Abstract
Purpose
To study the clinical presentation of femoral head osteonecrosis (ONFH). Publications dedicated to this aspect of ONFH are rare. Our aim was to systematically collect and describe the clinical data.
Methods
A prospective survey was conducted in a cohort of ONFH recruited from a dedicated clinic for osteonecrosis. The history of symptoms, medical management, and physical findings were obtained from 88 patients suffering from 125 ONFH. Subgroups were formed: bilateral versus unilateral ONFH, radiological stages 1–2 (pre-fractured) versus fractured stage 3 versus stage 4.
Results
ONFH was bilateral in 63 %, especially in corticosteroid users and in sickle-cell cases. These patients were younger but had similar BMIs compared to the unilateral cases. The pain was mechanical in 79 % of hips and inflammatory in 21 %. Acute pain at the onset was present in 55 % of hips. The localization of this pain was variable, including in the groin, the buttocks, or diffused in the lower limbs. A limp was present in 50 % of the patients, only when one hip was painful. The physical examination of the hip was normal in 31 %, especially in stages 1–2 (55 %). The diagnosis delay was 12 months, with inadequate medical management in 51 % of patients.
Conclusions
In ONFH cases, no typical clinical pattern was found. The clinical presentation was very variable, sometimes having spine or knee symptoms with a normal physical examination of the hip. ONFH should be systematically suspected in cases of onset of pain in the pelvis, buttocks, groin, and lower limbs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteonecrosis of the femoral head (ONFH) can cause hip destruction in young people as well as in the elderly. Early diagnosis is, therefore, of the utmost importance to maximize therapeutic efficacy [1]. The diagnosis of osteonecrosis (ON) is based on radiological and magnetic resonance imaging criteria [2, 3]. However, the first step in diagnosis remains “clinical suspicion” [1]. A review of the available articles and textbooks provides scant data concerning the typical patterns of symptoms and/or physical examination findings in ONFH. References to these aspects of ONFH are rare and include mainly case reports, except one [4], without any systematic and quantitative study. In our reviewed references, we found that the symptoms of ONFH should be typically pain, throbbing in the groin, sometimes radiating to the knee or the buttocks [1, 2]. This pain should be often intermittent; it can also be progressive and sometimes sudden [1]. This pattern of sudden onset pain was compared with coronary symptoms or visceral infarction [5, 6]. The physical examination could be unremarkable or could include pain upon internal rotation of the hip [1, 2].
In this paper, we present a study of the data that we prospectively collected from a number of ONFH cases that were evaluated in our clinic dedicated to osteonecrosis.
Patients, methods
In our osteonecrosis clinic, 97 patients/136 non-traumatic (no fracture or joint dislocation) ONFH were recruited from 2005 to 2012. Their clinical features were systematically and prospectively collected. Complete data were available for 88 patients — 125 hips.
All of the patients signed a consent form authorizing us to use the collected data. The study was approved by the ethical committee of the Faculty of Medicine of Liège.
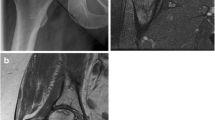
The evaluations included a systematic radiological examination (two views) together with an MR imaging study of both hips. The patients were questioned concerning their pain, (mechanical when the pain was increased by motion and improved by rest and inflammatory when increased by rest), the main areas of pain together with the spread areas, the type of onset (sudden or progressive), the presence of limp, the history of a triggering event, and the duration of symptoms as well as their medical history check-ups, follow-up care, and delay in establishing the correct diagnosis. The patients quantified their hip pain using a VAS scale from 1 (no pain) to 100 mm (worst pain) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) parts 1 (pain scoring 0–20) and 2 (stiffness scoring 0–8).
A physical examination of the hip was conducted by the same clinician (JPH) for all cases to avoid bias. The examination included local palpation and passive motion. The presence of induced pain was noted. The joint motion was measured by a hand goniometer for flexion, abduction, medial, and lateral rotations. When ONFH was unilateral, motion was compared with the normal contralateral hip and deemed reduced for a difference of minimum 10°. When ONFH was bilateral, motion was deemed reduced for a flexion of less than 110°, abduction of less than 40°, lateral rotations of less than 30° and medial rotation of less than 20° [7]. Subgroups were formed for unilateral versus bilateral ONFH using radiological staging with a modified Ficat staging: stages 1–2 for non-fractured ONFH, stage 3 when a crescent sign or a collapse was present and stage 4 when signs of osteoarthritis were present.
Statistical methods
Continuous variables were described by their means ± SEM and their minimum and maximum values. Discrete variables were described by their numbers of observations and percentages. Continuous variables were compared using ANOVA followed, in cases of statistical significance, by Tukey’s tests. Discrete variables were compared using exact Fisher’s tests. The statistical software used was IBM-SPSS V22.0. All statistical tests were stated as significant when the p-value was <0.05.
Results
The cohort included 54 males (61 %) and 34 females (39 %). The mean age was 48.4 ± 1.6 (19–83 years). The BMI was 26.0 ± 0.5 (11–36). Osteonecrosis was unilateral in 33 patients (38 %), (17 right hips, 16 left hips) and bilateral in 55 patients (63 %), with nine patients who presented with ON stage 1–2 in both hips. The stages were 1–2 in 55 hips, stage 3 in 53 hips, and stage 4 in 17 hips. In ten patients, ON was multifocal (more than 2 ON localizations). In Table 1, the age, gender, BMI, and etiological factors are presented for unilateral and bilateral hip ON with the p-values of the statistical comparisons. The etiological factors were corticosteroid use in 44 patients, ethanol abuse in 15, both in four, sickle cell disease in five, and other in seven (hyperlipemia in two, rheumatoid arthritis in one, beta thalassemia in one, trauma without neck fracture or dislocation in two, AIDS in one). No aetiological factors were found in 13 patients. In bilateral ONFH cases, patients did not show higher BMIs. Concerning the aetiological factors, corticosteroids and sickle cell were related to the bilateral form of ONFH.
Symptoms
Hips were painful in 94 patients (74 %) and painless in 31 (26 %), particularly in 49 % of the stage 1–2 hips (Table 2). All of the unilateral hips were painful. In bilateral ONFH, three were painless on both sides; they presented a multifocal ONFH with symptoms in another joint (knee in two cases, shoulder in one case). Pain was mechanical in 74 hips (79 %) (Table 2). Inflammatory pain was present in 26 cases (21 %), especially in ONFH stage 4 (41 %). The pain was localized in the groin region in 15 cases (18 %), the buttocks in 13 (15 %), in both in 23 (27 %), in the knee in 8 (9 %), and diffused in the lower limbs in 26 (31 %). Patients had a limp in 44 cases (50 %). In the unilateral cases, limping was present in 4/10 stage one to two cases, 10/15 stage three cases and 4/8 stage four cases. The three patients suffering from bilateral painless ONFH reported no limping. One crutch was needed in eight cases (9 %), two crutches in five (6 %), and a wheelchair in two cases. The onset was sudden in 42 hips (55 %) and progressive in 52 (45 %). Patients reported no triggering events in 79 cases (90 %) and a trauma (apart from fracture or joint dislocation) in nine (10 %). The duration of symptoms before the diagnosis was a mean of 12.8 ± 2.0 months (0–120). The first medical check-up concerned the hip in 43/88 cases (49 %), lumbar spine in 36 (41 %), the knee in seven (8 %), and other in two (2 %). ONFH was diagnosed after 11.0 ± 1.6 months (0–84). In 53 cases, previous radiological studies could be reviewed: in ten cases, ON features were present while the protocol did not mention the right diagnosis. The previous treatments were analgesic in 64 cases (73 %), NSAIDs in 38 (43 %), lumbar epidural injection, knee arthroscopy in two (2 %), other in three (3 %) (facet joint injections, physiotherapy, lumbar spine manipulations), and nothing in three (3 %).
Table 2 presents VAS pain, WOMAC pain, and WOMAC stiffness allocated by ONFH stage and a statistical comparison between ONFH stages 1–2 and 3, 1–2 and 4. Pain measured by VAS and WOMAC pain and stiffness evaluated by WOMAC stiffness are related to the radiological stage: lower in non-fractured stages 1–2 and increasing in stage 3.
Physical examination
The results of palpation and mobilization are presented in Table 2. A normal examination was found in 31 % of the hips. In non-fractured stage 1–2, hip physical examination was more frequently normal (55 %), with a lack of pain during palpation in 96 %, a lack of pain during mobilization in 55 %, and no joint motion limitation in 71 %. Stage 4 hips had more severe joint motion restrictions.
Discussion
Our ONFH cohort is comparable with some published cohorts in terms of the mean age and sex ratio. Older papers presented different sex ratios, with more males [4] or more females [8] in relation to the aetiological factors. The following relationships between sex ratios and some aetiological factors were recently confirmed: male predominance for ethanol abuse and female predominance for corticosteroid use [9]. In our series, bilateral ONFH lesions were more frequent than unilateral disease. This high percentage could be due to the systematic MRI evaluation of both hips. However, a higher proportion of bilateral lesions has been previously found in non-traumatic ONFH using radiological [5], histological [10], or MRI criteria [3]. The BMI was not found to play a role in terms of ONFH presence or in bilateral versus unilateral lesions. Etiological factors, such as corticosteroid use and sickle cell disease, are related to both bilateral ONFH and multifocal ON lesions.
Globally, no predominant pattern of a clinical presentation of ONFH was found in our study. Our main finding is a frequent lack of hip symptoms in ONFH.
Symptoms
Pain was only present in 51 % in the pre-fracture stages. This so-called “silent hip” has been previously described [11]. In the post-fracture stages, pain was almost always present. The pain was mainly mechanical. The osteoarthritic late changes induced more inflammatory pain, rather than more frequent pain or more severity of pain (VAS quantification). MR or ultrasonographic images should be collected to assess the relationship with synovitis. A suddenness of onset was found in 55 % of cases. Such an acute onset has been previously reported, including the mention of a so-called coronary-like presentation of ONFH [5, 6].
In ONFH, a limp was only present when at least one hip was painful. The localization of pain in ONFH is variable and can be diffuse. Such a variability of pain localization could explain the overlong delays common before ONFH diagnosis was considered as well as the inadequate medical investigations.
Physical findings
The most frequent pain reported for ONFH diagnosis was pain produced by hip mobilization. In the early stages, there was usually no movement limitation. In later stages, a reduction in movement was found more often (p = 0.001). We confirmed the predominance of the internal rotation limitation that was previously reported [1, 2]. The flexion limitation increased in the late stages.
Diagnostic management
Diagnostic management of ONFH is inadequate in many cases. The duration of symptoms (13 months) and the delay before the correct diagnosis (12 months) are very important. A previous inadequate diagnostic process (lumbar spine, knee, and others) was present in 55 % of cases. This sometimes led to inadequate therapies. ONFH is not often considered by physicians in cases of pain in the pelvis, buttocks, groin or lower limbs.
Our study is limited in that we only recruited patients referred to our clinic for cell-based therapies.
We conclude that, in ONFH, no typical pattern of clinical features was found. Our main finding in ONFH is a frequent lack of hip with sometimes presence of spine or knee symptoms. This could explain the inadequate diagnostic management of ONFH cases. Its clinical presentation is extremely variable, frequently poor, but normal in 31 % of cases. Therefore, ONFH diagnosis could be systematically suspected when the patient reports mechanical pain in the pelvis, the buttocks, the groin or the lower limbs.
References
Mont MA, Hungerford DS (1995) Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 77:459–474
Arlet J (1992) Nontraumatic avascular necrosis of the femoral head. Past, present, and future. Clin Orthop Relat Res 277:12–21
Hauzeur JP, Pasteels JL, Schoutens A, Hinsenkamp M, Appelboom T, Chochrad I, Perlmutter N (1989) The diagnostic value of magnetic resonance imaging in non-traumatic osteonecrosis of the femoral head. J Bone Joint Surg Am 71:641–649
Ficat P, Arlet J (1977) Statistical study of 136 patients suffering from non traumatic osteonecrosis of the femoral head. In: Ficat P, Arlet J (eds) Ischémie et nécrose osseuses: l’exploration fonctionnelle de la circulation intra-osseuse et ses applications. Masson, Paris, pp 87–90
Merle D’Aubigné R, Postel M, Mazabraud A, Massias P, Gueguen J, France P (1965) Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg (Br) 47:612–623
Chandler FA (2001) Coronary disease of the hip. Clin Orthop Relat Res 386:7–10
Kendall HO, Kendall FP, Wadsworth GE (1971) Hip. In: Kendall HO, Kendall FP, Wadsworth GE (eds) Muscles, testing and function. Williams & Wilkins, Baltimore, pp 25–26
Zizic TM, Marcoux C, Hungerford DS, Stevens MB (1986) The early diagnosis of ischemic necrosis of bone. Arthritis Rheum 29:1177–1186
Fukushima W, Fujioka M, Kubo T, Tamakoshi A, Nagai M, Hirota Y (2010) Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res 468:2715–2724
Hauzeur JP, Pasteels JL, Orloff S (1987) Bilateral non-traumatic aseptic osteonecrosis in the femoral head. An experimental study of incidence. J Bone Joint Surg Am 69:1221–1225
Marcus ND, Enneking WF, Massam RA (1973) The silent hip in idiopathic aseptic necrosis. Treatment by bone-grafting. J Bone Joint Surg Am 55:1351–1366
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Hauzeur, JP., Malaise, M. & de Maertelaer, V. A prospective cohort study of the clinical presentation of non-traumatic osteonecrosis of the femoral head: spine and knee symptoms as clinical presentation of hip osteonecrosis. International Orthopaedics (SICOT) 40, 1347–1351 (2016). https://doi.org/10.1007/s00264-015-3079-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3079-x