shoulder hemiarthroplasty: preliminary clinical applications. Musculoskelet Surg 94(Suppl 1):S71–S77. doi:10.1007/s12306-010-0059-6
Boileau P, Krishnan SG, Tinsi L et al (2002) Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elb Surg 11:401–412
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Godfrey J, Hamman R, Lowenstein S et al (2007) Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. J Shoulder Elb Surg 16:260–267. doi:10.1016/j.jse.2006.07.003
Harreld K, Clark R, Downes K et al (2013) Correlation of subjective and objective measures before and after shoulder arthroplasty. Orthopedics 36:808–814. doi:10.3928/01477447-20130523-29
Roberts CC, Ekelund AL, Renfree KJ et al (2007) Radiologic assessment of reverse shoulder arthroplasty. Radiographics 27:223–235. doi:10.1148/rg.271065076
Sirveaux F, Favard L, Oudet D et al (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg (Br) 86:388–395
Wall B, Nové-Josserand L, O’Connor DP et al (2007) Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 89:1476–1485. doi:10.2106/JBJS.F.00666
Alentorn-Geli E, Samitier G, Torrens C, Wright TW (2015) Reverse shoulder arthroplasty. Part 2: systematic review of reoperations, revisions, problems, and complications. Int J Shoulder Surg 9:60–67. doi:10.4103/0973-6042.154771
Robinson CM, Page RS, Hill RMF et al (2003) Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am 85-A:1215–1223
Hasan SS, Leith JM, Campbell B et al (2002) Characteristics of unsatisfactory shoulder arthroplasties. J Shoulder Elb Surg 11:431–441
Hashiguchi H, Iwashita S, Ohkubo A, Takai S (2015) The outcome of hemiarthroplasty for proximal humeral fractures is dependent on the status of the rotator cuff. Int Orthop 39:1115–1119. doi:10.1007/s00264-015-2758-y
Greiner S, Uschok S, Herrmann S et al (2014) The metaphyseal bone defect predicts outcome in reverse shoulder arthroplasty for proximal humerus fracture sequelae. Arch Orthop Trauma Surg 134:755–764. doi:10.1007/s00402-014-1980-1
Mansat P, Bonnevialle N (2015) Treatment of fracture sequelae of the proximal humerus: anatomical vs reverse shoulder prosthesis. Int Orthop 39:349–354. doi:10.1007/s00264-014-2651-0
Poon PC, Chou J, Young SW, Astley T (2014) A comparison of concentric and eccentric glenospheres in reverse shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 96:e138. doi:10.2106/JBJS.M.00941
Nam D, Kepler CK, Neviaser AS et al (2010) Reverse total shoulder arthroplasty: current concepts, results, and component wear analysis. J Bone Joint Surg Am 92(Suppl 2):23–35. doi:10.2106/JBJS.J.00769
Stephens SP, Paisley KC, Giveans MR, Wirth MA (2015) The effect of proximal humeral bone loss on revision reverse total shoulder arthroplasty. J Shoulder Elb Surg 24:1519–1526. doi:10.1016/j.jse.2015.02.020
Langohr GDG, Willing R, Medley JB et al (2015) Contact mechanics of reverse total shoulder arthroplasty during abduction: the effect of neck-shaft angle, humeral cup depth, and glenosphere diameter. J Shoulder Elb Surg. doi:10.1016/j.jse.2015.09.024
Wagner E, Houdek MT, Griffith T et al (2015) Glenoid bone-grafting in revision to a reverse total shoulder arthroplasty. J Bone Joint Surg Am 97:1653–1660. doi:10.2106/JBJS.N.00732
Hussey MM, Hussey SE, Mighell MA (2015) Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Joint J 97-B:967–972. doi:10.1302/0301-620X.97B7.35713
Khan L, Page R, Miller L, Graves S (2012) Risk factors for early revision after shoulder arthroplasty: 7113 shoulder arthroplasties from the Australian orthopaedic association national joint replacement registry. Orthop Proc 94-B:123
Tashjian RZ, Burks RT, Zhang Y, Henninger HB (2015) Reverse total shoulder arthroplasty: a biomechanical evaluation of humeral and glenosphere hardware configuration. J Shoulder Elb Surg 24:e68–e77. doi:10.1016/j.jse.2014.08.017
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merolla, G., Tartarone, A., Sperling, J.W. et al. Early clinical and radiological outcomes of reverse shoulder arthroplasty with an eccentric all-polyethylene glenosphere to treat failed hemiarthroplasty and the sequelae of proximal humeral fractures. International Orthopaedics (SICOT) 41, 141–148 (2017). https://doi.org/10.1007/s00264-016-3188-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3188-1